Clin Exp Otorhinolaryngol.
2023 Nov;16(4):380-387. 10.21053/ceo.2023.00689.
Ultrasound-Guided Ethanol Percutaneous Ablation Versus Rescue Surgery in Patients With Locoregional Recurrence of Papillary Thyroid Cancer
- Affiliations
-
- 1Department of Endocrinology, University Hospital Son Espases, Palma de Mallorca, Spain
- 2Department of Surgery, Section of Endocrine Surgery, University Hospital Son Espases, Palma de Mallorca, Spain
- 3Department of Maxillo-Facial Surgery, University Hospital Puerta del Mar, Cádiz, Spain
- 4Department of Nuclear Medicine, University Hospital Son Espases, Palma de Mallorca, Spain
- 5Laboratory of Clinical Analysis, University Hospital Son Espases, Palma de Mallorca, Spain
- KMID: 2548366
- DOI: http://doi.org/10.21053/ceo.2023.00689
Abstract
Objectives
Neck recurrence of papillary thyroid cancer (PTC) is frequently detected after initial surgery. The management of these lesions may include rescue surgery (RS) or minimally invasive techniques in selected patients, but comparative studies evaluating the effectiveness and safety of these techniques are lacking. In this paper, we compared ultrasound-guided ethanol ablation (EA) in selected patients to RS in a matched cohort.
Methods
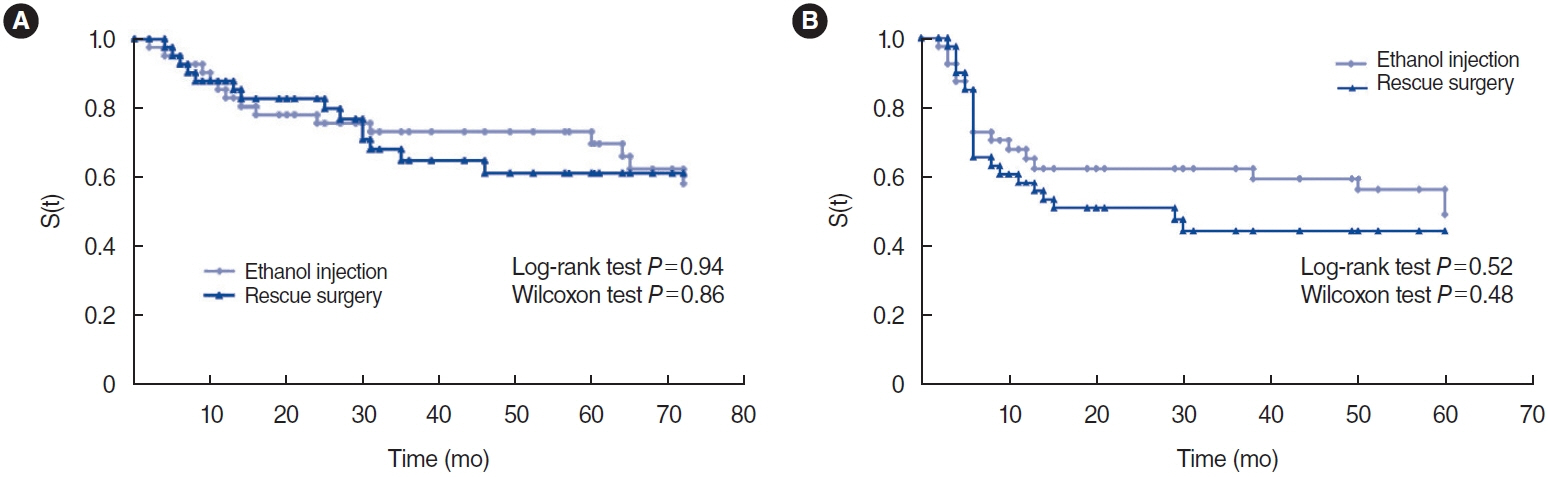
We retrospectively compared 41 patients and 41 matched PTC patients without known distant metastases, who underwent ultrasound-guided EA or RS (matched reference group), who had 63 and 75 thyroid bed and/or lymph node confirmed PTC recurrences during a median follow-up of 72.8 and 89.6 months, respectively. The primary outcome was time until structural recurrence, compared using Kaplan-Meier survival curves. The secondary outcomes included time until biochemical recurrence, plasma thyroglobulin (Tg) levels, American Thyroid Association (ATA) response-to-therapy categories by the last available observation, and treatment-derived complications in each group.
Results
No significant differences were found between the EA and RS groups for time until structural recurrence (log-rank test, P=0.94). The time until biochemical recurrence was also similar (P=0.51); and the plasma Tg concentration reduction and proportions of patients in the ATA reclassification categories were also similar. A significantly higher proportion of patients in the RS group presented treatment-derived complications (29.27% vs. 9.75%, P<0.05).
Conclusion
In this retrospective analysis, the treatment of PTC neck recurrence with EA in selected patients was comparable to RS in a matched reference group for the long-term risk of structural or biochemical relapse, but with a lower risk of treatment-derived complications. These results support the effectiveness and safety of this minimally invasive technique in the management of selected patients with recurrent PTC.
Figure
Reference
-
1. European Network of Cancer Registries (ENCR). ENCR factsheets [Internet]. ENCR; 2017 [cited 2023 Sep 1]. Available from: https://www.encr.eu/sites/default/files/factsheets/ENCR_Factsheet_Thyroid_2017-2.pdf.2. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016; Jan. 26(1):1–133.3. Urken ML, Milas M, Randolph GW, Tufano R, Bergman D, Bernet V, et al. Management of recurrent and persistent metastatic lymph nodes in well-differentiated thyroid cancer: a multifactorial decision-making guide for the Thyroid Cancer Care Collaborative. Head Neck. 2015; Apr. 37(4):605–14.4. Al-Saif O, Farrar WB, Bloomston M, Porter K, Ringel MD, Kloos RT. Long-term efficacy of lymph node reoperation for persistent papillary thyroid cancer. J Clin Endocrinol Metab. 2010; May. 95(5):2187–94.5. Uchida H, Imai T, Kikumori T, Hayashi H, Sato S, Noda S, et al. Longterm results of surgery for papillary thyroid carcinoma with local recurrence. Surg Today. 2013; Aug. 43(8):848–53.6. Roh JL, Kim JM, Park CI. Central compartment reoperation for recurrent/persistent differentiated thyroid cancer: patterns of recurrence, morbidity, and prediction of postoperative hypocalcemia. Ann Surg Oncol. 2011; May. 18(5):1312–8.7. Samaan NA, Schultz PN, Hickey RC, Goepfert H, Haynie TP, Johnston DA, et al. The results of various modalities of treatment of well differentiated thyroid carcinomas: a retrospective review of 1599 patients. J Clin Endocrinol Metab. 1992; Sep. 75(3):714–20.8. Mauri G, Hegedus L, Bandula S, Cazzato RL, Czarniecka A, Dudeck O, et al. European Thyroid Association and Cardiovascular and Interventional Radiological Society of Europe 2021 clinical practice guideline for the use of minimally invasive treatments in malignant thyroid lesions. Eur Thyroid J. 2021; Jun. 10(3):185–97.9. Hahn SY, Shin JH, Na DG, Ha EJ, Ahn HS, Lim HK, et al. Ethanol ablation of the thyroid nodules: 2018 consensus statement by the Korean Society of Thyroid Radiology. Korean J Radiol. 2019; Apr. 20(4):609–20.10. Orloff LA, Noel JE, Stack BC, Russell MD, Angelos P, Baek JH, et al. Radiofrequency ablation and related ultrasound-guided ablation technologies for treatment of benign and malignant thyroid disease: an international multidisciplinary consensus statement of the American Head and Neck Society Endocrine Surgery Section with the Asia Pacific Society of Thyroid Surgery, Associazione Medici Endocrinologi, British Association of Endocrine and Thyroid Surgeons, European Thyroid Association, Italian Society of Endocrine Surgery Units, Korean Society of Thyroid Radiology, Latin American Thyroid Society, and Thyroid Nodules Therapies Association. Head Neck. 2022; Mar. 44(3):633–60.11. Shin JE, Baek JH, Lee JH. Radiofrequency and ethanol ablation for the treatment of recurrent thyroid cancers: current status and challenges. Curr Opin Oncol. 2013; Jan. 25(1):14–9.12. Tofe S, Arguelles I, Serra G, Garcia H, Barcelo A, Pereg V. Ultrasound-guided percutaneous ethanol ablation for the management of recurrent thyroid cancer: evaluation of efficacy and impact on disease course. Int J Thyroidol. 2020; Nov. 13(2):128–41.13. Heilo A, Sigstad E, Fagerlid KH, Haskjold OI, Groholt KK, Berner A, et al. Efficacy of ultrasound-guided percutaneous ethanol injection treatment in patients with a limited number of metastatic cervical lymph nodes from papillary thyroid carcinoma. J Clin Endocrinol Metab. 2011; Sep. 96(9):2750–5.14. Lewis BD, Hay ID, Charboneau JW, McIver B, Reading CC, Goellner JR. Percutaneous ethanol injection for treatment of cervical lymph node metastases in patients with papillary thyroid carcinoma. AJR Am J Roentgenol. 2002; Mar. 178(3):699–704.15. Hay ID, Lee RA, Davidge-Pitts C, Reading CC, Charboneau JW. Longterm outcome of ultrasound-guided percutaneous ethanol ablation of selected “recurrent” neck nodal metastases in 25 patients with TNM stages III or IVA papillary thyroid carcinoma previously treated by surgery and 131I therapy. Surgery. 2013; Dec. 154(6):1448–55.16. Guenette JP, Monchik JM, Dupuy DE. Image-guided ablation of postsurgical locoregional recurrence of biopsy-proven well-differentiated thyroid carcinoma. J Vasc Interv Radiol. 2013; May. 24(5):672–9.17. Suh CH, Baek JH, Choi YJ, Lee JH. Efficacy and safety of radiofrequency and ethanol ablation for treating locally recurrent thyroid cancer: a systematic review and meta-analysis. Thyroid. 2016; Mar. 26(3):420–8.18. Fontenot TE, Deniwar A, Bhatia P, Al-Qurayshi Z, Randolph GW, Kandil E. Percutaneous ethanol injection vs reoperation for locally recurrent papillary thyroid cancer: a systematic review and pooled analysis. JAMA Otolaryngol Head Neck Surg. 2015; Jun. 141(6):512–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound (US)-Guided Ablation of Thyroid Nodules
- Non-surgical, Image-guided Management of Benign Thyroid Nodules
- Successful Endoscopic Ultrasound-Guided Alcohol Ablation of Sporadic Insulinoma Using Three-Dimensional Targeting (with Video)
- The Effect of Ethanol Ablation for the Treatment of Benign Cystic Thyroid Nodules
- Ultrasound-guided radiofrequency ablation for the treatment of papillary thyroid carcinoma: a review of the current state and future perspectives