Restor Dent Endod.
2023 May;48(2):e21. 10.5395/rde.2023.48.e21.
Effects of different calcium-silicate based materials on fracture resistance of immature permanent teeth with replacement root resorption and osteoclastogenesis
- Affiliations
-
- 1Department of Endodontics, School of Dentistry, Federal University of Uberlândia, Uberlândia, Brazil
- 2School of Dentistry, Federal University of Uberlândia, Uberlândia, Brazil
- 3Department of Operative Dentistry and Dental Materials, School of Dentistry, Federal University of Uberlândia, Uberlândia, Brazil
- KMID: 2548224
- DOI: http://doi.org/10.5395/rde.2023.48.e21
Abstract
Objectives
This study evaluated the effects of Biodentine (BD), Bio-C Repair (BCR), and mineral trioxide aggregate (MTA) plug on the fracture resistance of simulated immature teeth with replacement root resorption (RRR) and in vitro-induced osteoclastogenesis.
Materials and Methods
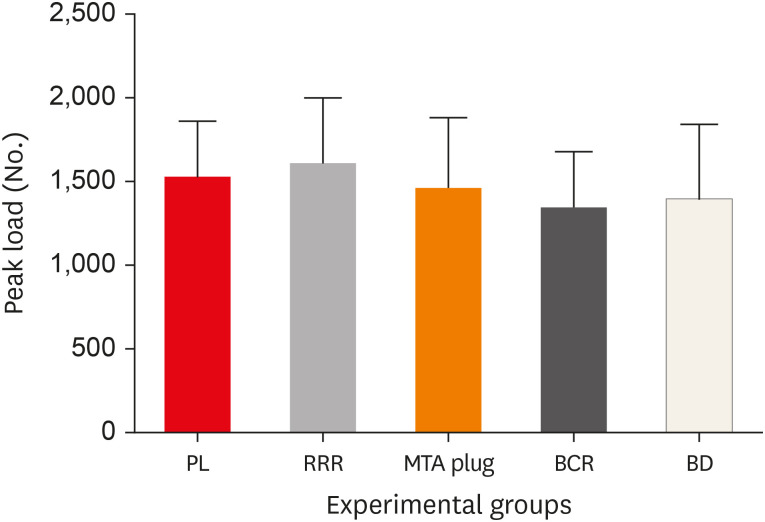
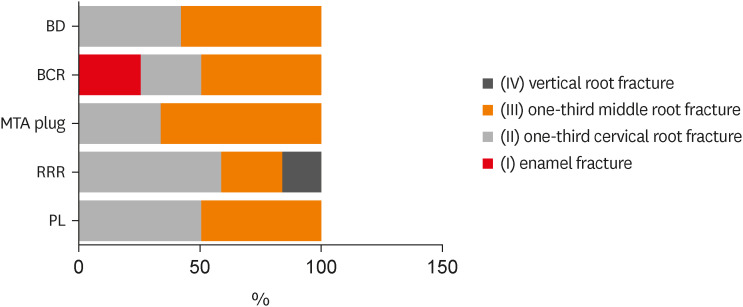
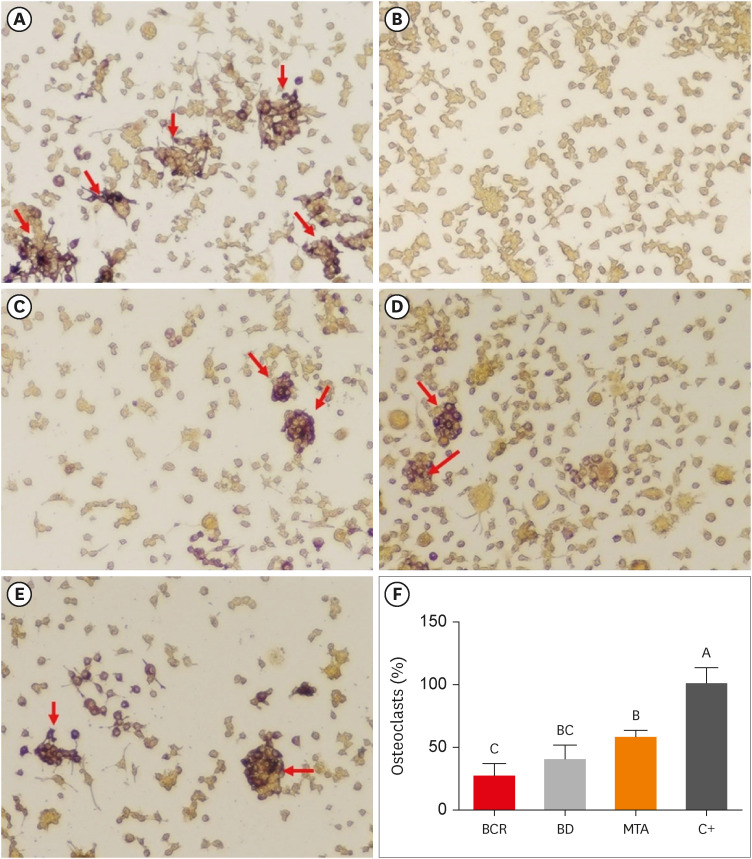
Sixty bovine incisors simulating immature teeth and RRR were divided into 5 groups: BD and BCR groups, with samples completely filled with the respective materials; MTA group, which utilized a 3-mm apical MTA plug; RRR group, which received no root canal filling; and normal periodontal ligament (PL) group, which had no RRR and no root canal filling. All the teeth underwent cycling loading, and compression strength testing was performed using a universal testing machine. RAW 264.7 macrophages were treated with 1:16 extracts of BD, BCR, and MTA containing receptor activator of nuclear factor-kappa B ligand (RANKL) for 5 days. RANKL-induced osteoclast differentiation was assessed by staining with tartrate-resistant acid phosphatase. The fracture load and osteoclast number were analyzed using 1-way ANOVA and Tukey’s test (α = 0.05).
Results
No significant difference in fracture resistance was observed among the groups (p > 0.05). All materials similarly inhibited osteoclastogenesis (p > 0.05), except for BCR, which led to a lower percentage of osteoclasts than did MTA (p < 0.0001).
Conclusions
The treatment options for non-vital immature teeth with RRR did not strengthen the teeth and promoted a similar resistance to fractures in all cases. BD, MTA, and BCR showed inhibitory effects on osteoclast differentiation, with BCR yielding improved results compared to the other materials.
Figure
Reference
-
1. Rocha Lima TF, Nagata JY, de Souza-Filho FJ, de Jesus Soares A. Post-traumatic complications of severe luxations and replanted teeth. J Contemp Dent Pract. 2015; 16:13–19. PMID: 25876944.
Article2. de Souza BD, Dutra KL, Reyes-Carmona J, Bortoluzzi EA, Kuntze MM, Teixeira CS, Porporatti AL, De Luca Canto G. Incidence of root resorption after concussion, subluxation, lateral luxation, intrusion, and extrusion: a systematic review. Clin Oral Investig. 2020; 24:1101–1111.
Article3. Galler KM, Grätz EM, Widbiller M, Buchalla W, Knüttel H. Pathophysiological mechanisms of root resorption after dental trauma: a systematic scoping review. BMC Oral Health. 2021; 21:163. PMID: 33771147.
Article4. Panzarini SR, Sonoda CK, Saito CT, Hamanaka EF, Poi WR. Delayed tooth replantation: MTA as root canal filling. Braz Oral Res. 2014; 28:1–7.
Article5. Torabinejad M, Parirokh M, Dummer PM. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part II: other clinical applications and complications. Int Endod J. 2018; 51:284–317. PMID: 28846134.
Article6. Kaur M, Singh H, Dhillon JS, Batra M, Saini M. MTA versus Biodentine: review of literature with a comparative analysis. J Clin Diagn Res. 2017; 11:ZG01–ZG05. PMID: 28969295.
Article7. Ghilotti J, Sanz JL, López-García S, Guerrero-Gironés J, Pecci-Lloret MP, Lozano A, Llena C, Rodríguez-Lozano FJ, Forner L, Spagnuolo G. Comparative surface morphology, chemical composition, and cytocompatibility of Bio-C Repair, Biodentine, and ProRoot MTA on hDPCs. Materials (Basel). 2020; 13:2189. PMID: 32397585.
Article8. Oliveira LV, de Souza GL, da Silva GR, Magalhães TE, Freitas GA, Turrioni AP, de Rezende Barbosa GL, Moura CC. Biological parameters, discolouration and radiopacity of calcium silicate-based materials in a simulated model of partial pulpotomy. Int Endod J. 2021; 54:2133–2144. PMID: 34418112.
Article9. Benetti F, Queiroz ÍO, Cosme-Silva L, Conti LC, Oliveira SH, Cintra LT. Cytotoxicity, biocompatibility and biomineralization of a new ready-for-use Bioceramic repair material. Braz Dent J. 2019; 30:325–332. PMID: 31340221.
Article10. Santiago MC, Gomes-Cornélio AL, de Oliveira LA, Tanomaru-Filho M, Salles LP. Calcium silicate-based cements cause environmental stiffness and show diverse potential to induce osteogenesis in human osteoblastic cells. Sci Rep. 2021; 11:16784. PMID: 34408247.
Article11. Karapinar-Kazandag M, Basrani B, Tom-Kun Yamagishi V, Azarpazhooh A, Friedman S. Fracture resistance of simulated immature tooth roots reinforced with MTA or restorative materials. Dent Traumatol. 2016; 32:146–152. PMID: 26411925.12. Linsuwanont P, Kulvitit S, Santiwong B. Reinforcement of simulated immature permanent teeth after mineral trioxide aggregate apexification. J Endod. 2018; 44:163–167. PMID: 29153732.
Article13. Nagendrababu V, Murray PE, Ordinola-Zapata R, Peters OA, Rôças IN, Siqueira JF Jr, Priya E, Jayaraman J, J Pulikkotil S, Camilleri J, Boutsioukis C, Rossi-Fedele G, Dummer PM. PRILE 2021 guidelines for reporting laboratory studies in endodontology: a consensus-based development. Int Endod J. 2021; 54:1482–1490. PMID: 33938010.
Article14. Tanalp J, Dikbas I, Malkondu O, Ersev H, Güngör T, Bayırlı G. Comparison of the fracture resistance of simulated immature permanent teeth using various canal filling materials and fiber posts. Dent Traumatol. 2012; 28:457–464. PMID: 22151797.
Article15. Brito-Júnior M, Pereira RD, Veríssimo C, Soares CJ, Faria-e-Silva AL, Camilo CC, Sousa-Neto MD. Fracture resistance and stress distribution of simulated immature teeth after apexification with mineral trioxide aggregate. Int Endod J. 2014; 47:958–966. PMID: 24386969.
Article16. Vieira HT, Vizzotto MB, da Silveira PF, Arús NA, Corrêa Travessas JA, da Silveira HL. Diagnostic efficacy of different cone beam computed tomography scanning protocols in the detection of chemically simulated external root resorption. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020; 130:322–327. PMID: 32423729.
Article17. Soares CJ, Pizi EC, Fonseca RB, Martins LR. Influence of root embedment material and periodontal ligament simulation on fracture resistance tests. Braz Oral Res. 2005; 19:11–16. PMID: 16229350.
Article18. Mello I, Michaud PL, Butt Z. Fracture resistance of immature teeth submitted to different endodontic procedures and restorative protocols. J Endod. 2020; 46:1465–1469. PMID: 32615172.
Article19. ISO 10993-5 - biological evaluation of medical devices- part 5: tests for in vitro cytotoxicity. Geneva, Switzerland: ISO;2009.20. Reis MV, de Souza GL, Moura CC, da Silva MV, Souza MA, Soares PB, Soares CJ. Effects of Lectin (ScLL) on osteoclast-like multinucleated giant cells’ maturation: a preliminary in vitro study. Dent Traumatol. 2018; 34:329–335. PMID: 29856524.
Article21. Rezende TM, Ribeiro Sobrinho AP, Vieira LQ, Sousa MG, Kawai T. Mineral trioxide aggregate (MTA) inhibits osteoclastogenesis and osteoclast activation through calcium and aluminum activities. Clin Oral Investig. 2021; 25:1805–1814.
Article22. Elnaghy A, Elsaka S. Fracture resistance of simulated immature roots using Biodentine and fiber post compared with different canal-filling materials under aging conditions. Clin Oral Investig. 2020; 24:1333–1338.
Article23. Andreasen JO. Analysis of pathogenesis and topography of replacement root resorption (ankylosis) after replantation of mature permanent incisors in monkeys. Swed Dent J. 1980; 4:231–240. PMID: 6938062.24. Fongsamootr T, Suttakul P. Effect of periodontal ligament on stress distribution and displacement of tooth and bone structure using finite element simulation. Eng J (NY). 2015; 19:99–108.
Article25. Marchionatti AM, Wandscher VF, Broch J, Bergoli CD, Maier J, Valandro LF, Kaizer OB. Influence of periodontal ligament simulation on bond strength and fracture resistance of roots restored with fiber posts. J Appl Oral Sci. 2014; 22:450–458. PMID: 25466478.
Article26. Yasin R, Al-Jundi S, Khader Y. Effect of mineral trioxide aggregate and biodentine™ on fracture resistance of immature teeth dentine over time: in vitro study. Eur Arch Paediatr Dent. 2021; 22:603–609. PMID: 33387346.
Article27. Pandolfo MT, Rover G, Bortoluzzi EA, Teixeira CD, Rossetto HL, Fernades PC, Côrte-Real IS, Carvalho SM, Garcia LD. Fracture resistance of simulated immature teeth reinforced with different mineral aggregate-based materials. Braz Dent J. 2021; 32:21–31. PMID: 34755787.
Article28. de Sá MA, Nunes E, Antunes AN, Brito Júnior M, Horta MC, Amaral RR, Cohen S, Silveira FF. Push-out bond strength and marginal adaptation of apical plugs with bioactive endodontic cements in simulated immature teeth. Restor Dent Endod. 2021; 46:e53. PMID: 34909417.
Article29. Danwittayakorn S, Banomyong D, Ongchavalit L, Ngoenwiwatkul Y, Porkaew P. Comparison of the effects of intraradicular materials on the incidence of fatal root fracture in immature teeth treated with mineral trioxide aggregate apexification: a retrospective study. J Endod. 2019; 45:977–984.e1. PMID: 31248698.
Article30. Sano H, Ciucchi B, Matthews WG, Pashley DH. Tensile properties of mineralized and demineralized human and bovine dentin. J Dent Res. 1994; 73:1205–1211. PMID: 8046110.
Article31. Schilke R, Lisson JA, Bauss O, Geurtsen W. Comparison of the number and diameter of dentinal tubules in human and bovine dentine by scanning electron microscopic investigation. Arch Oral Biol. 2000; 45:355–361. PMID: 10739856.
Article32. Reis AF, Giannini M, Kavaguchi A, Soares CJ, Line SR. Comparison of microtensile bond strength to enamel and dentin of human, bovine, and porcine teeth. J Adhes Dent. 2004; 6:117–121. PMID: 15293420.33. Soares CJ, Barbosa LM, Santana FR, Soares PB, Mota AS, Silva GR. Fracture strength of composite fixed partial denture using bovine teeth as a substitute for human teeth with or without fiber-reinforcement. Braz Dent J. 2010; 21:235–240. PMID: 21203707.
Article34. Rodrigues MN, Bruno KF, de Alencar AH, Silva JD, de Siqueira PC, Decurcio DA, Estrela C. Comparative analysis of bond strength to root dentin and compression of bioceramic cements used in regenerative endodontic procedures. Restor Dent Endod. 2021; 46:e59. PMID: 34909423.
Article35. Belli S, Eraslan O, Eskitaşcıoğlu G. Effect of different treatment options on biomechanics of immature teeth: a finite element stress analysis study. J Endod. 2018; 44:475–479. PMID: 29254818.
Article36. Tay FR, Pashley DH. Monoblocks in root canals: a hypothetical or a tangible goal. J Endod. 2007; 33:391–398. PMID: 17368325.
Article37. Honegger P. Overview of cell and tissue culture techniques. Curr Protocols Pharmacol. 2001; Chapter 12:12.1.
Article38. Collin-Osdoby P, Osdoby P. RANKL-mediated osteoclast formation from murine RAW 264.7 cells. Methods Mol Biol. 2012; 816:187–202. PMID: 22130930.
Article39. Oliveira LV, da Silva GR, Souza GL, Magalhães TE, Barbosa GL, Turrioni AP, Moura CC. A laboratory evaluation of cell viability, radiopacity and tooth discoloration induced by regenerative endodontic materials. Int Endod J. 2020; 53:1140–1152. PMID: 32299123.
Article40. Kim M, Kim S, Ko H, Song M. Effect of ProRoot MTA® and Biodentine® on osteoclastic differentiation and activity of mouse bone marrow macrophages. J Appl Oral Sci. 2019; 27:e20180150. PMID: 30624466.
Article41. Cheng X, Zhu L, Zhang J, Yu J, Liu S, Lv F, Lin Y, Liu G, Peng B. Anti-osteoclastogenesis of mineral trioxide aggregate through inhibition of the autophagic pathway. J Endod. 2017; 43:766–773. PMID: 28292604.
Article42. da Fonseca TS, Silva GF, Guerreiro-Tanomaru JM, Delfino MM, Sasso-Cerri E, Tanomaru-Filho M, Cerri PS. Biodentine and MTA modulate immunoinflammatory response favoring bone formation in sealing of furcation perforations in rat molars. Clin Oral Investig. 2019; 23:1237–1252.
Article43. Faloni AP, Sasso-Cerri E, Rocha FR, Katchburian E, Cerri PS. Structural and functional changes in the alveolar bone osteoclasts of estrogen-treated rats. J Anat. 2012; 220:77–85. PMID: 22092353.
Article44. Zaidi M, Adebanjo OA, Moonga BS, Sun L, Huang CL. Emerging insights into the role of calcium ions in osteoclast regulation. J Bone Miner Res. 1999; 14:669–674. PMID: 10320514.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Affecting the Pulp and Root Healing of Root Fractures in Immature Permanent Teeth
- A roentgenographic study on apical root resorption of human permanent teeth
- Calcium silicate-based root canal sealers: a literature review
- A micro-computed tomography evaluation of voids using calcium silicate-based materials in teeth with simulated internal root resorption
- Orthodontic treatment of molar teeth impacted by local factors