Restor Dent Endod.
2023 Feb;48(1):e5. 10.5395/rde.2023.48.e5.
Effect of endodontic sealer on postoperative pain: a network metaanalysis
- Affiliations
-
- 1Department of Endodontics, Paulo Picanço School of Dentistry, Fortaleza, CE, Brazil
- 2Department of Restorative Dentistry, State University of Ponta Grossa, Ponta Grossa, PR, Brazil
- KMID: 2548173
- DOI: http://doi.org/10.5395/rde.2023.48.e5
Abstract
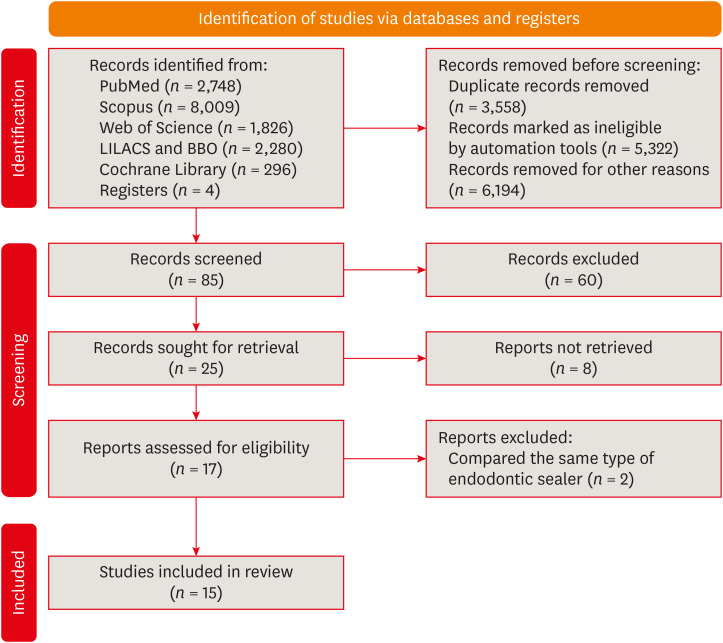
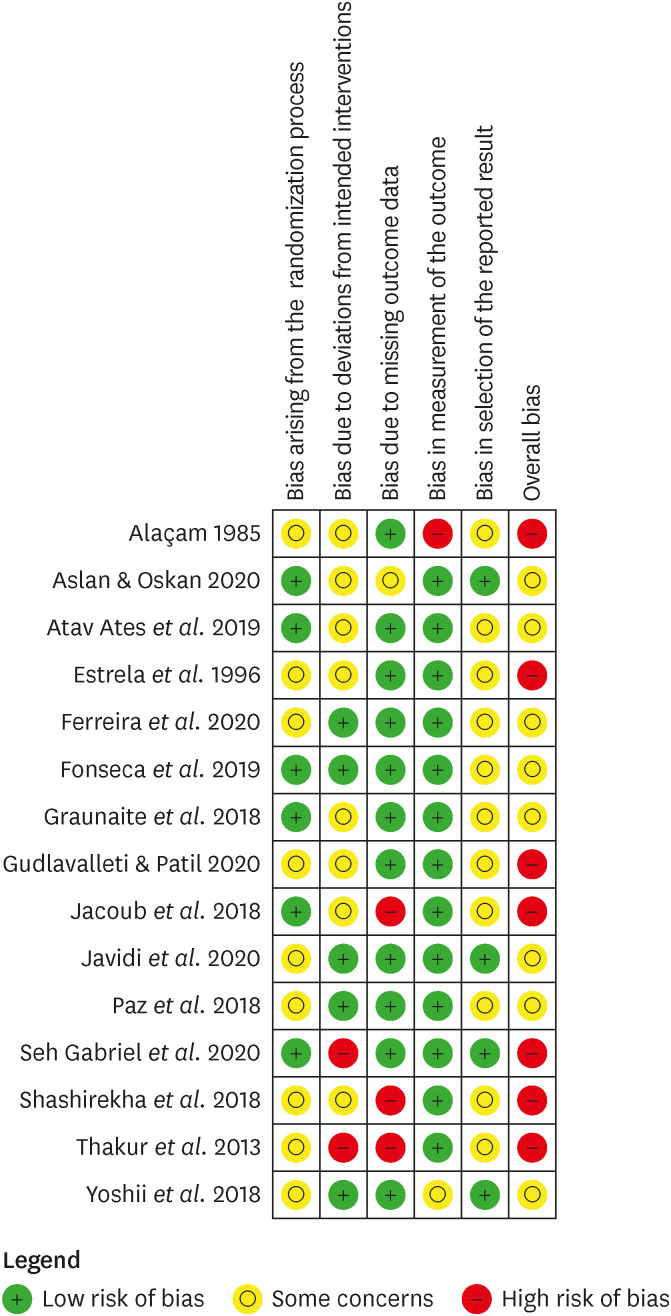
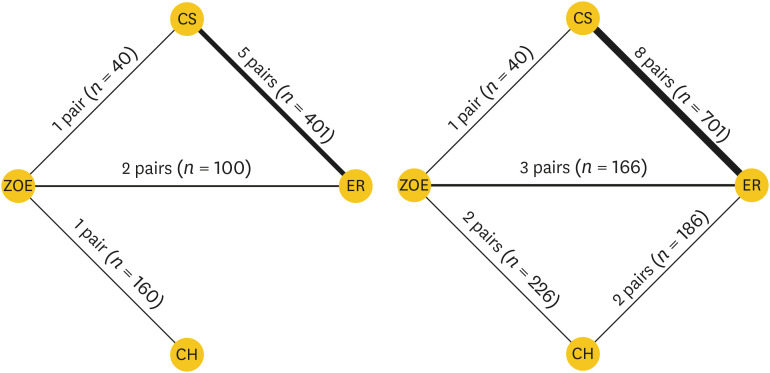
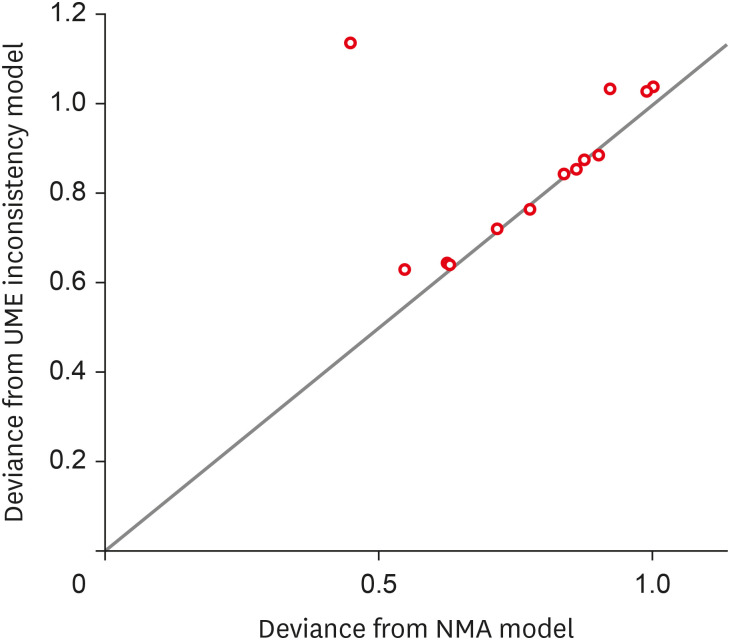
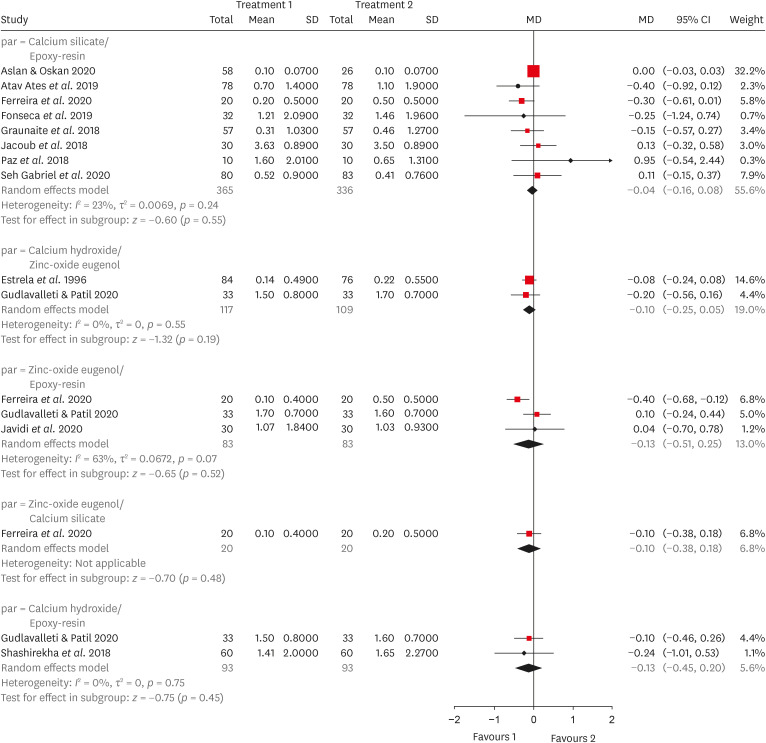
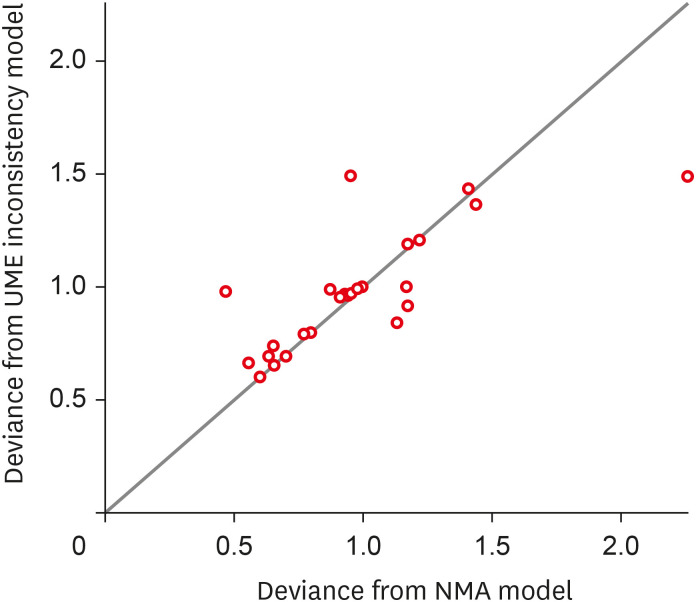
- This systematic review and network meta-analysis aimed to answer the following focused research question: “Does the type of endodontic sealer affect the postoperative pain in patients who received endodontic treatment?” Different databases and grey literature were surveyed. Only one randomized controlled trial were included. The risk of bias in the studies was evaluated by using the Cochrane Collaboration’s tool. A random-effects metaanalysis was conducted to compare the risk and intensity of postoperative pain. The quality of the body of evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation approach. Out of 11,601 studies, 15 remained for qualitative analyses and 12 for meta-analysis. Seven studies were classified at high risk of bias, and 8 studies raised some concerns. No significant differences between the endodontic materials were observed in the direct comparisons, both in risk and in intensity of postoperative pain (pairwise comparisons with 2 studies: I2 = 0%; p > 0.05 and 8 studies: I2 = 23%; p > 0.05, respectively). The certainty of the evidence was graded as low or moderate. There was no difference in the risk and intensity of postoperative pain after filling with different endodontic sealers. Further systematic reviews should be conducted.
Keyword
Figure
Reference
-
1. Benenati FW. Obturation of the radicular space. Ingle JI, Bakland LK, Baumgartner JC, editors. Endodontics. 6th ed. Hamilton: BC Decker;2008. p. 1053–1087.2. Holland R, Gomes JE, Cintra LT, Queiroz ÍO, Estrela C. Factors affecting the periapical healing process of endodontically treated teeth. J Appl Oral Sci. 2017; 25:465–476. PMID: 29069143.
Article3. Sathorn C, Parashos P, Messer H. The prevalence of postoperative pain and flare-up in single- and multiple-visit endodontic treatment: a systematic review. Int Endod J. 2008; 41:91–99. PMID: 17956561.
Article4. Manfredi M, Figini L, Gagliani M, Lodi G. Single versus multiple visits for endodontic treatment of permanent teeth. Cochrane Database Syst Rev. 2016; 12:CD005296. PMID: 27905673.
Article5. AlRahabi MK. Predictors, prevention, and management of postoperative pain associated with nonsurgical root canal treatment: a systematic review. J Taibah Univ Med Sci. 2017; 12:376–384. PMID: 31435267.
Article6. Zuckerman O, Metzger Z, Sela G, Lin S. "Flare-up" during endodontic treatment--etiology and management. Refuat Hapeh Vehashinayim. 1993; 2007:19–26.7. Mostafa ME, El-Shrief YA, Anous WI, Hassan MW, Salamah FT, El Boghdadi RM, El-Bayoumi MA, Seyam RM, Abd-El-Kader KG, Amin SA. Postoperative pain following endodontic irrigation using 1.3% versus 5.25% sodium hypochlorite in mandibular molars with necrotic pulps: a randomized double-blind clinical trial. Int Endod J. 2020; 53:154–166. PMID: 31563148.
Article8. Saha SG, Gupta RK, Bhardwaj A, Misuriya A, Saha MK, Nirwan AS. Comparison of the incidence of postoperative pain after using a continuous rotary system, a reciprocating system, and a Self-Adjusting File system in single-visit endodontics: a prospective randomized clinical trial. J Conserv Dent. 2018; 21:333–338. PMID: 29899640.
Article9. Vianna EC, Herkrath FJ, Martins IE, Lopes LP, Marques AA, Sponchiado Júnior EC. Effect of occlusal adjustment on postoperative pain after root canal treatment: a randomized clinical trial. Braz Dent J. 2020; 31:353–359. PMID: 32901709.
Article10. Javidi M, Zarei M, Ashrafpour E, Gharechahi M, Bagheri H. Post-treatment flare-up incidence after using nano zinc oxide eugenol sealer in mandibular first molars with irreversible pulpitis. J Dent (Shiraz). 2020; 21:307–313. PMID: 33344681.11. Rosen E, Goldberger T, Taschieri S, Del Fabbro M, Corbella S, Tsesis I. The prognosis of altered sensation after extrusion of root canal filling materials: a systematic review of the literature. J Endod. 2016; 42:873–879. PMID: 27133502.
Article12. Ørstavik D. Materials used for root canal obturation: technical, biological and clinical testing. Endod Topics. 2005; 12:25–38.
Article13. Lim M, Jung C, Shin DH, Cho YB, Song M. Calcium silicate-based root canal sealers: a literature review. Restor Dent Endod. 2020; 45:e35. PMID: 32839716.
Article14. Thakur S, Emil J, Paulaian B. Evaluation of mineral trioxide aggregate as root canal sealer: a clinical study. J Conserv Dent. 2013; 16:494–498. PMID: 24347880.
Article15. Paz A, Vasconcelos I, Ginjeira A. Evaluation of postoperative pain after using bioceramic materials as endodontic sealers. EC Dent Sci. 2018; 10:1739–1748.16. Fonseca B, Coelho MS, Bueno CE, Fontana CE, Martin AS, Rocha DG. Assessment of extrusion and postoperative pain of a bioceramic and resin-based root canal sealer. Eur J Dent. 2019; 13:343–348. PMID: 31794999.
Article17. Aslan T, Dönmez Özkan H. The effect of two calcium silicate-based and one epoxy resin-based root canal sealer on postoperative pain: a randomized controlled trial. Int Endod J. 2021; 54:190–197. PMID: 32929721.
Article18. Gudlavalleti B, Patil AA. Comparative evaluation of postoperative pain after root canal treatment using three different sealers, Viz., Tubli-Seal EWT, Apexit Plus, AH Plus: an in-vivo study. J Clin Diagn Res. 2020; 14:ZC04–ZC09.19. Tan HS, Lim KC, Lui JN, Lai WM, Yu VS. Postobturation pain associated with tricalcium silicate and resin-based sealer techniques: a randomized clinical trial. J Endod. 2021; 47:169–177. PMID: 33098889.
Article20. Sponchiado Junior EC, Vieira WA, Normando AG, Pereira JV, Ferraz CC, Almeida JF, Marciano MA, Gomes BP, de-Jesus-Soares A. Calcium silicate-based sealers do not reduce the risk and intensity of postoperative pain after root canal treatment when compared with epoxy resin-based sealers: a systematic review and meta-analysis. Eur J Dent. 2021; 15:347–359. PMID: 33759149.
Article21. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71. PMID: 33782057.
Article22. Larocca de Geus J, Nogueira da Costa JK, Wambier LM, Maran BM, Loguercio AD, Reis A. Different anesthetics on the efficacy of inferior alveolar nerve block in patients with irreversible pulpitis: a network systematic review and meta-analysis. J Am Dent Assoc. 2020; 151:87–97.e4. PMID: 31813471.23. Maran BM, Ziegelmann PK, Burey A, de Paris Matos T, Loguercio AD, Reis A. Different light-activation systems associated with dental bleaching: a systematic review and a network meta-analysis. Clin Oral Investig. 2019; 23:1499–1512.
Article24. Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JP. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019; 366:l4898. PMID: 31462531.
Article25. Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010; 29:932–944. PMID: 20213715.
Article26. Puhan MA, Schünemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, Kessels AG, Guyatt GH. GRADE Working Group. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014; 349:g5630. PMID: 25252733.
Article27. Nabi S, Farooq R, Purra A, Ahmed F. Comparison of various sealers on postoperative pain in single-visit endodontics: a randomized clinical study. Indian J Dent Sci. 2019; 11:99–102.
Article28. Sharma N, Mandhotra P, Kumari S, Chandel N. A study to compare various sealers on postoperative pain in single visit endodontics. Ann Int Med Dent Res. 2019; 6:40–42.29. Graunaite I, Skucaite N, Lodiene G, Agentiene I, Machiulskiene V. Effect of resin-based and bioceramic root canal sealers on postoperative pain: a split-mouth randomized controlled trial. J Endod. 2018; 44:689–693. PMID: 29571915.
Article30. Yoshii S, Morotomi T, Fujimoto M, Washio A, Miyashita K, Kitamura C.. A pilot study on the effects of two types of root canal sealer on postoperative pain. J Jpn Endod Assoc. 2018; 39:43–48.31. Atav Ates A, Dumani A, Yoldas O, Unal I. Post-obturation pain following the use of carrier-based system with AH Plus or iRoot SP sealers: a randomized controlled clinical trial. Clin Oral Investig. 2019; 23:3053–3061.
Article32. Ferreira NS, Gollo EK, Boscato N, Arias A, Silva EJ. Postoperative pain after root canal filling with different endodontic sealers: a randomized clinical trial. Braz Oral Res. 2020; 34:e069. PMID: 32696911.
Article33. Jacoub MS, Kataia MA, Hashem AA, Hafiz EA. The influence of two instrumentation techniques with two sealers on postoperative pain after endodontic treatment “randomized clinical trial”. Future Dent J. 2018; 4:175–180.
Article34. Shashirekha G, Jena A, Pattanaik S, Rath J. Assessment of pain and dissolution of apically extruded sealers and their effect on the periradicular tissues. J Conserv Dent. 2018; 21:546–550. PMID: 30294119.
Article35. Estrela C, Siqueira RMG, Resende EV, Silva SA, Silva FAC. Influência da substância química, do cimento obturador e do número de sessões na incidência de pericementite traumática. Rev Odontol Bras Cent. 1996; 6:9–13.36. Alacam T. Incidence of postoperative pain following the use of different sealers in immediate root canal filling. J Endod. 1985; 11:135–137. PMID: 3858406.
Article37. Komabayashi T, Colmenar D, Cvach N, Bhat A, Primus C, Imai Y. Comprehensive review of current endodontic sealers. Dent Mater J. 2020; 39:703–720. PMID: 32213767.
Article38. Desai S, Chandler N. Calcium hydroxide-based root canal sealers: a review. J Endod. 2009; 35:475–480. PMID: 19345790.
Article39. Raghavendra SS, Jadhav GR, Gathani KM, Kotadia P. Bioceramics in endodontics - a review. J Istanb Univ Fac Dent. 2017; 51:S128–S137. PMID: 29354316.40. Lodienė G, Kopperud HM, Ørstavik D, Bruzell EM. Detection of leachables and cytotoxicity after exposure to methacrylate- and epoxy-based root canal sealers in vitro . Eur J Oral Sci. 2013; 121:488–496. PMID: 24028598.
Article41. Seo DG, Lee D, Kim YM, Song D, Kim SY. Biocompatibility and mineralization activity of three calcium silicate-based root canal sealers compared to conventional resin-based sealer in human dental pulp stem cells. Materials (Basel). 2019; 12:E2482.
Article42. Silva-Herzog D, Ramírez T, Mora J, Pozos AJ, Silva LA, Silva RA, Nelson-Filho P. Preliminary study of the inflammatory response to subcutaneous implantation of three root canal sealers. Int Endod J. 2011; 44:440–446. PMID: 21255048.
Article43. Zhang W, Peng B. Tissue reactions after subcutaneous and intraosseous implantation of iRoot SP, MTA and AH Plus. Dent Mater J. 2015; 34:774–780. PMID: 26632225.
Article44. Nusstein J, Lee S, Reader A, Beck M, Weaver J. Injection pain and postinjection pain of the anterior middle superior alveolar injection administered with the Wand or conventional syringe. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 98:124–131. PMID: 15243483.
Article45. Wambier LM, de Geus JL, Boing TF, Brancher JA, Chibinski AC, Wambier DS, Farago PV, Loguercio AD, Reis A. A randomized clinical trial evaluating rubber dam clamp pain reduction from a new topical liposomal anesthetic gel. Pediatr Dent. 2018; 40:190–194. PMID: 29793565.46. Khan J, Zusman T, Wang Q, Eliav E. Acute and chronic pain in orofacial trauma patients. Dent Traumatol. 2019; 35:348–357. PMID: 31125489.
Article47. Bernáth M, Szabó J. Tissue reaction initiated by different sealers. Int Endod J. 2003; 36:256–261. PMID: 12702119.
Article48. Pocock SJ. Clinical trials: a practical approach. Chichester: John Wiley & Sons;1983.49. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995; 273:408–412. PMID: 7823387.
Article50. Khan KS, Daya S, Jadad A. The importance of quality of primary studies in producing unbiased systematic reviews. Arch Intern Med. 1996; 156:661–666. PMID: 8629879.
Article51. Albashaireh ZS, Alnegrish AS. Postobturation pain after single- and multiple-visit endodontic therapy. A prospective study. J Dent. 1998; 26:227–232. PMID: 9594474.
Article52. Su Y, Wang C, Ye L. Healing rate and post-obturation pain of single- versus multiple-visit endodontic treatment for infected root canals: a systematic review. J Endod. 2011; 37:125–132. PMID: 21238790.
Article53. Almeida DO, Chaves SC, Souza RA, Soares FF. Outcome of single- vs multiple-visit endodontic therapy of nonvital teeth: a meta-analysis. J Contemp Dent Pract. 2017; 18:330–336. PMID: 28349914.
Article54. Gondim E Jr, Setzer FC, Dos Carmo CB, Kim S. Postoperative pain after the application of two different irrigation devices in a prospective randomized clinical trial. J Endod. 2010; 36:1295–1301. PMID: 20647083.
Article55. Ramamoorthi S, Nivedhitha MS, Divyanand MJ. Comparative evaluation of postoperative pain after using endodontic needle and EndoActivator during root canal irrigation: a randomised controlled trial. Aust Endod J. 2015; 41:78–87. PMID: 25195661.
Article56. Gotler M, Bar-Gil B, Ashkenazi M. Postoperative pain after root canal treatment: a prospective cohort study. Int J Dent. 2012; 2012:310467. PMID: 22505897.
Article57. Alonso-Ezpeleta LO, Gasco-Garcia C, Castellanos-Cosano L, Martín-González J, López-Frías FJ, Segura-Egea JJ. Postoperative pain after one-visit root-canal treatment on teeth with vital pulps: comparison of three different obturation techniques. Med Oral Patol Oral Cir Bucal. 2012; 17:e721–e727. PMID: 22322522.
Article58. Rahimi S, Shahi S, Yavari HR, Reyhani MF, Ebrahimi ME, Rajabi E. A stereomicroscopy study of root apices of human maxillary central incisors and mandibular second premolars in an Iranian population. J Oral Sci. 2009; 51:411–415. PMID: 19776508.
Article59. Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL 3rd. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009; 10:447–485. PMID: 19411059.
Article60. Pieretti S, Di Giannuario A, Di Giovannandrea R, Marzoli F, Piccaro G, Minosi P, Aloisi AM. Gender differences in pain and its relief. Ann Ist Super Sanita. 2016; 52:184–189. PMID: 27364392.61. Cooper NJ, Peters J, Lai MC, Juni P, Wandel S, Palmer S, Paulden M, Conti S, Welton NJ, Abrams KR, Bujkiewicz S, Spiegelhalter D, Sutton AJ. How valuable are multiple treatment comparison methods in evidence-based health-care evaluation? Value Health. 2011; 14:371–380. PMID: 21296599.
Article62. Caldwell DM, Dias S, Welton NJ. Extending treatment networks in health technology assessment: how far should we go? Value Health. 2015; 18:673–681. PMID: 26297096.
Article63. Chaimani A, Caldwell DM, Li T, Higgins JPT, Salanti G. Chapter 11: Undertaking network meta-analyses. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.2. Chichester: John Wiley & Sons;2021.64. Fonseca DA, Paula AB, Marto CM, Coelho A, Paulo S, Martinho JP, Carrilho E, Ferreira MM. Biocompatibility of root canal sealers: a systematic review of in vitro and in vivo studies. Materials (Basel). 2019; 12:4113. PMID: 31818038.
Article65. Coghill RC. Individual differences in the subjective experience of pain: new insights into mechanisms and models. Headache. 2010; 50:1531–1535. PMID: 20958300.
Article66. Martín-González J, Echevarría-Pérez M, Sánchez-Domínguez B, Tarilonte-Delgado ML, Castellanos-Cosano L, López-Frías FJ, Segura-Egea JJ. Influence of root canal instrumentation and obturation techniques on intra-operative pain during endodontic therapy. Med Oral Patol Oral Cir Bucal. 2012; 17:e912–e918. PMID: 22549694.67. Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, Kvarstein G, Stubhaug A. Assessment of pain. Br J Anaesth. 2008; 101:17–24. PMID: 18487245.
Article68. Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005; 14:798–804. PMID: 16000093.
Article69. Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE handbook for grading quality of evidence and strength of recommendations. place unknown: The GRADE Working Group;2013.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postoperative pain after endodontic treatment of necrotic teeth with large intentional foraminal enlargement
- Retreatability of two endodontic sealers, EndoSequence BC Sealer and AH Plus: a micro-computed tomographic comparison
- Comparison of pretreatment gabapentin and pregabalin to control postoperative endodontic pain – a double-blind, randomized clinical trial
- Micro-computed tomographic evaluation of single-cone obturation with three sealers
- Effect of intracanal cryotherapy on postoperative pain after endodontic treatment: systematic review with meta-analysis