Diabetes Metab J.
2023 Nov;47(6):859-868. 10.4093/dmj.2022.0377.
Prediabetes Progression and Regression on Objectively- Measured Physical Function: A Prospective Cohort Study
- Affiliations
-
- 1Department of General Practice, Institute of Diabetes, Zhongda Hospital, School of Medicine, Southeast University, Nanjing,
- 2Research and Education Centre of General Practice, Zhongda Hospital, Southeast University, Nanjing,
- 3Department of Endocrinology, Institute of Diabetes, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, China
- 4Department of Clinical Sciences, Liverpool School of Tropical Medicine, Liverpool, UK
- 5Department of Nursing Management, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, China
- 6Adelaide Medical School and Centre of Research Excellence (CRE) in Translating Nutritional Science to Good Health, The University of Adelaide, Adelaide, Australia
- KMID: 2548162
- DOI: http://doi.org/10.4093/dmj.2022.0377
Abstract
- Background
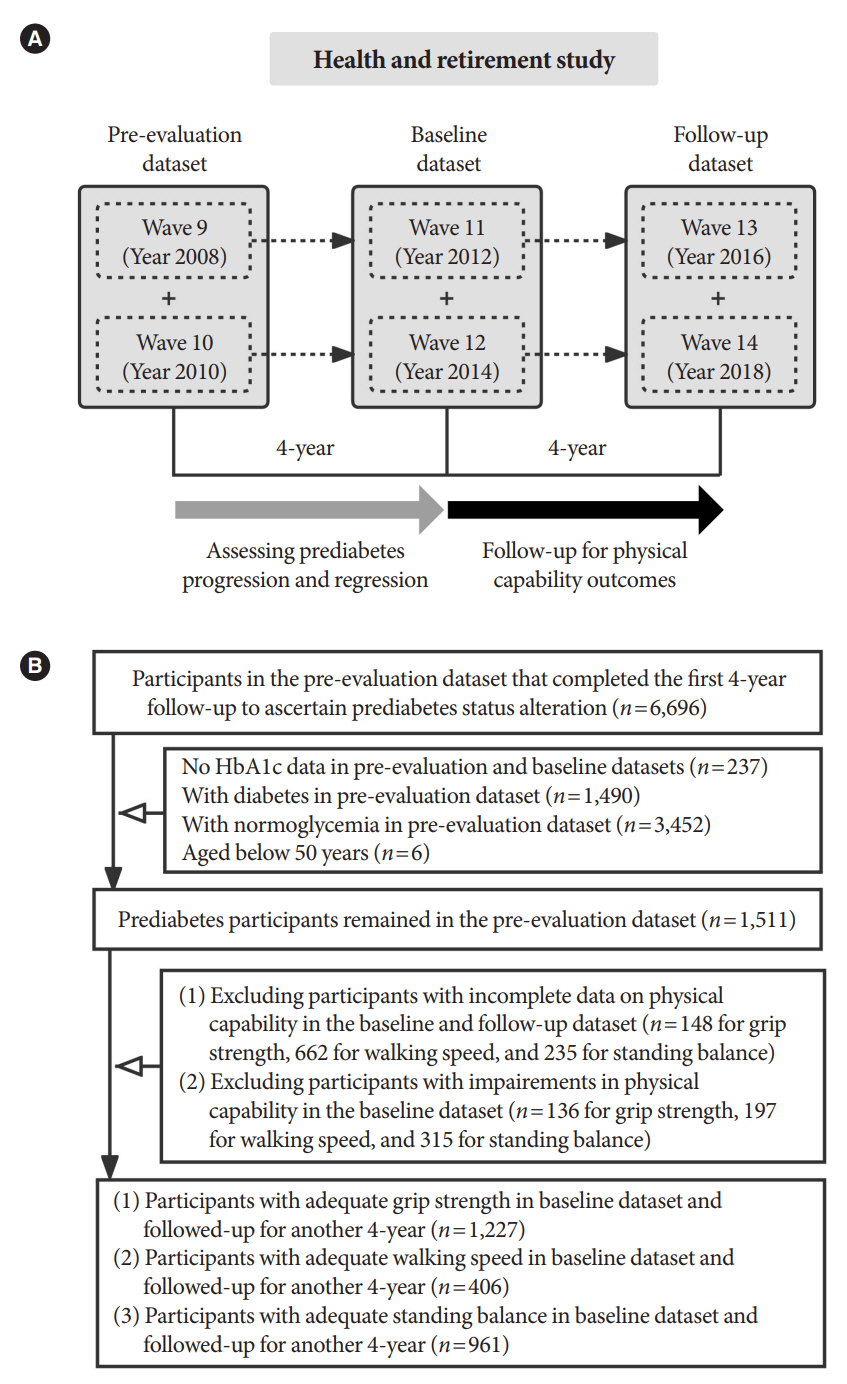
Prediabetes leads to declines in physical function in older adults, but the impact of prediabetes progression or regression on physical function is unknown. This study assessed this longitudinal association, with physical function objectivelymeasured by grip strength, walking speed, and standing balance, based on the Health and Retirement Study enrolling United States adults aged >50 years.
Methods
Participants with prediabetes were followed-up for 4-year to ascertain prediabetes status alteration (maintained, regressed, or progressed), and another 4-year to assess their impacts on physical function. Weak grip strength was defined as <26 kg for men and <16 kg for women, slow walking speed was as <0.8 m/sec, and poor standing balance was as an uncompleted fulltandem standing testing. Logistic and linear regression analyses were performed.
Results
Of the included 1,511 participants with prediabetes, 700 maintained as prediabetes, 306 progressed to diabetes, and 505 regressed to normoglycemia over 4 years. Grip strength and walking speed were declined from baseline during the 4-year followup, regardless of prediabetes status alteration. Compared with prediabetes maintenance, prediabetes progression increased the odds of developing weak grip strength by 89% (95% confidence interval [CI], 0.04 to 2.44) and exhibited larger declines in grip strength by 0.85 kg (95% CI, –1.65 to –0.04). However, prediabetes progression was not related to impairments in walking speed or standing balance. Prediabetes regression also did not affect any measures of physical function.
Conclusion
Prediabetes progression accelerates grip strength decline in aging population, while prediabetes regression may not prevent physical function decline due to aging.
Keyword
Figure
Reference
-
1. Cooper R, Kuh D, Cooper C, Gale CR, Lawlor DA, Matthews F, et al. Objective measures of physical capability and subsequent health: a systematic review. Age Ageing. 2011; 40:14–23.
Article2. Qiu S, Cai X, Zheng P, Yuan Y, Xu Y, Jia L, et al. Changes in objectively-measured physical capability over 4-year, risk of diabetes, and glycemic control in older adults: the China Health and Retirement Longitudinal study. Diabetes Res Clin Pract. 2022; 184:109186.
Article3. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48:601.
Article4. de Oliveira DC, de Oliveira Maximo R, Ramirez PC, de Souza AF, Luiz MM, Delinocente ML, et al. Is slowness a better discriminator of disability than frailty in older adults? J Cachexia Sarcopenia Muscle. 2021; 12:2069–78.
Article5. Cooper R, Strand BH, Hardy R, Patel KV, Kuh D. Physical capability in mid-life and survival over 13 years of follow-up: British birth cohort study. BMJ. 2014; 348:g2219.
Article6. Hostalek U. Global epidemiology of prediabetes: present and future perspectives. Clin Diabetes Endocrinol. 2019; 5:5.7. Li Y, Teng D, Shi X, Qin G, Qin Y, Quan H, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020; 369:m997.
Article8. Shang Y, Fratiglioni L, Vetrano DL, Dove A, Welmer AK, Xu W. Not only diabetes but also prediabetes leads to functional decline and disability in older adults. Diabetes Care. 2021; 44:690–8.
Article9. Rooney MR, Rawlings AM, Pankow JS, Echouffo Tcheugui JB, Coresh J, Sharrett AR, et al. Risk of progression to diabetes among older adults with prediabetes. JAMA Intern Med. 2021; 181:511–9.
Article10. Lazo-Porras M, Bernabe-Ortiz A, Ruiz-Alejos A, Smeeth L, Gilman RH, Checkley W, et al. Regression from prediabetes to normal glucose levels is more frequent than progression towards diabetes: the CRONICAS Cohort Study. Diabetes Res Clin Pract. 2020; 163:107829.
Article11. Liu X, Wu S, Song Q, Wang X. Reversion from pre-diabetes mellitus to normoglycemia and risk of cardiovascular disease and all-cause mortality in a Chinese population: a prospective cohort study. J Am Heart Assoc. 2021; 10:e019045.
Article12. Vistisen D, Kivimaki M, Perreault L, Hulman A, Witte DR, Brunner EJ, et al. Reversion from prediabetes to normoglycaemia and risk of cardiovascular disease and mortality: the Whitehall II cohort study. Diabetologia. 2019; 62:1385–90.
Article13. Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. Cohort profile: the Health and Retirement Study (HRS). Int J Epidemiol. 2014; 43:576–85.
Article14. Peterson MD, Casten K, Collins S, Hassan H, Garcia-Hermoso A, Faul J. Muscle weakness is a prognostic indicator of disability and chronic disease multimorbidity. Exp Gerontol. 2021; 152:111462.
Article15. Bardenheier BH, Wu WC, Zullo AR, Gravenstein S, Gregg EW. Progression to diabetes by baseline glycemic status among middle-aged and older adults in the United States, 2006-2014. Diabetes Res Clin Pract. 2021; 174:108726.
Article16. Kim ES, Kawachi I, Chen Y, Kubzansky LD. Association between purpose in life and objective measures of physical function in older adults. JAMA Psychiatry. 2017; 74:1039–45.
Article17. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care. 2019; 42(Suppl 1):S13–28.18. Duchowny KA, Peterson MD, Clarke PJ. Cut points for clinical muscle weakness among older Americans. Am J Prev Med. 2017; 53:63–9.
Article19. Kitamura A, Seino S, Abe T, Nofuji Y, Yokoyama Y, Amano H, et al. Sarcopenia: prevalence, associated factors, and the risk of mortality and disability in Japanese older adults. J Cachexia Sarcopenia Muscle. 2021; 12:30–8.
Article20. Yu R, Ong S, Cheung O, Leung J, Woo J. Reference values of grip strength, prevalence of low grip strength, and factors affecting grip strength values in Chinese adults. J Am Med Dir Assoc. 2017; 18:551.
Article21. Perreault L, Temprosa M, Mather KJ, Horton E, Kitabchi A, Larkin M, et al. Regression from prediabetes to normal glucose regulation is associated with reduction in cardiovascular risk: results from the Diabetes Prevention Program outcomes study. Diabetes Care. 2014; 37:2622–31.
Article22. de Abreu L, Holloway KL, Kotowicz MA, Pasco JA. Dysglycaemia and other predictors for progression or regression from impaired fasting glucose to diabetes or normoglycaemia. J Diabetes Res. 2015; 2015:373762.
Article23. Pratte KA, Johnson A, Beals J, Bullock A, Manson SM, Jiang L, et al. Regression to normal glucose regulation in American Indians and Alaska natives of a diabetes prevention program. Diabetes Care. 2019; 42:1209–16.
Article24. Tabak AG, Herder C, Rathmann W, Brunner EJ, Kivimaki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012; 379:2279–90.
Article25. Wu F, Callisaya M, Laslett LL, Wills K, Zhou Y, Jones G, et al. Lower limb muscle strength is associated with poor balance in middle-aged women: linear and nonlinear analyses. Osteoporos Int. 2016; 27:2241–8.
Article26. Qiu S, Cai X, Yuan Y, Xie B, Sun Z, Wang D, et al. Muscle strength and prediabetes progression and regression in middle-aged and older adults: a prospective cohort study. J Cachexia Sarcopenia Muscle. 2022; 13:909–18.
Article27. Perreault L, Pan Q, Mather KJ, Watson KE, Hamman RF, Kahn SE, et al. Effect of regression from prediabetes to normal glucose regulation on long-term reduction in diabetes risk: results from the Diabetes Prevention Program Outcomes Study. Lancet. 2012; 379:2243–51.
Article28. International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009; 32:1327–34.29. Abellan van Kan G, Rolland Y, Andrieu S, Bauer J, Beauchet O, Bonnefoy M, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009; 13:881–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lifestyle-related predictors affecting prediabetes and diabetes in 20-30-year-old young Korean adults
- Sex differences in factors associated with prediabetes in Korean adults
- Physical Functions and Comorbidity Affecting Collapse at 4 or More Weeks after Admission in Patients with Osteoporotic Vertebral Fractures: A Prospective Cohort Study
- Physical Activity and Prevalence of Rheumatoid Arthritis in Korean Adults with Prediabetes in the 2009–2013 National Health Cohort Study
- Association of Serum Vitamin D Status with Prediabetes and Prehypertension in Korean Adults: An Analysis of the 2013–2015 Korea National Health and Nutrition Examination Survey Data