Restor Dent Endod.
2021 Nov;46(4):e53. 10.5395/rde.2021.46.e53.
Push-out bond strength and marginal adaptation of apical plugs with bioactive endodontic cements in simulated immature teeth
- Affiliations
-
- 1Department of Dentistry, Pontifical Catholic University of Minas Gerais, Belo Horizonte, Minas Gerais, Brazil
- 2Department Dentistry, Montes Claros, Minas Gerais, Brazil
- 3Department of Endodontics, Arthur School of Dentistry, University of the Pacific, San Francisco, CA, USA
- KMID: 2548097
- DOI: http://doi.org/10.5395/rde.2021.46.e53
Abstract
Objectives
This study evaluates the bond strength and marginal adaptation of mineral trioxide aggregate (MTA) Repair HP and Biodentine used as apical plugs; MTA was used as reference material for comparison.
Materials and Methods
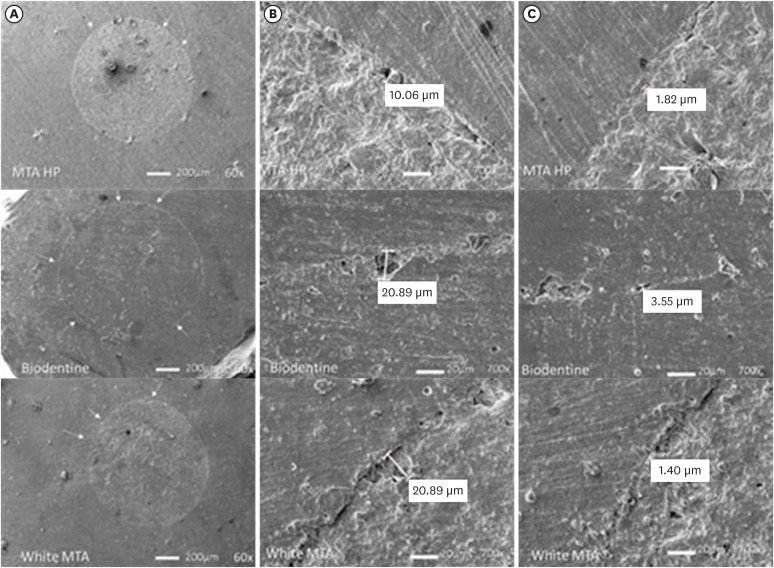
A total of 30 single-rooted teeth with standardized, artificially created open apices were randomly divided into 3 groups (n = 10 per group), according to the material used to form 6-mm-thick apical plugs: group 1 (MTA Repair HP); group 2 (Biodentine); and group 3 (white MTA). Subsequently, the specimens were transversely sectioned to obtain 2 (cervical and apical) 2.5-mm-thick slices per root. Epoxy resin replicas were observed under a scanning electron microscope to measure the gap size at the material/ dentin interface (the largest and smaller gaps were recorded for each replica). The bond strength of the investigated materials to dentin was determined using the push-out test. The variable bond strengths and gap sizes were evaluated independently at the apical and cervical root dentin slices. Data were analyzed using descriptive and analytic statistics.
Results
The comparison between the groups regarding the variables' bond strengths and gap sizes showed no statistical difference (p > 0.05) except for a single difference in the smallest gap at the cervical root dentin slice, which was higher in group 3 than in group 1 (p < 0.05).
Conclusions
The bond strength and marginal adaptation to root canal walls of MTA HP and Biodentine cement were comparable to white MTA.
Keyword
Figure
Cited by 1 articles
-
Effects of different calcium-silicate based materials on fracture resistance of immature permanent teeth with replacement root resorption and osteoclastogenesis
Gabriela Leite de Souza, Gabrielle Alves Nunes Freitas, Maria Tereza Hordones Ribeiro, Nelly Xiomara Alvarado Lemus, Carlos José Soares, Camilla Christian Gomes Moura
Restor Dent Endod. 2023;48(2):e21. doi: 10.5395/rde.2023.48.e21.
Reference
-
1. Sisli SN, Ozbas H. Comparative micro-computed tomographic evaluation of the sealing quality of ProRoot MTA and MTA Angelus apical plugs placed with various techniques. J Endod. 2017; 43:147–151. PMID: 27939735.
Article2. Torabinejad M, Parirokh M, Dummer PM. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part II: other clinical applications and complications. Int Endod J. 2018; 51:284–317. PMID: 28846134.
Article3. Ber BS, Hatton JF, Stewart GP. Chemical modification of ProRoot MTA to improve handling characteristics and decrease setting time. J Endod. 2007; 33:1231–1234. PMID: 17889696.
Article4. Guimarães BM, Prati C, Duarte MA, Bramante CM, Gandolfi MG. Physicochemical properties of calcium silicate-based formulations MTA Repair HP and MTA Vitalcem. J Appl Oral Sci. 2018; 26:e2017115. PMID: 29641748.
Article5. Marciano MA, Costa RM, Camilleri J, Mondelli RF, Guimarães BM, Duarte MA. Assessment of color stability of white mineral trioxide aggregate angelus and bismuth oxide in contact with tooth structure. J Endod. 2014; 40:1235–1240. PMID: 25069940.
Article6. Możyńska J, Metlerski M, Lipski M, Nowicka A. Tooth discoloration induced by different calcium silicate-based cements: a systematic review of in vitro studies. J Endod. 2017; 43:1593–1601. PMID: 28864217.
Article7. Rajasekharan S, Martens LC, Cauwels RG, Anthonappa RP, Verbeeck RM. Biodentine™ material characteristics and clinical applications: a 3 year literature review and update. Eur Arch Paediatr Dent. 2018; 19:1–22. PMID: 29372451.
Article8. Vidal K, Martin G, Lozano O, Salas M, Trigueros J, Aguilar G. Apical closure in apexification: a review and case report of apexification treatment of an immature permanent tooth with Biodentine. J Endod. 2016; 42:730–734. PMID: 26994597.
Article9. Hachmeister DR, Schindler WG, Walker WA 3rd, Thomas DD. The sealing ability and retention characteristics of mineral trioxide aggregate in a model of apexification. J Endod. 2002; 28:386–390. PMID: 12033201.
Article10. Yilmaz Z, Küçükkaya Eren S, Uzunoğlu E, Görduysus M, Görduysus MÖ. Interaction of backfilling techniques and MTA plugs with additives: Fracture strength and adaptation analyses. Dent Mater J. 2017; 36:809–815. PMID: 28845036.
Article11. Kadić S, Baraba A, Miletić I, Ionescu A, Brambilla E, Ivanišević Malčić A, Gabrić D. Push-out bond strength of three different calcium silicate-based root-end filling materials after ultrasonic retrograde cavity preparation. Clin Oral Investig. 2018; 22:1559–1565.
Article12. Tran D, He J, Glickman GN, Woodmansey KF. Comparative analysis of calcium silicate-based root filling materials using an open apex model. J Endod. 2016; 42:654–658. PMID: 26925519.
Article13. Araújo AC, Nunes E, Fonseca AA, Cortes MI, Horta MC, Silveira FF. Influence of smear layer removal and application mode of MTA on the marginal adaptation in immature teeth: a SEM analysis. Dent Traumatol. 2013; 29:212–217. PMID: 22788690.
Article14. Bidar M, Disfani R, Gharagozloo S, Khoynezhad S, Rouhani A. Medication with calcium hydroxide improved marginal adaptation of mineral trioxide aggregate apical barrier. J Endod. 2010; 36:1679–1682. PMID: 20850677.
Article15. López-García S, Pecci-Lloret MP, Pecci-Lloret MR, Oñate-Sánchez RE, García-Bernal D, Castelo-Baz P, Rodríguez-Lozano FJ, Guerrero-Gironés J. In vitro evaluation of the biological effects of ACTIVA Kids BioACTIVE Restorative, Ionolux, and Riva Light Cure on human dental pulp stem cells. Materials (Basel). 2019; 12:3694–3705.
Article16. Ertas H, Kucukyilmaz E, Ok E, Uysal B. Push-out bond strength of different mineral trioxide aggregates. Eur J Dent. 2014; 8:348–352. PMID: 25202215.
Article17. Shokouhinejad N, Yazdi KA, Nekoofar MH, Matmir S, Khoshkhounejad M. Effect of acidic environment on dislocation resistance of endosequence root repair material and mineral trioxide aggregate. J Dent (Tehran). 2014; 11:161–166. PMID: 24910691.18. Thompson JI, Gregson PJ, Revell PA. Analysis of push-out test data based on interfacial fracture energy. J Mater Sci Mater Med. 1999; 10:863–868. PMID: 15347966.19. Saghiri MA, Garcia-Godoy F, Gutmann JL, Lotfi M, Asatourian A, Ahmadi H. Push-out bond strength of a nano-modified mineral trioxide aggregate. Dent Traumatol. 2013; 29:323–327. PMID: 22882995.
Article20. Shokouhinejad N, Nekoofar MH, Iravani A, Kharrazifard MJ, Dummer PM. Effect of acidic environment on the push-out bond strength of mineral trioxide aggregate. J Endod. 2010; 36:871–874. PMID: 20416436.
Article21. Camilleri J. The chemical composition of mineral trioxide aggregate. J Conserv Dent. 2008; 11:141–143. PMID: 20351970.
Article22. Stefaneli Marques JH, Silva-Sousa YT, Rached-Júnior FJ, Macedo LM, Mazzi-Chaves JF, Camilleri J, Sousa-Neto MD. Push-out bond strength of different tricalcium silicate-based filling materials to root dentin. Braz Oral Res. 2018; 32:e18. PMID: 29538480.
Article23. Silva EJ, Carvalho NK, Zanon M, Senna PM, De-Deus G, Zuolo ML, Zaia AA. Push-out bond strength of MTA HP, a new high-plasticity calcium silicate-based cement. Braz Oral Res. 2016; 30:S1806-83242016000100269.
Article24. Bodanezi A, Carvalho N, Silva D, Bernardineli N, Bramante CM, Garcia RB, de Moraes IG. Immediate and delayed solubility of mineral trioxide aggregate and Portland cement. J Appl Oral Sci. 2008; 16:127–131. PMID: 19089204.
Article25. Bachoo IK, Seymour D, Brunton P. A biocompatible and bioactive replacement for dentine: is this a reality? The properties and uses of a novel calcium-based cement. Br Dent J. 2013; 214:E5. PMID: 23348482.
Article26. Stabholz A, Friedman S, Abed J. Marginal adaptation of retrograde fillings and its correlation with sealability. J Endod. 1985; 11:218–223. PMID: 3889216.
Article27. Johnson BR. Considerations in the selection of a root-end filling material. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87:398–404. PMID: 10225620.
Article28. Zafar M, Iravani M, Eghbal MJ, Asgary S. Coronal and apical sealing ability of a new endodontic cement. Iran Endod J. 2009; 4:15–19. PMID: 23864871.29. Bolhari B, Ashofteh Yazdi K, Sharifi F, Pirmoazen S. Comparative scanning electron microscopic study of the marginal adaptation of four root-end filling materials in presence and absence of blood. J Dent (Tehran). 2015; 12:226–234. PMID: 26622276.30. Shokouhinejad N, Nekoofar MH, Ashoftehyazdi K, Zahraee S, Khoshkhounejad M. Marginal adaptation of new bioceramic materials and mineral trioxide aggregate: a scanning electron microscopy study. Iran Endod J. 2014; 9:144–148. PMID: 24688585.31. Costa AT, Konrath F, Dedavid B, Weber JB, de Oliveira MG. Marginal adaptation of root-end filling materials: an in vitro study with teeth and replicas. J Contemp Dent Pract. 2009; 10:75–82.32. Badr AE. Marginal adaptation and cytotoxicity of bone cement compared with amalgam and mineral trioxide aggregate as root-end filling materials. J Endod. 2010; 36:1056–1060. PMID: 20478465.
Article33. Gondim E Jr, Zaia AA, Gomes BP, Ferraz CC, Teixeira FB, Souza-Filho FJ. Investigation of the marginal adaptation of root-end filling materials in root-end cavities prepared with ultrasonic tips. Int Endod J. 2003; 36:491–499. PMID: 12823705.
Article34. Teaford MF, Oyen OJ. Live primates and dental replication: new problems and new techniques. Am J Phys Anthropol. 1989; 80:73–81. PMID: 2679119.
Article35. Gondim E Jr, Gomes BP, Ferraz CC, Teixeira FB, Souza-Filho FJ. Effect of sonic and ultrasonic retrograde cavity preparation on the integrity of root apices of freshly extracted human teeth: scanning electron microscopy analysis. J Endod. 2002; 28:646–650. PMID: 12236308.
Article36. Bocker C, Kracker M, Rüssel C. Replica extraction method on nanostructured gold coatings and orientation determination combining SEM and TEM techniques. Microsc Microanal. 2014; 20:1654–1661. PMID: 25313465.
Article37. Küçükkaya Eren S, Görduysus MÖ, Şahin C. Sealing ability and adaptation of root-end filling materials in cavities prepared with different techniques. Microsc Res Tech. 2017; 80:756–762. PMID: 28271594.
Article38. Bolhari B, Yazdi KA, Sharifi F, Pirmoazen S. Comparative scanning electron microscopic study of the marginal adaptation of four root-end filling materials in presence and absence of blood. J Dent (Tehran). 2015; 12:226–234. PMID: 26622276.39. Torres FFE, Jacobs R, EzEldeen M, Guerreiro-Tanomaru JM, Dos Santos BC, Lucas-Oliveira É, Bonagamba TJ, Tanomaru-Filho M. Micro-computed tomography high resolution evaluation of dimensional and morphological changes of 3 root-end filling materials in simulated physiological conditions. J Mater Sci Mater Med. 2020; 31:14. PMID: 31965336.
Article40. Küçükkaya Eren S, Aksel H, Askerbeyli Örs S, Serper A, Koçak Y, Ocak M, Çelik HH. Obturation quality of calcium silicate-based cements placed with different techniques in teeth with perforating internal root resorption: a micro-computed tomographic study. Clin Oral Investig. 2019; 23:805–811.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of ultrasonic agitation on push-out bond strength and adaptation of root-end filling materials
- Bonding values of two contemporary ceramic inlay materials to dentin following simulated aging
- Push-out bond strengths of fiber-reinforced composite posts with various resin cements according to the root level
- Effect of curing methods of resin cements on bond strength and adhesive interface of post
- Effect of different adhesive systems and post surface treatments on the push-out bond strengths of fiber-reinforced post