Restor Dent Endod.
2021 Feb;46(1):e12. 10.5395/rde.2021.46.e12.
The effect of different confluence confirmation strategies on the obturation of Vertucci type II canal: micro-CT analysis
- Affiliations
-
- 1Department of Conservative Dentistry, Wonkwang University Daejeon Dental Hospital, Daejeon, Korea
- KMID: 2548047
- DOI: http://doi.org/10.5395/rde.2021.46.e12
Abstract
Objectives
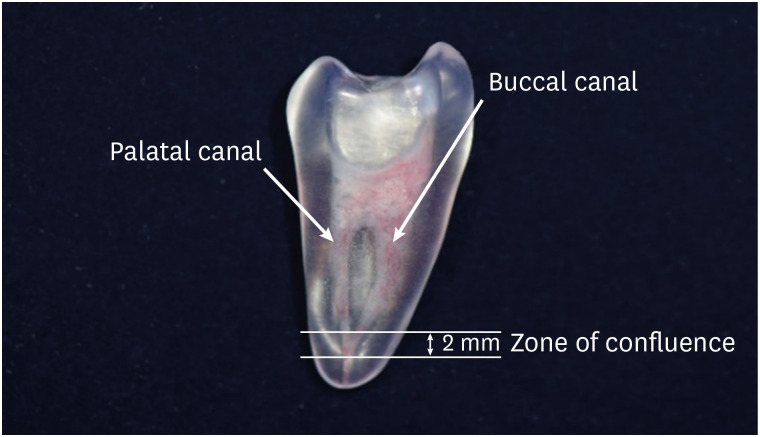
The present study aims to compare the obturation quality of 2 confluence confirmation techniques in artificial maxillary first premolars showing Vertucci type II root canal configuration.
Materials and Methods
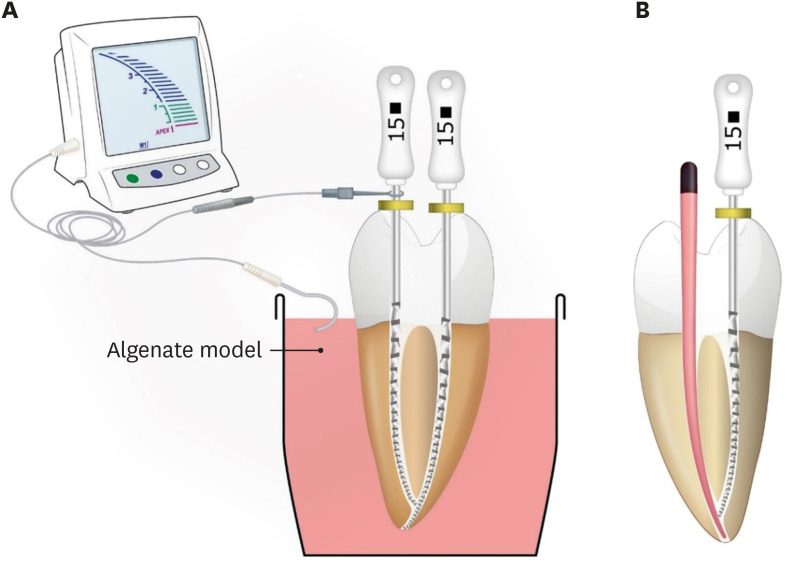
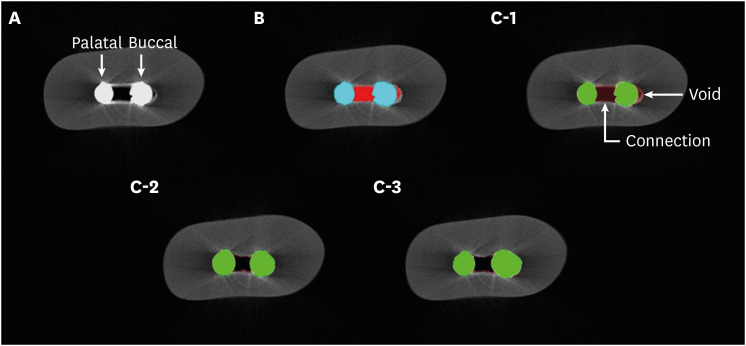
Thirty artificial maxillary premolars having Vertucci type II root canal configuration were made. They were divided into 3 groups according to the confluence confirmation technique as follows. Gutta-percha indentation (GPI) group (confluence confirmation using a gutta-percha cone and a K file); electronic apex locator (EAL) group (confluence confirmation using K files and EAL); and no confluence detection (NCD) group. In the GPI group and the EAL group, shaping and obturation were performed with the modified working length (WL). In the NCD group, shaping was performed without WL adjustment and obturation was carried out with an adjusted master cone. Micro-computed tomography was used before preparation and after obturation to calculate the percentage of gutta-percha occupied volume (%GPv) and the volume increase in the apical 4 mm. Data were analyzed using 1-way analysis of variance and post hoc Tukey's test.
Results
Statistically significant difference was not found in terms of the %GPv from the apex to apical 4 mm. However, the NCD group showed a statistically significant volume increase compared with the EAL group (p < 0.05).
Conclusions
In terms of gutta-percha occupied volume, no significant difference was observed among the 3 groups. Confluence confirmation using an EAL in teeth with Vertucci type II configuration showed less volume increase during canal shaping compared with no confluence confirmation.
Figure
Reference
-
1. Whitworth J. Methods of filling root canals: principles and practices. Endod Topics. 2005; 12:2–24.
Article2. Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984; 58:589–599. PMID: 6595621.
Article3. Gambarini G, Piasecki L, Ropini P, Miccoli G, Nardo DD, Testarelli L. Cone-beam computed tomographic analysis on root and canal morphology of mandibular first permanent molar among multiracial population in Western European population. Eur J Dent. 2018; 12:434–438. PMID: 30147412.
Article4. Chaparro AJ, Segura JJ, Guerrero E, Jiménez-Rubio A, Murillo C, Feito JJ. Number of roots and canals in maxillary first premolars: study of an Andalusian population. Endod Dent Traumatol. 1999; 15:65–67. PMID: 10379274.
Article5. Teixeira FB, Sano CL, Gomes BP, Zaia AA, Ferraz CC, Souza-Filho FJ. A preliminary in vitro study of the incidence and position of the root canal isthmus in maxillary and mandibular first molars. Int Endod J. 2003; 36:276–280. PMID: 12702122.
Article6. Alves FR, Andrade-Junior CV, Marceliano-Alves MF, Pérez AR, Rôças IN, Versiani MA, Sousa-Neto MD, Provenzano JC, Siqueira JF Jr. Adjunctive steps for disinfection of the mandibular molar root canal system: a correlative bacteriologic, micro-computed tomography, and cryopulverization approach. J Endod. 2016; 42:1667–1672. PMID: 27641947.
Article7. Keleş A, Alçin H, Sousa-Neto MD, Versiani MA. Supplementary steps for removing hard tissue debris from isthmus-containing canal systems. J Endod. 2016; 42:1677–1682. PMID: 27623498.
Article8. Versiani MA, Alves FR, Andrade-Junior CV, Marceliano-Alves MF, Provenzano JC, Rôças IN, Sousa-Neto MD, Siqueira JF Jr. Micro-CT evaluation of the efficacy of hard-tissue removal from the root canal and isthmus area by positive and negative pressure irrigation systems. Int Endod J. 2016; 49:1079–1087. PMID: 26459183.
Article9. Kim S, Jung H, Kim S, Shin SJ, Kim E. The influence of an isthmus on the outcomes of surgically treated molars: a retrospective study. J Endod. 2016; 42:1029–1034. PMID: 27238415.
Article10. Keleş A, Torabinejad M, Keskin C, Sah D, Uzun İ, Alçin H. Micro-CT evaluation of voids using two root filling techniques in the placement of MTA in mesial root canals of Vertucci type II configuration. Clin Oral Investig. 2018; 22:1907–1913.
Article11. Jho W, Park JW, Kim E, Song M, Seo DG, Yang DK, Shin SJ. Comparison of root canal filling quality by mineral trioxide aggregate and gutta percha cones/AH plus sealer. Dent Mater J. 2016; 35:644–650. PMID: 27477231.
Article12. Küçükkaya Eren S, Aksel H, Askerbeyli Örs S, Serper A, Koçak Y, Ocak M, Çelik HH. Obturation quality of calcium silicate-based cements placed with different techniques in teeth with perforating internal root resorption: a micro-computed tomographic study. Clin Oral Investig. 2019; 23:805–811.
Article13. de Pablo OV, Estevez R, Péix Sánchez M, Heilborn C, Cohenca N. Root anatomy and canal configuration of the permanent mandibular first molar: a systematic review. J Endod. 2010; 36:1919–1931. PMID: 21092807.
Article14. Kim S, Kim S, Park JW, Jung IY, Shin SJ. Comparison of the percentage of voids in the canal filling of a calcium silicate-based sealer and gutta percha cones using two obturation techniques. Materials (Basel). 2017; 10:1–9.
Article15. Moinzadeh AT, Zerbst W, Boutsioukis C, Shemesh H, Zaslansky P. Porosity distribution in root canals filled with gutta percha and calcium silicate cement. Dent Mater. 2015; 31:1100–1108. PMID: 26205383.
Article16. Hammad M, Qualtrough A, Silikas N. Evaluation of root canal obturation: a three-dimensional in vitro study. J Endod. 2009; 35:541–544. PMID: 19345801.
Article17. Kaufman AY, Keila S, Yoshpe M. Accuracy of a new apex locator: an in vitro study. Int Endod J. 2002; 35:186–192. PMID: 11843975.18. Jeong JW, DeGraft-Johnson A, Dorn SO, Di Fiore PM. Dentinal tubule penetration of a calcium silicate-based root canal sealer with different obturation methods. J Endod. 2017; 43:633–637. PMID: 28216267.
Article19. Keleş A, Alcin H, Kamalak A, Versiani MA. Micro-CT evaluation of root filling quality in oval-shaped canals. Int Endod J. 2014; 47:1177–1184. PMID: 24527697.20. Senia ES, Marshall FJ, Rosen S. The solvent action of sodium hypochlorite on pulp tissue of extracted teeth. Oral Surg Oral Med Oral Pathol. 1971; 31:96–103. PMID: 5275511.
Article21. Wu M, van der Sluis LW, Wesselink PR. A preliminary study of the percentage of gutta-percha-filled area in the apical canal filled with vertically compacted warm gutta-percha. Int Endod J. 2002; 35:527–535. PMID: 12190910.
Article22. Peters OA. Current challenges and concepts in the preparation of root canal systems: a review. J Endod. 2004; 30:559–567. PMID: 15273636.
Article23. Eleftheriadis GI, Lambrianidis TP. Technical quality of root canal treatment and detection of iatrogenic errors in an undergraduate dental clinic. Int Endod J. 2005; 38:725–734. PMID: 16164687.
Article24. Hülsmann M, Peters OA, Dummer PM. Mechanical preparation of root canals: shaping goals, techniques and means. Endod Topics. 2005; 10:30–76.
Article25. Schäfer E, Dammaschke T. Development and sequelae of canal transportation. Endod Topics. 2006; 15:75–90.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of mesial root canal configuration of mandibular first molars using micro-computed tomography
- Bacterial leakage and micro-computed tomography evaluation in round-shaped canals obturated with bioceramic cone and sealer using matched single cone technique
- Analysis of root number and canal morphology of maxillary premolars using cone-beam computed tomography
- Micro-computed tomographic evaluation of a new system for root canal filling using calcium silicatebased root canal sealers
- Comparison of sealing ability of different obturation techniques in type II root canals