J Korean Med Sci.
2023 Nov;38(43):e352. 10.3346/jkms.2023.38.e352.
Comparative Analysis of Olfactory and Gustatory Function of Patients With COVID-19 Olfactory Dysfunction and Non-COVID-19 Postinfectious Olfactory Dysfunction
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Konkuk University Medical Center, Konkuk University College of Medicine, Seoul, Korea
- 2Korea mRNA Vaccine Initiative, Gachon University, Seongnam, Korea
- KMID: 2547965
- DOI: http://doi.org/10.3346/jkms.2023.38.e352
Abstract
- Background
Coronavirus disease 2019 (COVID-19) is known to have a high incidence of loss of smell and taste. However, studies in the early stages of the COVID-19 pandemic have evaluated these symptoms using subjective surveys and simple olfactory tests only. Hence, we compared the olfactory and gustatory characteristics of patient groups with COVID-19 olfactory dysfunction (C19OD) and non-COVID-19 postinfectious olfactory dysfunction (PIOD) using an objective olfactory test and evaluated the significance of olfactory training in both patient groups.
Methods
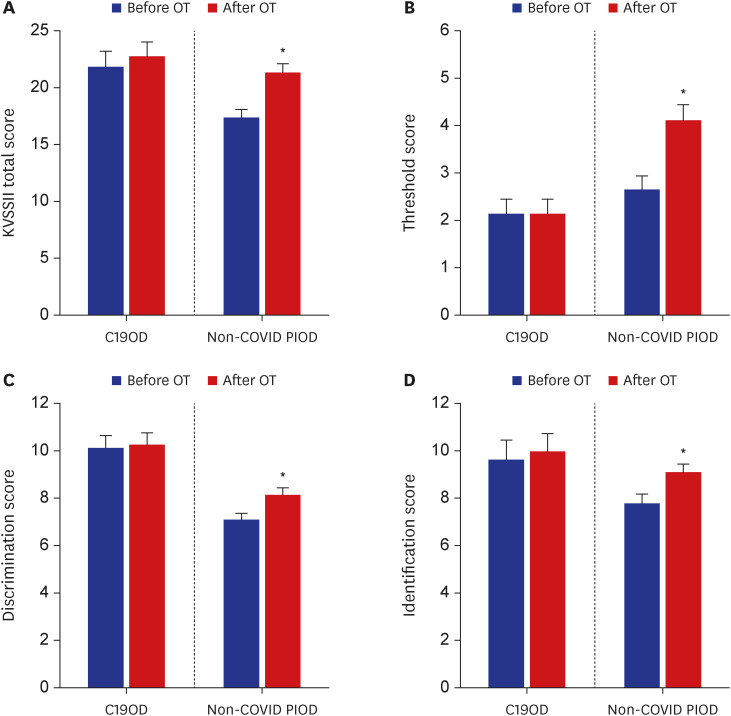
We retrospectively analyzed the medical records of 14 patients with a decreased sense of smell after having positive COVID-19 polymerase chain reaction results, and 56 patients with PIOD with no history of confirmed COVID-19. Participants were evaluated using the Korean version of the Sniffin’ stick (KVSS) II, and chemical gustometry and olfactory training was assessed during their first visit. Olfactory training was then re-evaluated after an average of 8 (± 6) weeks.
Results
The average age of participants in the C19OD group was lower than in those in the non-COVID-19 PIOD group. The proportion of men in the C19OD group was higher than in the non-COVID-19 PIOD group. At baseline assessment, the C19OD group had better olfactory and gustatory functions. After olfactory training, the non-COVID-19 PIOD patient group showed a significant increase in all KVSS II Total, T, D, and I scores, but there was a non-significant increase in all scores in the C19OD group.
Conclusion
The C19OD group had better olfactory and gustatory function than the nonCOVID-19 PIOD group at the initial assessment. After olfactory training, there was an increase in olfactory function test scores in both groups. Olfactory training may be helpful in C19OD, as in non-COVID-19 PIOD.
Figure
Reference
-
1. Tan BKJ, Han R, Zhao JJ, Tan NKW, Quah ESH, Tan CJ, et al. Prognosis and persistence of smell and taste dysfunction in patients with COVID-19: meta-analysis with parametric cure modelling of recovery curves. BMJ. 2022; 378:e069503. PMID: 35896188.
Article2. Chen L, Zhao J, Peng J, Li X, Deng X, Geng Z, et al. Detection of SARS-CoV-2 in saliva and characterization of oral symptoms in COVID-19 patients. Cell Prolif. 2020; 53(12):e12923. PMID: 33073910.
Article3. Chen M, Shen W, Rowan NR, Kulaga H, Hillel A, Ramanathan M Jr, et al. Elevated ACE-2 expression in the olfactory neuroepithelium: implications for anosmia and upper respiratory SARS-CoV-2 entry and replication. Eur Respir J. 2020; 56(3):2001948. PMID: 32817004.
Article4. Wang Z, Zhou J, Marshall B, Rekaya R, Ye K, Liu HX. SARS-CoV-2 receptor ACE2 Is enriched in a subpopulation of mouse tongue epithelial cells in nongustatory papillae but not in taste buds or embryonic oral epithelium. ACS Pharmacol Transl Sci. 2020; 3(4):749–758. PMID: 32821883.
Article5. Addison AB, Wong B, Ahmed T, Macchi A, Konstantinidis I, Huart C, et al. Clinical Olfactory Working Group consensus statement on the treatment of postinfectious olfactory dysfunction. J Allergy Clin Immunol. 2021; 147(5):1704–1719. PMID: 33453291.
Article6. Hummel T, Rissom K, Reden J, Hähner A, Weidenbecher M, Hüttenbrink KB. Effects of olfactory training in patients with olfactory loss. Laryngoscope. 2009; 119(3):496–499. PMID: 19235739.
Article7. Choi BY, Jeong H, Noh H, Park JY, Cho JH, Kim JK. Effects of olfactory training in patients with postinfectious olfactory dysfunction. Clin Exp Otorhinolaryngol. 2021; 14(1):88–92. PMID: 32575977.
Article8. Sorokowska A, Drechsler E, Karwowski M, Hummel T. Effects of olfactory training: a meta-analysis. Rhinology. 2017; 55(1):17–26. PMID: 28040824.
Article9. Park JY, Choi BY, Kim H, Jung T, Kim JK. Olfactory training assists in olfactory recovery after sinonasal surgery. Laryngoscope Investig Otolaryngol. 2022; 7(6):1733–1739.
Article10. Butowt R, Bilinska K, von Bartheld CS. Olfactory dysfunction in COVID-19: new insights into the underlying mechanisms. Trends Neurosci. 2023; 46(1):75–90. PMID: 36470705.
Article11. Khan M, Yoo SJ, Clijsters M, Backaert W, Vanstapel A, Speleman K, et al. Visualizing in deceased COVID-19 patients how SARS-CoV-2 attacks the respiratory and olfactory mucosae but spares the olfactory bulb. Cell. 2021; 184(24):5932–5949.e15. PMID: 34798069.
Article12. Kim JK, Han DH. COVID-19 and smell loss. Korean J Otorhinolaryngol-Head Neck Surg. 2020; 63(11):491–496.
Article13. Genetzaki S, Tsakiropoulou E, Nikolaidis V, Markou K, Konstantinidis I. Postinfectious olfactory dysfunction: oral steroids and olfactory training versus olfactory training alone: is there any benefit from steroids? ORL J Otorhinolaryngol Relat Spec. 2021; 83(6):387–394. PMID: 34107478.
Article14. Deems DA, Doty RL, Settle RG, Moore-Gillon V, Shaman P, Mester AF, et al. Smell and taste disorders, a study of 750 patients from the University of Pennsylvania Smell and Taste Center. Arch Otolaryngol Head Neck Surg. 1991; 117(5):519–528. PMID: 2021470.
Article15. Mott AE, Leopold DA. Disorders in taste and smell. Med Clin North Am. 1991; 75(6):1321–1353. PMID: 1943323.
Article16. Giacomelli A, Pezzati L, Conti F, Bernacchia D, Siano M, Oreni L, et al. Self-reported olfactory and taste disorders in patients with severe acute respiratory coronavirus 2 infection: a cross-sectional study. Clin Infect Dis. 2020; 71(15):889–890. PMID: 32215618.
Article17. Haehner A, Draf J, Dräger S, de With K, Hummel T. Predictive value of sudden olfactory loss in the diagnosis of COVID-19. ORL J Otorhinolaryngol Relat Spec. 2020; 82(4):175–180. PMID: 32526759.
Article18. Izquierdo-Dominguez A, Rojas-Lechuga MJ, Mullol J, Alobid I. Olfactory dysfunction in the COVID-19 outbreak. J Investig Allergol Clin Immunol. 2020; 30(5):317–326.19. Vandersteen C, Payne M, Dumas LÉ, Cancian É, Plonka A, D’Andréa G, et al. Olfactory training in post-COVID-19 persistent olfactory disorders: value normalization for threshold but not identification. J Clin Med. 2022; 11(12):3275. PMID: 35743346.
Article20. Heo SJ, Kim TH, Shin SH, Ye MK. Characteristics and prognosis of COVID-19 induced olfactory and gustatory dysfunction in Daegu. Korean J Otorhinolaryngol-Head Neck Surg. 2021; 64(10):720–725.
Article21. Cattaneo C, Pagliarini E, Mambrini SP, Tortorici E, Mené R, Torlasco C, et al. Changes in smell and taste perception related to COVID-19 infection: a case-control study. Sci Rep. 2022; 12(1):8192. PMID: 35581235.
Article22. Parma V, Ohla K, Veldhuizen MG, Niv MY, Kelly CE, Bakke AJ, et al. More than smell-COVID-19 is associated with severe impairment of smell, taste, and chemesthesis. Chem Senses. 2020; 45(7):609–622. PMID: 32564071.23. Asadi MM, Shankayi Z, Bahrami F, Mohammadzadeh T, Amini H, Naderi M. Quantitative analysis of taste disorder in COVID-19 patients, the hypersensitivity to salty quality. New Microbes New Infect. 2021; 43:100919. PMID: 34306710.
Article24. Hummel T, Lötsch J. Prognostic factors of olfactory dysfunction. Arch Otolaryngol Head Neck Surg. 2010; 136(4):347–351. PMID: 20403850.
Article25. Lechien JR, Vaira LA, Saussez S. Effectiveness of olfactory training in COVID-19 patients with olfactory dysfunction: a prospective study. Eur Arch Otorhinolaryngol. 2023; 280(3):1255–1263. PMID: 36153785.
Article26. Kattar N, Do TM, Unis GD, Migneron MR, Thomas AJ, McCoul ED. Olfactory training for postviral olfactory dysfunction: systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2021; 164(2):244–254. PMID: 32660334.
Article27. Denis F, Septans AL, Periers L, Maillard JM, Legoff F, Gurden H, et al. Olfactory training and visual stimulation assisted by a web application for patients with persistent olfactory dysfunction after SARS-CoV-2 infection: observational study. J Med Internet Res. 2021; 23(5):e29583. PMID: 34003765.28. Lee Y, Min P, Lee S, Kim SW. Prevalence and duration of acute loss of smell or taste in COVID-19 patients. J Korean Med Sci. 2020; 35(18):e174. PMID: 32383370.
Article29. Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 2020; 277(8):2251–2261. PMID: 32253535.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristics and Prognosis of COVID-19 Induced Olfactory and Gustatory Dysfunction in Daegu
- Contemporary Review of Olfactory Dysfunction in COVID-19
- A review on photobiomodulation therapy for olfactory dysfunction caused by COVID-19
- Regional and Chronological Variation of Chemosensory Dysfunction in COVID-19: a Meta-Analysis
- The Sniffing Bead System as a Useful Diagnostic Tool for Olfactory Dysfunction in COVID-19