Ewha Med J.
2023 Oct;46(4):e20. 10.12771/emj.2023.e20.
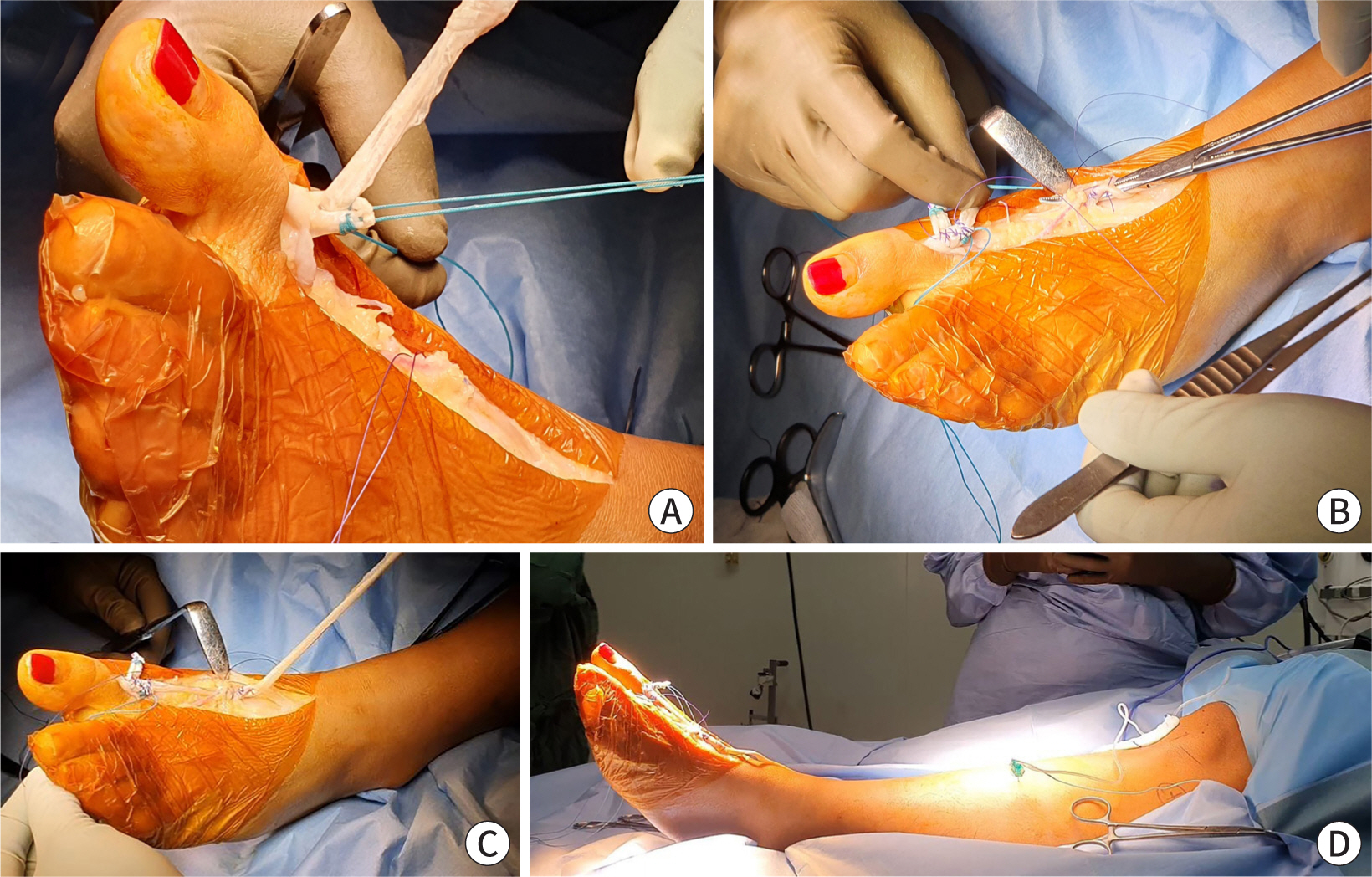
A 12-Week Rehabilitation Protocol for the Management of Chronic Extensor Hallucis Longus Rupture Repaired with an Autograft of the Semitendinosus Tendon
- Affiliations
-
- 1St. Carolus Hospital, Bone and Joint Centre, Jakarta, Indonesia
- 2Faculty of Medicine and Health Sciences, Atma Jaya Catholic University of Indonesia, Jakarta, Indonesia
- 3Department of Surgery, Faculty of Medicine, Universitas Trisakti, Jakarta, Indonesia
- KMID: 2547924
- DOI: http://doi.org/10.12771/emj.2023.e20
Abstract
- Traumatic rupture of the extensor hallucis longus (EHL) is an uncommon finding in an outpatient setting. Surgical repair is typically necessary, particularly in chronic conditions that have persisted for six weeks or more. While several studies have reported EHL repair using autograft tendons, rehabilitation regimes vary, and standardized protocols have not yet been established. This case report presents with an inability to extend her left great toe. She underwent tendon reconstruction with an autograft semitendinosus tendon. At an 8-week follow-up, the patient reported greatly improved outcomes on the American Orthopaedic Foot and Ankle Society, Foot and Ankle Ability Measure, Foot and Ankle Disability Index questionnaire. Full recovery was achieved 12 weeks after surgery. The use of autograft semitendinosus tendon repair for chronic EHL tendon rupture, in conjunction with rehabilitation program, can be expected to yield favorable results.
Figure
Reference
-
References
1. Wong JC, Daniel JN, Raikin SM. Repair of acute extensor hallucis longus tendon injuries: a retrospective review. Foot Ankle Spec. 2014; 7((1)):45–51. DOI: 10.1177/1938640013514271. PMID: 24334369.2. Kim WJ, Jung KJ, Ahn H, Yeo ED, Lee HS, Won SH, et al. Reconstruction of a neglected, extensor hallucis longus tendon rupture using interposed scar tissue: a case report and literature review. Int J Environ Res Public Health. 2021; 18((22)):12157. DOI: 10.3390/ijerph182212157. PMID: 34831920. PMCID: PMC8619473.3. Park HG, Lee BK, Sim JA. Autogenous graft repair using semitendinous tendon for a chronic multifocal rupture of the extensor hallucis longus tendon: a case report. Foot Ankle Int. 2003; 24((6)):506–508. DOI: 10.1177/107110070302400610. PMID: 12854673.4. Ferretti A, Conteduca F, Morelli F, Masi V. Regeneration of the semitendinosus tendon after its use in anterior cruciate ligament reconstruction: a histologic study of three cases. Am J Sports Med. 2002; 30((2)):204–207. DOI: 10.1177/03635465020300021001. PMID: 11912089.5. Chun DI, Lee JH, Cho J. Rupture of the extensor hallucis longus muscle secondary to repetitive overuse in a taekwondo athlete: a case report. J Am Podiatr Med Assoc. 2017; 107((5)):446–449. DOI: 10.7547/16-012. PMID: 29077497.6. Al-Qattan MM. Surgical treatment and results in 17 cases of open lacerations of the extensor hallucis longus tendon. J Plast Reconstr Aesthet Surg. 2007; 60((4)):360–367. DOI: 10.1016/j.bjps.2006.05.003. PMID: 17349589.7. Kurashige T. Chronic extensor hallucis longus tendon rupture treated with double-bundle autograft of extensor hallucis capsularis: a case report. SAGE Open Med Case Rep. 2019; 7:2050313X19841962. DOI: 10.1177/2050313X19841962. PMID: 31007922. PMCID: PMC6457017.8. Tuncer S, Aksu N. Isıklar U. Delayed rupture of the extensor hallucis longus and extensor digitorum communis tendons after breaching the anterior capsule with a radiofrequency probe during ankle arthroscopy: a case report. J Foot Ankle Surg. 2010; 49((5)):490.E1–490.E3. DOI: 10.1053/j.jfas.2010.05.003. PMID: 20576449.9. Lohrer H, Nauck T. Subcutaneous extensor hallucis longus tendon rupture: case report and literature review. Foot Ankle Int. 2012; 33((10)):905–911. DOI: 10.3113/FAI.2012.0905. PMID: 23050717.10. Bronner S, Ojofeitimi S, Rose D. Repair and rehabilitation of extensor hallucis longus and brevis tendon lacerations in a professional dancer. J Orthop Sports Phys Ther. 2008; 38((6)):362–370. DOI: 10.2519/jospt.2008.2749. PMID: 18515958.11. Joseph RM, Barhorst J. Surgical reconstruction and mobilization therapy for a retracted extensor hallucis longus laceration and tendon defect repaired by split extensor hallucis longus tendon lengthening and dermal scaffold augmentation. J Foot Ankle Surg. 2012; 51((4)):509–516. DOI: 10.1053/j.jfas.2012.04.018. PMID: 22658790.12. Refshauge KM, Taylor JL, McCloskey DI, Gianoutsos M, Mathews P, Fitzpatrick RC. Movement detection at the human big toe. J Physiol. 1998; 513((Pt 1)):307–314. DOI: 10.1111/j.1469-7793.1998.307by.x. PMID: 9782180. PMCID: PMC2231274.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of Chronic Extensor Hallucis Longus Tendon Rupture Using Interposed Scar Tissue: A Case Report
- Spontaneous Degenerative Rupture of Extensor Hallucis Longus Treated with a Split Tibialis Anterior Tendon Autograft: A Case Report
- Complete Rupture of the Extensor Hallucis Longus Tendon with Accessory Slip Mimicking a Partial Rupture: A Case Report
- Rupture of the Extensor Pollicis Longus after Fracture of the Distal end of the Radius: Report of 3 cases
- Delayed Rupture of the Extensor Pollicis Longus Tendon Following Intramedullary Nailing of Radial Shaft Fracture