Clin Endosc.
2023 Nov;56(6):802-811. 10.5946/ce.2022.211.
Covered self-expandable metallic stents versus plastic stents for endoscopic ultrasound-guided hepaticogastrostomy in patients with malignant biliary obstruction
- Affiliations
-
- 1Department of Hepatobiliary and Pancreatic Oncology, National Cancer Center Hospital East, Chiba, Japan
- 2Department of Gastroenterology, Jichi Medical University Saitama Medical Center, Saitama, Japan
- 3Department of Gastroenterology, Dokkyo Medical University Saitama Medical Center, Saitama, Japan
- 4Department of Gastroenterology, Toyooka Hospital, Hyogo, Japan
- 5Department of Gastroenterology, National Organization Disaster Medical Center, Tokyo, Japan
- 6Department of Gastroenterology, Fujigaoka Hospital, Showa University, Kanagawa, Japan
- 7Division of Gastroenterology, Department of Internal Medicine, University of Florida, Jacksonville, FL, USA
- KMID: 2547903
- DOI: http://doi.org/10.5946/ce.2022.211
Abstract
- Background/Aims
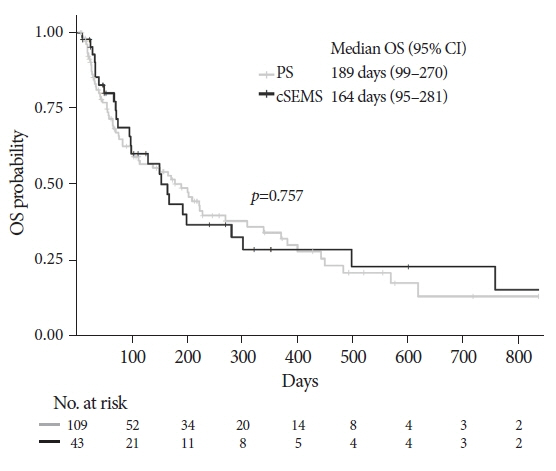
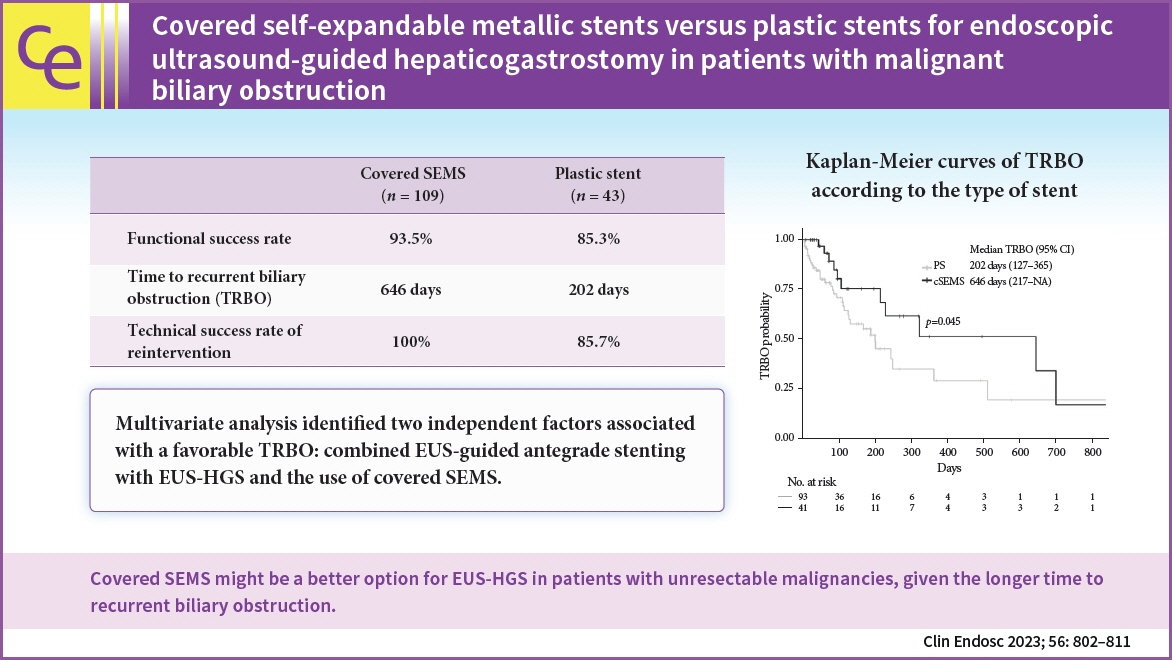
Covered self-expandable metallic stents (cSEMS) have become popular for endoscopic ultrasound-guided hepaticogastrostomy with transmural stenting (EUS-HGS). We compared the time to recurrent biliary obstruction (TRBO), complications, and reintervention rates between EUS-HGS using plastic stent (PS) and cSEMS in patients with unresectable malignancies at multicenter institutions in Japan.
Methods
Patients with unresectable malignant biliary obstruction who underwent EUS-HGS between April 2015 and July 2020 at any of the six participating facilities were enrolled. Primary endpoint: TRBO; secondary endpoints: rate of complications other than recurrent biliary obstruction and technical success rate of reintervention were evaluated.
Results
PS and cSEMS were used for EUS-HGS in 109 and 43 patients, respectively. The TRBO was significantly longer in the cSEMS group than in the PS group (646 vs. 202 days). Multivariate analysis identified two independent factors associated with a favorable TRBO: combined EUS-guided antegrade stenting with EUS-HGS and the use of cSEMS. No significant difference was observed in the rate of complications other than recurrent biliary obstruction between the two groups. The technical success rate of reintervention was 85.7% for PS and 100% for cSEMS (p=0.309).
Conclusions
cSEMS might be a better option for EUS-HGS in patients with unresectable malignancies, given the longer TRBO.
Keyword
Figure
Cited by 1 articles
-
The writing on the wall: self-expandable stents for endoscopic ultrasound-guided hepaticogastrostomy?
Hyung Ku Chon, Shayan Irani, Tae Hyeon Kim
Clin Endosc. 2023;56(6):741-743. doi: 10.5946/ce.2023.207.
Reference
-
1. Smith AC, Dowsett JF, Russell RC, et al. Randomised trial of endoscopic stenting versus surgical bypass in malignant low bile duct obstruction. Lancet. 1994; 344:1655–1660.
Article2. Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy. 2007; 39:1068–1071.
Article3. Itoi T, Ishii K, Sofuni A, et al. Single-balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video). Am J Gastroenterol. 2010; 105:93–99.
Article4. Nennstiel S, Weber A, Frick G, et al. Drainage-related complications in percutaneous transhepatic biliary drainage: an analysis over 10 years. J Clin Gastroenterol. 2015; 49:764–770.
Article5. Yamada A, Kogure H, Nakai Y, et al. Performance of a new short-type double-balloon endoscope with advanced force transmission and adaptive bending for pancreaticobiliary intervention in patients with surgically altered anatomy: a propensity-matched analysis. Dig Endosc. 2019; 31:86–93.
Article6. Lee TH, Choi JH, Park do H, et al. Similar efficacies of endoscopic ultrasound-guided transmural and percutaneous drainage for malignant distal biliary obstruction. Clin Gastroenterol Hepatol. 2016; 14:1011–1019.
Article7. Khashab MA, El Zein MH, Sharzehi K, et al. EUS-guided biliary drainage or enteroscopy-assisted ERCP in patients with surgical anatomy and biliary obstruction: an international comparative study. Endosc Int Open. 2016; 4:E1322–E1327.8. Jagielski M, Zieliński M, Piątkowski J, et al. Outcomes and limitations of endoscopic ultrasound-guided hepaticogastrostomy in malignant biliary obstruction. BMC Gastroenterol. 2021; 21:202.
Article9. Giovannini M. EUS-guided hepaticogastrostomy. Endosc Ultrasound. 2019; 8(Suppl 1):S35–S39.
Article10. Ogura T, Higuchi K. Endoscopic ultrasound-guided hepaticogastrostomy: technical review and tips to prevent adverse events. Gut Liver. 2021; 15:196–205.
Article11. Guo J, Giovannini M, Sahai AV, et al. A multi-institution consensus on how to perform EUS-guided biliary drainage for malignant biliary obstruction. Endosc Ultrasound. 2018; 7:356–365.12. Isayama H, Hamada T, Yasuda I, et al. TOKYO criteria 2014 for transpapillary biliary stenting. Dig Endosc. 2015; 27:259–264.13. Ogura T, Kitano M, Takenaka M, et al. Multicenter prospective evaluation study of endoscopic ultrasound-guided hepaticogastrostomy combined with antegrade stenting (with video). Dig Endosc. 2018; 30:252–259.
Article14. Davids PH, Groen AK, Rauws EA, et al. Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction. Lancet. 1992; 340:1488–1492.
Article15. Nakai Y, Sato T, Hakuta R, et al. Long-term outcomes of a long, partially covered metal stent for EUS-guided hepaticogastrostomy in patients with malignant biliary obstruction (with video). Gastrointest Endosc. 2020; 92:623–631.
Article16. Ogura T, Higuchi K. Technical tips for endoscopic ultrasound-guided hepaticogastrostomy. World J Gastroenterol. 2016; 22:3945–3951.
Article17. Yamamoto Y, Ogura T, Nishioka N, et al. Risk factors for adverse events associated with bile leak during EUS-guided hepaticogastrostomy. Endosc Ultrasound. 2020; 9:110–115.
Article18. Asai S, Takeshita K, Ichinona T, et al. A novel partially covered metallic stent with a 20-mm long distal bare portion for EUS-guided hepaticogastrostomy. VideoGIE. 2021; 6:322–324.
Article19. Okuno N, Hara K, Mizuno N, et al. Risks of transesophageal endoscopic ultrasonography-guided biliary drainage. Gastrointest Interv. 2017; 6:82–84.
Article20. Park DH, Jang JW, Lee SS, et al. EUS-guided biliary drainage with transluminal stenting after failed ERCP: predictors of adverse events and long-term results. Gastrointest Endosc. 2011; 74:1276–1284.
Article21. Honjo M, Itoi T, Tsuchiya T, et al. Safety and efficacy of ultra-tapered mechanical dilator for EUS-guided hepaticogastrostomy and pancreatic duct drainage compared with electrocautery dilator (with video). Endosc Ultrasound. 2018; 7:376–382.
Article22. Khashab MA, Messallam AA, Penas I, et al. International multicenter comparative trial of transluminal EUS-guided biliary drainage via hepatogastrostomy vs. choledochoduodenostomy approaches. Endosc Int Open. 2016; 4:E175–E181.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Stent Placement in the Palliation of Malignant Biliary Obstruction
- Current Status of Biliary Metal Stents
- Endoscopic Reintervention for Recurrence of Malignant Biliary Obstruction: Developing the Best Strategy
- Can Endoscopic Ultrasonography-guided Biliary Drainage Using Self-expandable Metal Stents in Malignant Distal Biliary Obstruction Be a Substitute When Endoscopic Retrograde Cholangiopancreatography Has Failed?
- Technical Tips and Issues of Biliary Stenting, Focusing on Malignant Hilar Obstruction