Clin Endosc.
2023 Nov;56(6):761-768. 10.5946/ce.2022.297.
Self-expandable metallic stent-induced esophagorespiratory fistulas in patients with advanced esophageal cancer
- Affiliations
-
- 1Department of Gastroenterology, Instituto do Câncer do Estado de São Paulo, Hospital das Clinicas da Faculdade de Medicina da Universidade de São Paulo, Sao Paulo, Brazil
- 2Division of Gastroenterology and Hepatology, University of North Carolina, Chapel Hill, NC, USA
- 3Laboratório de Investigações Médicas 37, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil
- 4National Council for Scientific and Technological Development, Brasília, Brazil
- KMID: 2547898
- DOI: http://doi.org/10.5946/ce.2022.297
Abstract
- Background/Aims
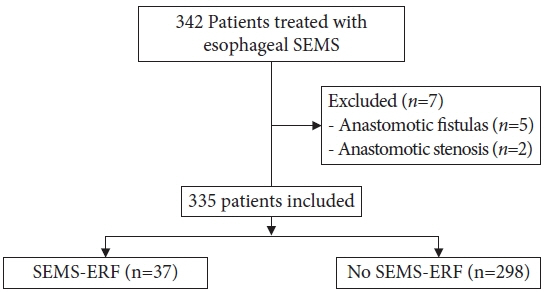
Self-expandable metallic stents (SEMSs) are widely adopted for the palliation of dysphagia in patients with malignant esophageal strictures. An important adverse event is the development of SEMS-induced esophagorespiratory fistulas (SEMS-ERFs). This study aimed to assess the risk factors related to the development of SEMS-ERF after SEMS placement in patients with esophageal cancer.
Methods
This retrospective study was performed at the Instituto do Cancer do Estado de São Paulo. All patients with malignant esophageal strictures who underwent esophageal SEMS placement between 2009 and 2019 were included in the study.
Results
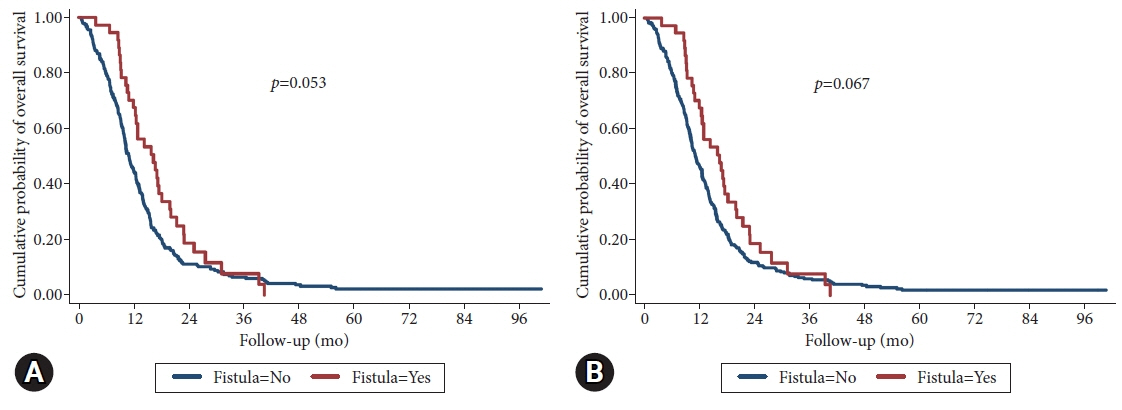
Of the 335 patients, 37 (11.0%) developed SEMS-ERF, with a median time of 129 days after SEMS placement. Stent flare of 28 mm (hazard ratio [HR], 2.05; 95% confidence interval [CI], 1.15–5.51; p=0.02) and post-stent chemotherapy (HR, 2.0; 95% CI, 1.01–4.00; p=0.05) were associated with an increased risk of developing SEMS-ERF, while lower-third tumors were a protective factor (HR, 0.5; 95% CI, 0.26–0.85; p=0.01). No difference was observed in overall survival.
Conclusions
The incidence of SEMS-ERFs was 11%, with a median time of 129 days after SEMS placement. Post-stent chemotherapy and a 28 mm stent flare were associated with a higher risk of SEMS-ERF.
Figure
Cited by 1 articles
-
How to reduce fistula formation after self-expandable metallic stent insertion for treating malignant esophageal stricture?
Kwang Bum Cho
Clin Endosc. 2023;56(6):735-737. doi: 10.5946/ce.2023.257.
Reference
-
1. Napier KJ, Scheerer M, Misra S. Esophageal cancer: a review of epidemiology, pathogenesis, staging workup and treatment modalities. World J Gastrointest Oncol. 2014; 6:112–120.
Article2. Parker RK, White RE, Topazian M, et al. Stents for proximal esophageal cancer: a case-control study. Gastrointest Endosc. 2011; 73:1098–1105.
Article3. Medeiros VS, Martins BC, Lenz L, et al. Adverse events of self-expandable esophageal metallic stents in patients with long-term survival from advanced malignant disease. Gastrointest Endosc. 2017; 86:299–306.
Article4. Homann N, Noftz MR, Klingenberg-Noftz RD, et al. Delayed complications after placement of self-expanding stents in malignant esophageal obstruction: treatment strategies and survival rate. Dig Dis Sci. 2008; 53:334–340.
Article5. Lenz CJ, Bick BL, Katzka D, et al. Esophagorespiratory fistulas: survival and outcomes of treatment. J Clin Gastroenterol. 2018; 52:131–136.6. Bick BL, Song LM, Buttar NS, et al. Stent-associated esophagorespiratory fistulas: incidence and risk factors. Gastrointest Endosc. 2013; 77:181–189.
Article7. Nagaraja V, Cox MR, Eslick GD. Safety and efficacy of esophageal stents preceding or during neoadjuvant chemotherapy for esophageal cancer: a systematic review and meta-analysis. J Gastrointest Oncol. 2014; 5:119–126.8. Sreedharan A, Harris K, Crellin A, et al. Interventions for dysphagia in oesophageal cancers. Cochrane Database Syst Rev. 2009; (4):CD005048.9. Raijman I, Siddique I, Ajani J, et al. Palliation of malignant dysphagia and fistulae with coated expandable metal stents: experience with 101 patients. Gastrointest Endosc. 1998; 48:172–179.
Article10. Chen YH, Li SH, Chiu YC, et al. Comparative study of esophageal stent and feeding gastrostomy/jejunostomy for tracheoesophageal fistula caused by esophageal squamous cell carcinoma. PLoS One. 2012; 7:e42766.
Article11. Na HK, Song HY, Kim JH, et al. How to design the optimal self-expandable oesophageal metallic stents: 22 years of experience in 645 patients with malignant strictures. Eur Radiol. 2013; 23:786–796.
Article12. Ross WA, Alkassab F, Lynch PM, et al. Evolving role of self-expanding metal stents in the treatment of malignant dysphagia and fistulas. Gastrointest Endosc. 2007; 65:70–76.
Article13. Ribeiro MS, da Costa Martins B, Simas de Lima M, et al. Self-expandable metal stent for malignant esophagorespiratory fistula: predictive factors associated with clinical failure. Gastrointest Endosc. 2018; 87:390–396.
Article14. Bethge N, Sommer A, Gross U, et al. Human tissue responses to metal stents implanted in vivo for the palliation of malignant stenoses. Gastrointest Endosc. 1996; 43:596–602.
Article15. Javed A, Pal S, Dash NR, et al. Palliative stenting with or without radiotherapy for inoperable esophageal carcinoma: a randomized trial. J Gastrointest Cancer. 2012; 43:63–69.
Article16. Park JY, Shin JH, Song HY, et al. Airway complications after covered stent placement for malignant esophageal stricture: special reference to radiation therapy. AJR Am J Roentgenol. 2012; 198:453–459.
Article17. Kim KY, Tsauo J, Song HY, et al. Self-expandable metallic stent placement for the palliation of esophageal cancer. J Korean Med Sci. 2017; 32:1062–1071.
Article18. Nishimura Y, Nagata K, Katano S, et al. Severe complications in advanced esophageal cancer treated with radiotherapy after intubation of esophageal stents: a questionnaire survey of the Japanese Society for Esophageal Diseases. Int J Radiat Oncol Biol Phys. 2003; 56:1327–1332.
Article19. Kinsman KJ, DeGregorio BT, Katon RM, et al. Prior radiation and chemotherapy increase the risk of life-threatening complications after insertion of metallic stents for esophagogastric malignancy. Gastrointest Endosc. 1996; 43:196–203.
Article20. Spaander MC, Baron TH, Siersema PD, et al. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016; 48:939–948.
Article21. Machado AA, da Costa Martins B, Lima GR, et al. Impact of radiotherapy (RT) on adverse events of self-expanding metallic stents (SEMS) in patients with esophageal cancer. Gastrointest Endosc. 2020; 91:AB149.22. Homs MY, Hansen BE, van Blankenstein M, et al. Prior radiation and/or chemotherapy has no effect on the outcome of metal stent placement for oesophagogastric carcinoma. Eur J Gastroenterol Hepatol. 2004; 16:163–170.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Self-expandable Metallic Stents for Palliative Treatment of Malignant Esophagogastric Strictures: Experiences in 103 Patients
- Self-Expandable Metallic Stent Placement for the Palliation of Esophageal Cancer
- Treatment of Esophagorespiratory Fistulas with Silicone-Coated Self-Expanding Metal Stents
- Silicone - Covered Self - Expandable Metal Stents for the Palliation of Malignant Esophageal Obstruction and Esophagorespiratory Fistulas
- Treatment of Esophagorespiratory Fistulas Associated with Esophageal Carcinoma: Effectiveness and Problems of a Modified Gianturco Stent