Cancer Res Treat.
2023 Oct;55(4):1281-1290. 10.4143/crt.2023.479.
Differential Perspectives by Specialty on Oligometastatic Colorectal Cancer: A Korean Oligometastasis Working Group’s Comparative Survey Study
- Affiliations
-
- 1Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Radiation Oncology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 3Department of Radiation Oncology, Chonnam National University Hwasun Hospital, Chonnam National University College of Medicine, Hwasun, Korea
- 4Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Surgery, St. Vincent`s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- 6Department of Surgery, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 7Proton Therapy Center, Research Institute and Hospital, National Cancer Center, Goyang, Korea
- 8Department of Radiation Oncology, Soonchunhyang University Seoul Hospital, Seoul, Korea
- 9Department of Radiation Oncology, St Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- KMID: 2547802
- DOI: http://doi.org/10.4143/crt.2023.479
Abstract
- Purpose
Despite numerous studies on the optimal treatments for oligometastatic disease (OMD), there is no established interdisciplinary consensus on its diagnosis or classification. This survey-based study aimed to analyze the differential opinions of colorectal surgeons and radiation oncologists regarding the definition and treatment of OMD from the colorectal primary.
Materials and Methods
A total of 141 participants were included in this study, consisting of 63 radiation oncologists (44.7%) and 78 colorectal surgeons (55.3%). The survey consisted of 19 questions related to OMD, and the responses were analyzed using the chi-square test to determine statistical differences between the specialties.
Results
The radiation oncologists chose “bone” more frequently compared to the colorectal surgeons (19.2% vs. 36.5%, p=0.022), while colorectal surgeons favored “peritoneal seeding” (26.9% vs. 9.5%, p=0.009). Regarding the number of metastatic tumors, 48.3% of colorectal surgeons responded that “irrelevant, if all metastatic lesions are amendable to local therapy”, while only 21.8% of radiation oncologist chose same answer. When asked about molecular diagnosis, most surgeons (74.8%) said it was important, but only 35.8% of radiation oncologists agreed.
Conclusion
This study demonstrates that although radiation oncologists and colorectal surgeons agreed on a majority of aspects such as diagnostic imaging, biomarker, systemic therapy, and optimal timing of OMD, they also had quite different perspectives on several aspects of OMD. Understanding these differences is crucial to achieving multidisciplinary consensus on the definition and optimal management of OMD.
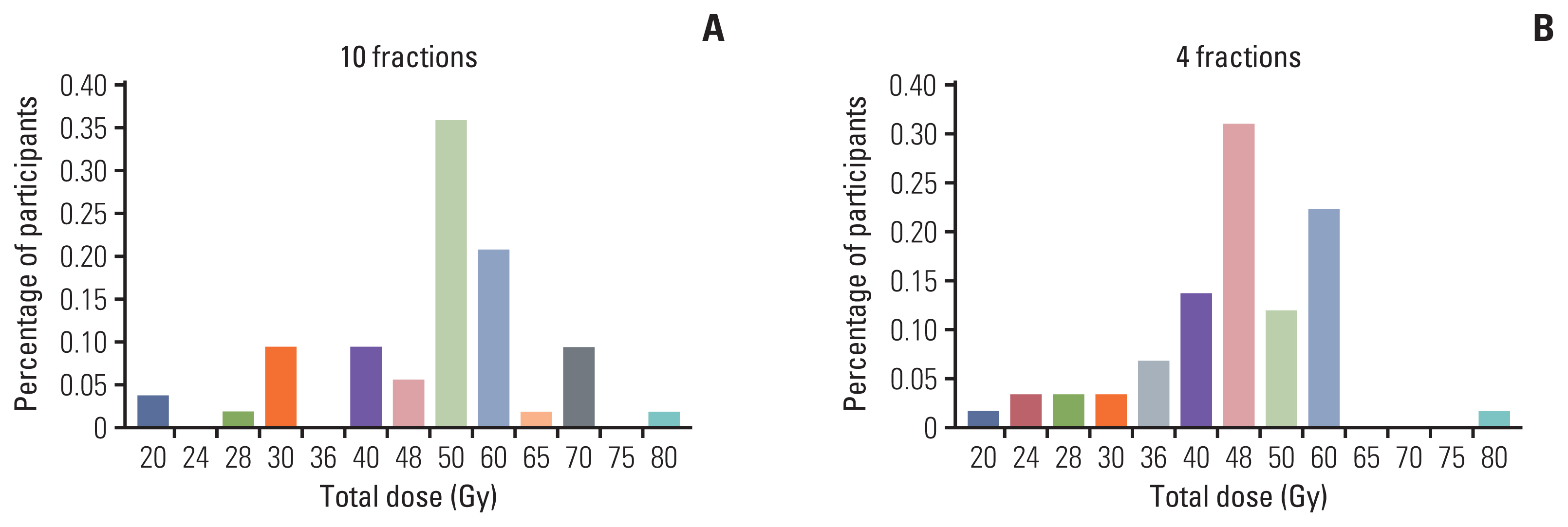
Figure
Reference
-
References
1. Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol. 1995; 13:8–10.2. Choti MA, Sitzmann JV, Tiburi MF, Sumetchotimetha W, Rangsin R, Schulick RD, et al. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg. 2002; 235:759–66.3. Kanas GP, Taylor A, Primrose JN, Langeberg WJ, Kelsh MA, Mowat FS, et al. Survival after liver resection in metastatic colorectal cancer: review and meta-analysis of prognostic factors. Clin Epidemiol. 2012; 4:283–301.4. Guckenberger M, Lievens Y, Bouma AB, Collette L, Dekker A, deSouza NM, et al. Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. Lancet Oncol. 2020; 21:e18–28.5. Willmann J, Vlaskou Badra E, Adilovic S, Ahmadsei M, Christ SM, van Timmeren JE, et al. Evaluation of the prognostic value of the ESTRO EORTC classification of oligometastatic disease in patients treated with stereotactic body radiotherapy: a retrospective single center study. Radiother Oncol. 2022; 168:256–64.6. Xi Y, Xu P. Global colorectal cancer burden in 2020 and projections to 2040. Transl Oncol. 2021; 14:101174.7. Hughes KS, Rosenstein RB, Songhorabodi S, Adson MA, Ilstrup DM, Fortner JG, et al. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of long-term survivors. Dis Colon Rectum. 1988; 31:1–4.8. Pastorino U, Buyse M, Friedel G, Ginsberg RJ, Girard P, Goldstraw P, et al. Long-term results of lung metastasectomy: prognostic analyses based on 5206 cases. J Thorac Cardiovasc Surg. 1997; 113:37–49.9. Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P, et al. Surgical resection of colorectal carcinoma metastases to the liver: a prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer. 1996; 77:1254–62.10. Shida D, Kobayashi H, Kameyama M, Hase K, Maeda K, Suto T, et al. Factors affecting R0 resection of colorectal cancer with synchronous peritoneal metastases: a multicenter prospective observational study by the Japanese Society for Cancer of the Colon and Rectum. Int J Clin Oncol. 2020; 25:330–7.11. Santini D, Tampellini M, Vincenzi B, Ibrahim T, Ortega C, Virzi V, et al. Natural history of bone metastasis in colorectal cancer: final results of a large Italian bone metastases study. Ann Oncol. 2012; 23:2072–7.12. Christensen TD, Jensen SG, Larsen FO, Nielsen DL. Systematic review: incidence, risk factors, survival and treatment of bone metastases from colorectal cancer. J Bone Oncol. 2018; 13:97–105.13. Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016; 27:1386–422.14. O’Cathail SM, Smith T, Owens R, Zeniou A, Tsang Y, Holyoake DL, et al. Superior outcomes of nodal metastases compared to visceral sites in oligometastatic colorectal cancer treated with stereotactic ablative radiotherapy. Radiother Oncol. 2020; 151:280–6.15. Kalapurackal Mathai V, Aung SY, Wong V, Dunn C, Shapiro JD, Jalali A, et al. Outcomes of isolated distant lymph node metastases in colorectal cancer. J Clin Oncol. 2021; 39(3 Suppl):84.16. Lievens Y, Guckenberger M, Gomez D, Hoyer M, Iyengar P, Kindts I, et al. Defining oligometastatic disease from a radiation oncology perspective: an ESTRO-ASTRO consensus document. Radiother Oncol. 2020; 148:157–66.17. Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999; 230:309–18.18. Kim KY, Kim NK, Cha IH, Ahn JB, Choi JS, Choi GH, et al. Novel methods for clinical risk stratification in patients with colorectal liver metastases. Cancer Res Treat. 2015; 47:242–50.19. Taieb J, Zaanan A, Le Malicot K, Julie C, Blons H, Mineur L, et al. Prognostic effect of BRAF and KRAS mutations in patients with stage III colon cancer treated with leucovorin, fluorouracil, and oxaliplatin with or without cetuximab: a post hoc analysis of the PETACC-8 trial. JAMA Oncol. 2016; 2:643–53.20. Tan C, Du X. KRAS mutation testing in metastatic colorectal cancer. World J Gastroenterol. 2012; 18:5171–80.21. Vaughn CP, Zobell SD, Furtado LV, Baker CL, Samowitz WS. Frequency of KRAS, BRAF, and NRAS mutations in colorectal cancer. Genes Chromosomes Cancer. 2011; 50:307–12.22. Li Y, Xiao J, Zhang T, Zheng Y, Jin H. Analysis of KRAS, NRAS, and BRAF mutations, microsatellite instability, and relevant prognosis effects in patients with early colorectal cancer: a cohort study in East Asia. Front Oncol. 2022; 12:897548.23. Singh MP, Rai S, Pandey A, Singh NK, Srivastava S. Molecular subtypes of colorectal cancer: An emerging therapeutic opportunity for personalized medicine. Genes Dis. 2021; 8:133–45.24. Pitroda SP, Khodarev NN, Huang L, Uppal A, Wightman SC, Ganai S, et al. Integrated molecular subtyping defines a curable oligometastatic state in colorectal liver metastasis. Nat Commun. 2018; 9:1793.25. Jethwa KR, Jang S, Mullikin TC, Harmsen WS, Petersen MM, Olivier KR, et al. Association of tumor genomic factors and efficacy for metastasis-directed stereotactic body radiotherapy for oligometastatic colorectal cancer. Radiother Oncol. 2020; 146:29–36.26. Hong TS, Wo JY, Borger DR, Yeap BY, McDonnell EI, Willers H, et al. Phase II study of proton-based stereotactic body radiation therapy for liver metastases: importance of tumor genotype. J Natl Cancer Inst. 2017; 109:djx031.27. Jia-Mahasap B, Madla C, Sripan P, Chitapanarux I, Tharavichitkul E, Chakrabandhu S, et al. Stereotactic radiosurgery for limited brain metastasis using three different techniques: helical tomotherapy, volumetric modulated arc therapy, and cone-based LINAC radiosurgery. Radiat Oncol J. 2022; 40:232–41.28. Tsai CJ, Yang JT, Guttmann DM, Shaverdian N, Eng J, Yeh R, et al. Final analysis of consolidative use of radiotherapy to block (CURB) oligoprogression trial: a randomized study of stereotactic body radiotherapy for oligoprogressive metastatic lung and breast cancers. Int J Radiat Oncol Biol Phys. 2022; 114:P1061.29. Chmura SJ, Winter KA, Woodward WA, Borges VF, Salama JK, Al-Hallaq HA, et al. NRG-BR002: a phase IIR/III trial of standard of care systemic therapy with or without stereotactic body radiotherapy (SBRT) and/or surgical resection (SR) for newly oligometastatic breast cancer (NCT02364557). J Clin Oncol. 2022; 40(16 Suppl):1007.30. Kim E, Jang WI, Yang K, Kim MS, Yoo HJ, Paik EK, et al. Clinical utilization of radiation therapy in Korea between 2017 and 2019. Radiat Oncol J. 2022; 40:251–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Genomic Characteristics and the Potential Clinical Implications in Oligometastatic Non–Small Cell Lung Cancer
- Radiation Oncologists’ Perspectives on Oligometastatic Disease: A Korean Survey Study
- The role of metastasis-directed therapy and local therapy of the primary tumor in the management of oligometastatic prostate cancer
- Long-term survival after multimodal treatment involving radiotherapy for huge hepatocellular carcinoma with oligometastasis: a case report
- Top Ten Lessons Learned from Trials in Oligometastatic Cancers