J Korean Assoc Oral Maxillofac Surg.
2023 Oct;49(5):252-261. 10.5125/jkaoms.2023.49.5.252.
Extraction of mandibular third molars: relationship of preoperative anxiety with body mass index, serum high-sensitivity C-reactive protein levels, and visual analog scale scores and predictors of postoperative complications
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Kyung Hee University Dental Hospital at Gangdong, Seoul, Korea
- 2Department of Oral and Maxillofacial Surgery, College of Dentistry, Kyung Hee University, Seoul, Korea
- KMID: 2547569
- DOI: http://doi.org/10.5125/jkaoms.2023.49.5.252
Abstract
Objectives
Patients undergoing oral surgery exhibit high anxiety, which may elevate their cortisol levels and affect postoperative recovery. Overweight patients are often encountered in the dental clinic due to the increasing prevalence of overweight. We aimed to investigate the relationships between preoperatively assessed body mass index (BMI), serum cortisol and high-sensitivity C-reactive protein (hs-CRP) levels, and visual analog scale (VAS) scores and preoperative anxiety in patients undergoing mandibular third molar (MM3) extraction and to identify predictors of postoperative complications.
Patients and Methods
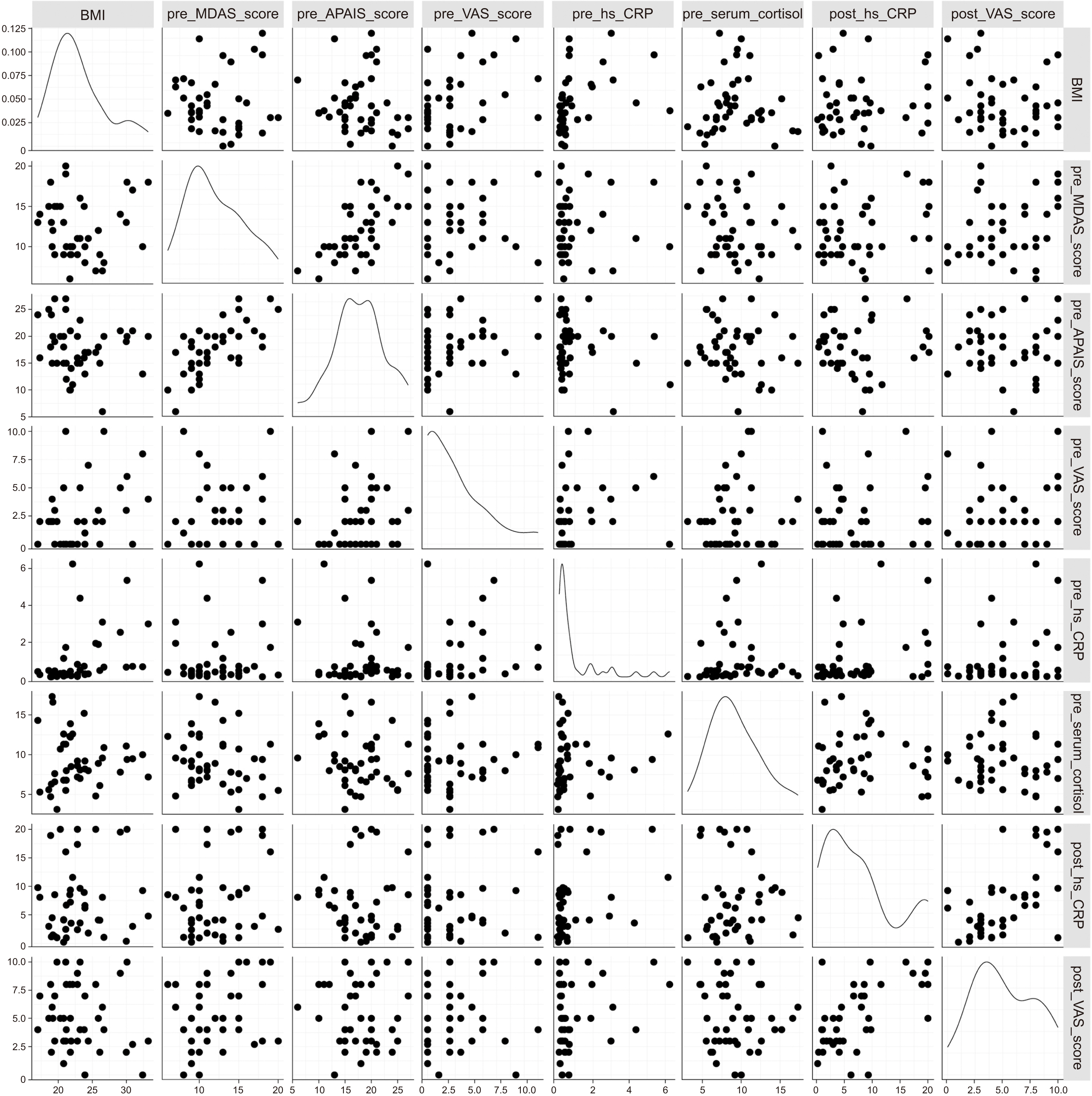
We analyzed 43 patients (age, 20-42 years) undergoing MM3 extraction. At the first visit, patients completed the Modified Dental Anxiety Scale (MDAS) and Amsterdam Preoperative Anxiety and Information Scale (APAIS) questionnaires. Their BMI and VAS scores were also calculated. The participants underwent blood tests 1 hour before MM3 extraction. On the first postoperative day, the participants’ VAS scores and serum hs-CRP levels were reevaluated.
Results
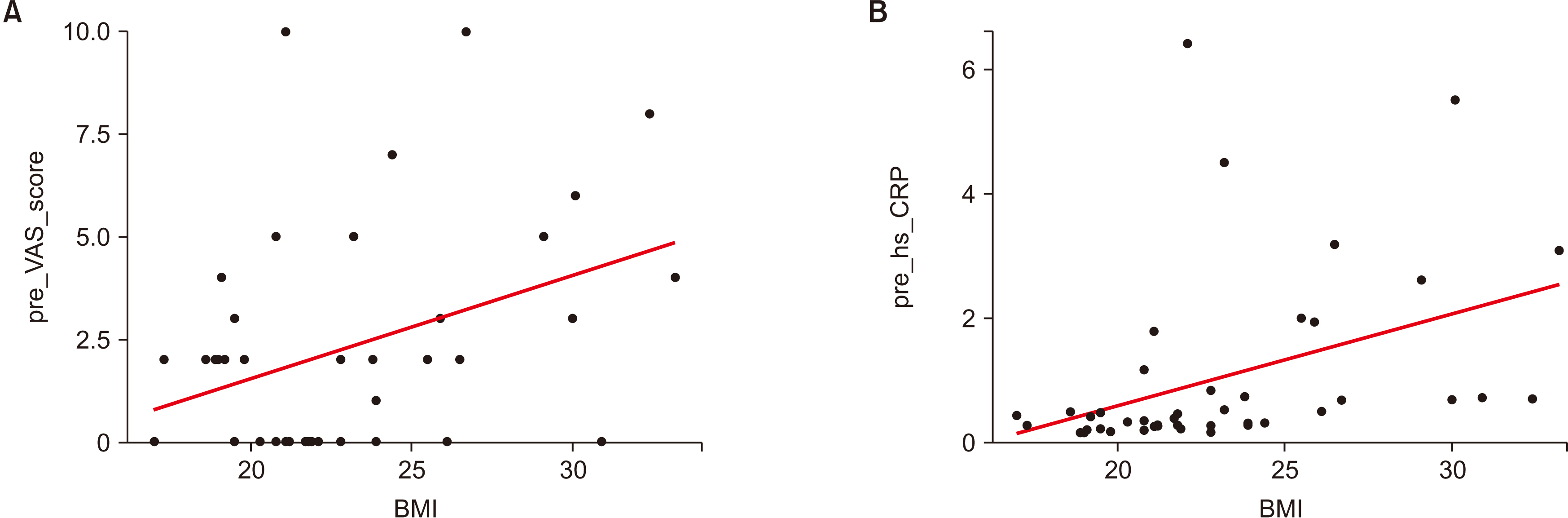
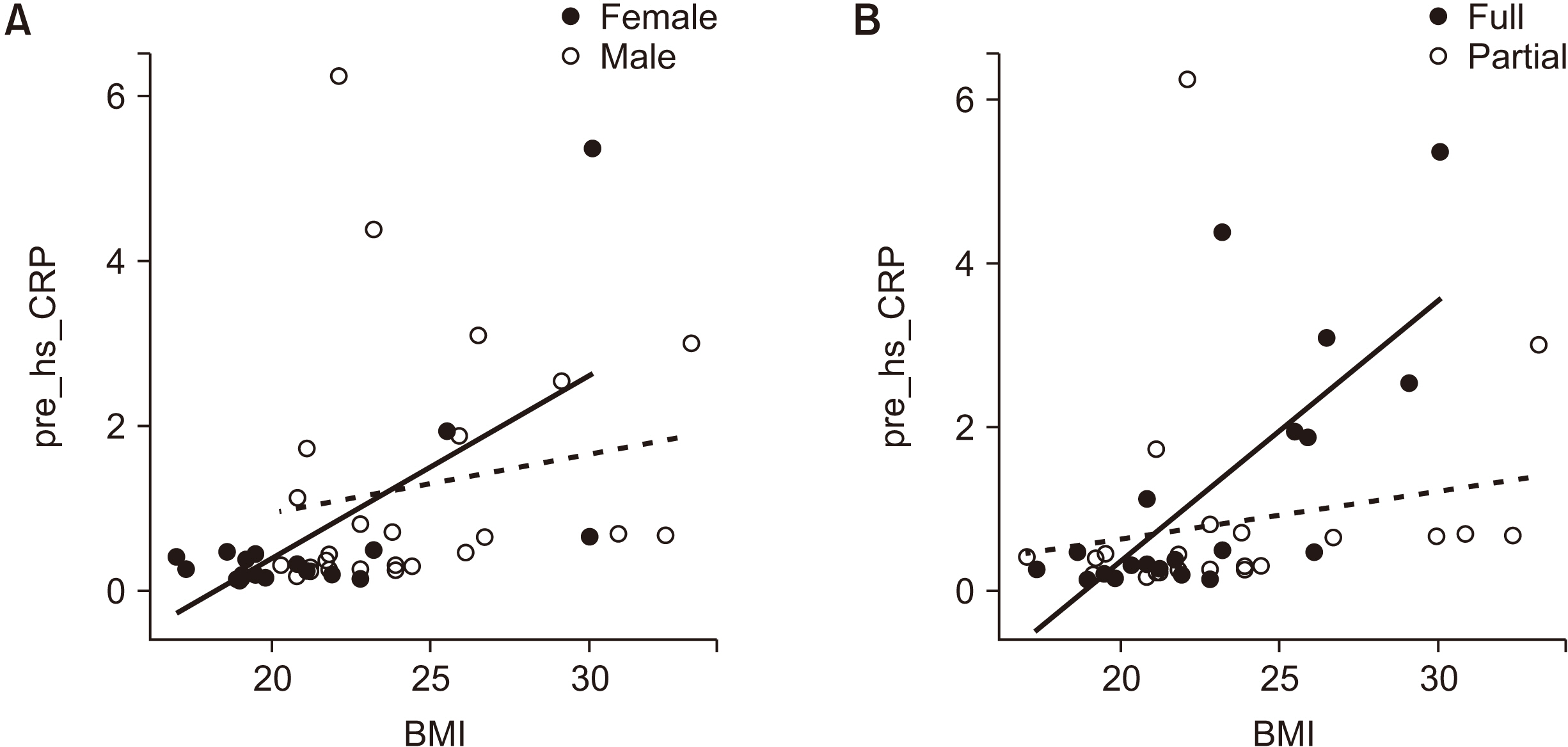
We found that BMI was significantly correlated with preoperative VAS scores. Further, BMI and preoperative hs-CRP levels were significantly correlated among women and patients undergoing extractions of fully impacted MM3s. No correlations were found between serum cortisol and other variables. The preoperative MDAS and VAS scores were significantly positively correlated, especially among patients undergoing extractions of fully impacted MM3s. Multiple linear regression showed that BMI and the eruption status of the MM3 were significant predictors of postoperative hsCRP levels and VAS scores, respectively.
Conclusion
In MM3 removals, patients with higher BMI showed elevated hs-CRP and higher VAS scores before surgery. Patients with higher anxiety among those undergoing extractions of fully impacted MM3s showed higher preoperative VAS scores. The two main predictors of postoperative complications were BMI and MM3 eruption status.
Keyword
Figure
Reference
-
References
1. Agras S, Sylvester D, Oliveau D. 1969; The epidemiology of common fears and phobia. Compr Psychiatry. 10:151–6. https://doi.org/10.1016/0010-440x(69)90022-4. DOI: 10.1016/0010-440X(69)90022-4. PMID: 5774552.
Article2. Tanidir AN, Atac MS, Karacelebi E. 2016; Informatıon given by multımedıa: influence on anxıety about extractıon of impacted wısdom teeth. Br J Oral Maxillofac Surg. 54:652–7. https://doi.org/10.1016/j.bjoms.2016.03.026. DOI: 10.1016/j.bjoms.2016.03.026. PMID: 27105893.
Article3. Earl P. 1994; Patients' anxieties with third molar surgery. Br J Oral Maxillofac Surg. 32:293–7. https://doi.org/10.1016/0266-4356(94)90049-3. DOI: 10.1016/0266-4356(94)90049-3. PMID: 7999736.
Article4. Kazancioglu HO, Tek M, Ezirganli S, Demirtas N. 2015; Does watching a video on third molar surgery increase patients' anxiety level? Oral Surg Oral Med Oral Pathol Oral Radiol. 119:272–7. https://doi.org/10.1016/j.oooo.2014.10.012. DOI: 10.1016/j.oooo.2014.10.012. PMID: 25561389.
Article5. Sbirkova T, Мassaldjieva R, Neychev D, Raycheva R. 2021; Anxiety and changes in physiological parameters during surgical procedures for removal of impacted mandibular third molars in young adults. J Int Dent Med Res. 14:221–7.6. Xu JL, Xia R. 2020; Influence factors of dental anxiety in patients with impacted third molar extractions and its correlation with postoperative pain: a prospective study. Med Oral Patol Oral Cir Bucal. 25:e714–9. https://doi.org/10.4317/medoral.23293. DOI: 10.4317/medoral.23293. PMID: 33037812. PMCID: PMC7648926.
Article7. George JM, Scott DS, Turner SP, Gregg JM. 1980; The effects of psychological factors and physical trauma on recovery from oral surgery. J Behav Med. 3:291–310. https://doi.org/10.1007/bf00845053. DOI: 10.1007/BF00845053. PMID: 7441729.
Article8. Vallerand WP, Vallerand AH, Heft M. 1994; The effects of postoperative preparatory information on the clinical course following third molar extraction. J Oral Maxillofac Surg. 52:1165–70. discussion 1170–1. https://doi.org/10.1016/0278-2391(94)90536-3. DOI: 10.1016/0278-2391(94)90536-3. PMID: 7965311.
Article9. Gao Q, Mok HP, Zhang HY, Qiu HL, Liu J, Chen ZR, et al. 2021; Inflammatory indicator levels in patients undergoing aortic valve replacement via median sternotomy with preoperative anxiety and postoperative complications: a prospective cohort study. J Int Med Res. 49:300060520977417. https://doi.org/10.1177/0300060520977417. DOI: 10.1177/0300060520977417. PMID: 33535861. PMCID: PMC7869182.
Article10. Litt MD. 1996; A model of pain and anxiety associated with acute stressors: distress in dental procedures. Behav Res Ther. 34:459–76. https://doi.org/10.1016/0005-7967(96)00015-0. DOI: 10.1016/0005-7967(96)00015-0. PMID: 8687368.
Article11. Benjamins C, Asscheman H, Schuurs AH. 1992; Increased salivary cortisol in severe dental anxiety. Psychophysiology. 29:302–5. https://doi.org/10.1111/j.1469-8986.1992.tb01703.x. DOI: 10.1111/j.1469-8986.1992.tb01703.x. PMID: 1626040.
Article12. Krueger TH, Heller HW, Hauffa BP, Haake P, Exton MS, Schedlowski M. 2005; The dental anxiety scale and effects of dental fear on salivary cortisol. Percept Mot Skills. 100:109–17. https://doi.org/10.2466/pms.100.1.109-117. DOI: 10.2466/pms.100.1.109-117. PMID: 15773701.
Article13. Yfanti K, Kitraki E, Emmanouil D, Pandis N, Papagiannoulis L. 2014; Psychometric and biohormonal indices of dental anxiety in children. A prospective cohort study. Stress. 17:296–304. https://doi.org/10.3109/10253890.2014.918602. DOI: 10.3109/10253890.2014.918602. PMID: 24766350.
Article14. Preiss K, Brennan L, Clarke D. 2013; A systematic review of variables associated with the relationship between obesity and depression. Obes Rev. 14:906–18. https://doi.org/10.1111/obr.12052. DOI: 10.1111/obr.12052. PMID: 23809142.
Article15. Lykouras L, Michopoulos J. 2011; Anxiety disorders and obesity. Psychiatriki. 22:307–13.16. Tayefi M, Shafiee M, Kazemi-Bajestani SMR, Esmaeili H, Darroudi S, Khakpouri S, et al. 2017; Depression and anxiety both associate with serum level of hs-CRP: a gender-stratified analysis in a population-based study. Psychoneuroendocrinology. 81:63–9. https://doi.org/10.1016/j.psyneuen.2017.02.035. DOI: 10.1016/j.psyneuen.2017.02.035. PMID: 28419913.
Article17. Humphris GM, Dyer TA, Robinson PG. 2009; The modified dental anxiety scale: UK general public population norms in 2008 with further psychometrics and effects of age. BMC Oral Health. 9:20. https://doi.org/10.1186/1472-6831-9-20. DOI: 10.1186/1472-6831-9-20. PMID: 19709436. PMCID: PMC2743651.
Article18. Moerman N, van Dam FS, Muller MJ, Oosting H. 1996; The Amsterdam Preoperative Anxiety and Information Scale (APAIS). Anesth Analg. 82:445–51. https://doi.org/10.1097/00000539-199603000-00002. DOI: 10.1097/00000539-199603000-00002. PMID: 8623940.
Article19. Shin WJ, Kim YC, Yeom JH, Cho SY, Lee DH, Kim DW. 1999; The validity of Amsterdam Preoperative Anxiety Information Scale in the assessment of the preoperative anxiety - compared with hospital anxiety depression scale and visual analogue scale -. Korean J Anesthesiol. 37:179–87. https://doi.org/10.4097/kjae.1999.37.2.179. DOI: 10.4097/kjae.1999.37.2.179.
Article20. Granot M, Ferber SG. 2005; The roles of pain catastrophizing and anxiety in the prediction of postoperative pain intensity: a prospective study. Clin J Pain. 21:439–45. https://doi.org/10.1097/01.ajp.0000135236.12705.2d. DOI: 10.1097/01.ajp.0000135236.12705.2d. PMID: 16093750.
Article21. Zhao G, Ford ES, Dhingra S, Li C, Strine TW, Mokdad AH. 2009; Depression and anxiety among US adults: associations with body mass index. Int J Obes (Lond). 33:257–66. https://doi.org/10.1038/ijo.2008.268. DOI: 10.1038/ijo.2008.268. PMID: 19125163.
Article22. Gariepy G, Nitka D, Schmitz N. 2010; The association between obesity and anxiety disorders in the population: a systematic review and meta-analysis. Int J Obes (Lond). 34:407–19. https://doi.org/10.1038/ijo.2009.252. DOI: 10.1038/ijo.2009.252. PMID: 19997072.
Article23. Barry D, Pietrzak RH, Petry NM. 2008; Gender differences in associations between body mass index and DSM-IV mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Ann Epidemiol. 18:458–66. https://doi.org/10.1016/j.annepidem.2007.12.009. DOI: 10.1016/j.annepidem.2007.12.009. PMID: 18329894. PMCID: PMC2504706.
Article24. Scott KM, McGee MA, Wells JE, Oakley Browne MA. 2008; Obesity and mental disorders in the adult general population. J Psychosom Res. 64:97–105. https://doi.org/10.1016/j.jpsychores.2007.09.006. DOI: 10.1016/j.jpsychores.2007.09.006. PMID: 18158005.
Article25. Bankier B, Barajas J, Martinez-Rumayor A, Januzzi JL. 2008; Association between C-reactive protein and generalized anxiety disorder in stable coronary heart disease patients. Eur Heart J. 29:2212–7. https://doi.org/10.1093/eurheartj/ehn326. DOI: 10.1093/eurheartj/ehn326. PMID: 18603621.
Article26. Kim T, Ganocy SJ, Antonelli M, Einstadter D, Ballou S. 2017; Association of CRP with BMI in males and females. Arthritis Rheumatol. 69(Suppl 10):1954.27. Kandemir S, Okşan T, Alpöz AR, Ergezer G, Kabalak T. 1997; Salivary cortisol levels in children during dental treatment. J Marmara Univ Dent Fac. 2:639–42.28. Selimuzzaman SM, Begum N, Islam N, Begum S. 2007; Effects of surgical stress on serum cortisol level: a comparative study between elective and emergency surgery. J Bangladesh Soc Physiol. 2:28–33. DOI: 10.3329/jbsp.v2i0.981.
Article29. Manso Platero FJ, Calatayud Sierra J, Carrillo Baracaldo JS, Barbería Leache E, Zaragoza Rubira JR. 1989; [Anxiety, inflammation and duration of operation: is there a relationship?] . Av Odontoestomatol. 5:31–4. Spanish.30. Ozalp G, Sarioglu R, Tuncel G, Aslan K, Kadiogullari N. 2003; Preoperative emotional states in patients with breast cancer and postoperative pain. Acta Anaesthesiol Scand. 47:26–9. https://doi.org/10.1034/j.1399-6576.2003.470105.x. DOI: 10.1034/j.1399-6576.2003.470105.x. PMID: 12492793.
Article31. Feeney SL. 2004; The relationship between pain and negative affect in older adults: anxiety as a predictor of pain. J Anxiety Disord. 18:733–44. https://doi.org/10.1016/j.janxdis.2001.04.001. DOI: 10.1016/j.janxdis.2001.04.001. PMID: 15474849.
Article32. Martinez-Urrutia A. 1975; Anxiety and pain in surgical patients. J Consult Clin Psychol. 43:437–42. https://doi.org/10.1037/h0076898. DOI: 10.1037/h0076898. PMID: 1159142.
Article33. Kain ZN, Sevarino FB, Rinder C, Pincus S, Alexander GM, Ivy M, et al. 2001; Preoperative anxiolysis and postoperative recovery in women undergoing abdominal hysterectomy. Anesthesiology. 94:415–22. https://doi.org/10.1097/00000542-200103000-00009. DOI: 10.1097/00000542-200103000-00009. PMID: 11374599.
Article34. Kalkman JC, Visser K, Moen J, Bonsel JG, Grobbee ED, Moons MKG. 2003; Preoperative prediction of severe postoperative pain. Pain. 105:415–23. https://doi.org/10.1016/s0304-3959(03)00252-5. DOI: 10.1016/S0304-3959(03)00252-5. PMID: 14527702.
Article35. Chung F, Ritchie E, Su J. 1997; Postoperative pain in ambulatory surgery. Anesth Analg. 85:808–16. https://doi.org/10.1097/00000539-199710000-00017. DOI: 10.1097/00000539-199710000-00017. PMID: 9322460.
Article36. Dušková M, Vašáková J, Dušková J, Kaiferová J, Broukal Z, Stárka L. 2017; The role of stress hormones in dental management behavior problems. Physiol Res. 66(Suppl 3):S317–22. https://doi.org/10.33549/physiolres.933718. DOI: 10.33549/physiolres.933718. PMID: 28948815.
Article37. Brand HS. 1999; Anxiety and cortisol excretion correlate prior to dental treatment. Int Dent J. 49:330–6. https://doi.org/10.1111/j.1875-595x.1999.tb00533.x. DOI: 10.1111/j.1875-595X.1999.tb00533.x. PMID: 10907430.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The relationship between insomnia severity and depression, anxiety and anxiety sensitivity in general population
- Effects of pain catastrophizing and anxiety on analgesic use after surgical removal of impacted mandibular third molars
- Relationship between Serum Vitamin E Level and Serum High-Sensitivity C-Reactive Protein in Koreans: Based on National Health and Nutrition Survey
- Comparative Study for the Anesthetic Efficacy between Articaine HCl and Lidocaine HCl during the Surgical Extraction of Bilateral Mandibular Impacted Third Molars
- The anxiety in patients undergoing third molar extraction