J Korean Assoc Oral Maxillofac Surg.
2023 Oct;49(5):243-251. 10.5125/jkaoms.2023.49.5.243.
Association of the number of remaining teeth with kidney function in community-dwelling healthy older adults: a cross-sectional study
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Shimane University Faculty of Medicine, Izumo, Japan
- 2Center for Community-Based Healthcare Research and Education (CoHRE), Head Office for Research and Academic Information, Shimane University, Izumo, Japan
- 3Tominaga Dental Office, Ohchi, Japan
- KMID: 2547568
- DOI: http://doi.org/10.5125/jkaoms.2023.49.5.243
Abstract
Objectives
Although a few studies have investigated the relationship between kidney and oral function (number of remaining teeth), their results remain inconclusive. Therefore, this study aimed to investigate the relationship between kidney function and oral health in community-dwelling healthy elderlies and examine the factors associated with kidney function.
Materials and Methods
We used cross-sectional data from the Shimane prefecture cohort recruited by the Center for Community-Based Health Research and Education in 2019. We collected clinical data on dental status, background factors and kidney function (estimated glomerular filtration rate [eGFR], mL/min/1.73 m2 and creatinine levels, mg/dL).
Results
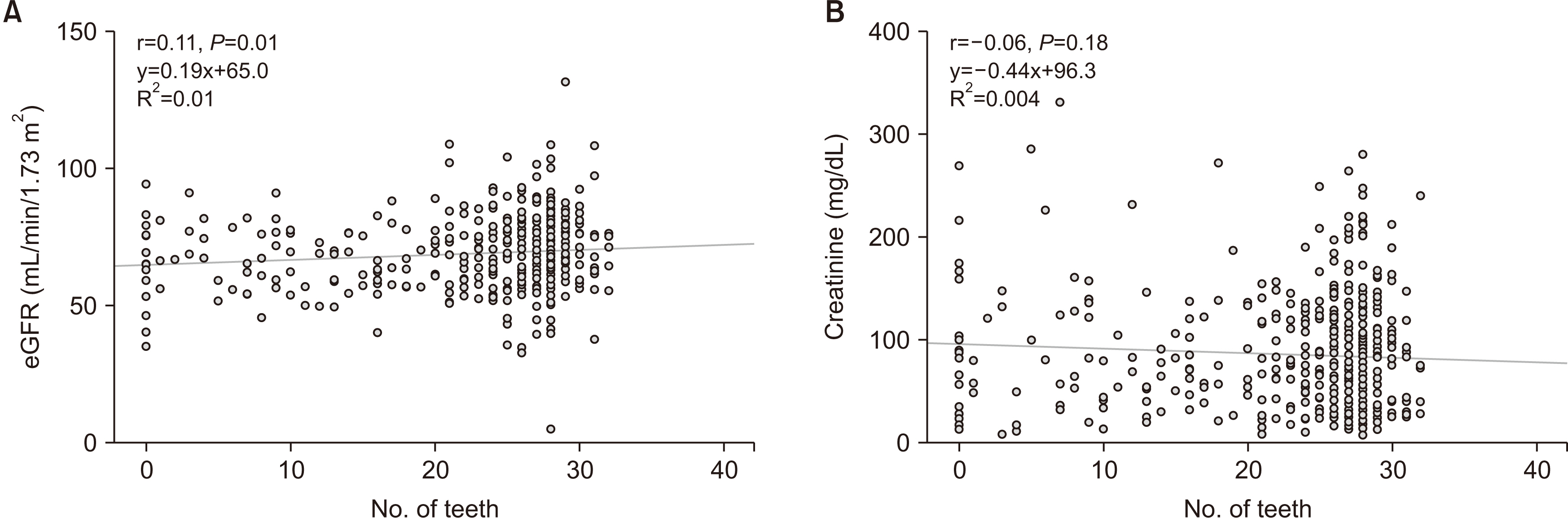
The study enrolled 481 participants, whose mean age was 66.7±7.4 years, and 223 (46.4%) participants were men. Multivariate analysis revealed significant correlations between eGFR (B=0.17, P=0.04), creatinine (B=–0.54, P<0.01), and the number of remaining teeth. The number of remaining teeth was associated with creatinine and eGFR, which are indicators of kidney function.
Conclusion
This study suggests that preserving the teeth may prevent decline in kidney function. Dental professionals should provide instructions and professional care to reduce the risk of systemic diseases such as kidney dysfunction.
Figure
Reference
-
References
1. Schena FP. 2011; Management of patients with chronic kidney disease. Intern Emerg Med. 6 Suppl 1:77–83. https://doi.org/10.1007/s11739-011-0688-2. DOI: 10.1007/s11739-011-0688-2. PMID: 22009616.
Article2. Ballew SH, Matsushita K. 2018; Cardiovascular risk prediction in CKD. Semin Nephrol. 38:208–16. https://doi.org/10.1016/j.semnephrol.2018.02.002. DOI: 10.1016/j.semnephrol.2018.02.002. PMID: 29753398.
Article3. Sedaghat S, Sorond F, Yaffe K, Sidney S, Kramer HJ, Jacobs DR Jr, et al. 2020; Decline in kidney function over the course of adulthood and cognitive function in midlife. Neurology. 95:e2389–97. https://doi.org/10.1212/wnl.0000000000010631. DOI: 10.1212/WNL.0000000000010631. PMID: 32878993. PMCID: PMC7682918.
Article4. Webster AC, Nagler EV, Morton RL, Masson P. 2017; Chronic kidney disease. Lancet. 389:1238–52. https://doi.org/10.1016/s0140-6736(16)32064-5. DOI: 10.1016/S0140-6736(16)32064-5. PMID: 27887750.
Article5. Wołyniec W, Ratkowski W, Kasprowicz K, Małgorzewicz S, Aleksandrowicz E, Zdrojewski T, et al. 2020; Factors influencing post-exercise proteinuria after marathon and ultramarathon races. Biol Sport. 37:33–40. https://doi.org/10.5114/biolsport.2020.89939. DOI: 10.5114/biolsport.2020.89939. PMID: 32205908. PMCID: PMC7075229.
Article6. Sabatino A, Cuppari L, Stenvinkel P, Lindholm B, Avesani CM. 2021; Sarcopenia in chronic kidney disease: what have we learned so far? J Nephrol. 34:1347–72. https://doi.org/10.1007/s40620-020-00840-y. DOI: 10.1007/s40620-020-00840-y. PMID: 32876940. PMCID: PMC8357704.
Article7. Yu MD, Zhang HZ, Zhang Y, Yang SP, Lin M, Zhang YM, et al. 2021; Relationship between chronic kidney disease and sarcopenia. Sci Rep. 11:20523. https://doi.org/10.1038/s41598-021-99592-3. DOI: 10.1038/s41598-021-99592-3. PMID: 34654871. PMCID: PMC8520007.
Article8. Ishikawa S, Naito S, Iimori S, Takahashi D, Zeniya M, Sato H, et al. 2018; Loop diuretics are associated with greater risk of sarcopenia in patients with non-dialysis-dependent chronic kidney disease. PLoS One. 13:e0192990. https://doi.org/10.1371/journal.pone.0192990. DOI: 10.1371/journal.pone.0192990. PMID: 29447254. PMCID: PMC5814019.
Article9. Hanna RM, Ghobry L, Wassef O, Rhee CM, Kalantar-Zadeh K. 2020; A practical approach to nutrition, protein-energy wasting, sarcopenia, and cachexia in patients with chronic kidney disease. Blood Purif. 49:202–11. https://doi.org/10.1159/000504240. DOI: 10.1159/000504240. PMID: 31851983.
Article10. Roshanravan B, Khatri M, Robinson-Cohen C, Levin G, Patel KV, de Boer IH, et al. 2012; A prospective study of frailty in nephrology-referred patients with CKD. Am J Kidney Dis. 60:912–21. https://doi.org/10.1053/j.ajkd.2012.05.017. DOI: 10.1053/j.ajkd.2012.05.017. PMID: 22770927. PMCID: PMC3491110.
Article11. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. 2001; ; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 56:M146–56. https://doi.org/10.1093/gerona/56.3.m146. DOI: 10.1093/gerona/56.3.M146. PMID: 11253156.
Article12. Tanaka T, Takahashi K, Hirano H, Kikutani T, Watanabe Y, Ohara Y, et al. 2018; Oral frailty as a risk factor for physical frailty and mortality in community-dwelling elderly. J Gerontol A Biol Sci Med Sci. 73:1661–7. https://doi.org/10.1093/gerona/glx225. DOI: 10.1093/gerona/glx225. PMID: 29161342.
Article13. Minakuchi S. 2022; Philosophy of oral hypofunction. Gerodontology. 39:1–2. https://doi.org/10.1111/ger.12606. DOI: 10.1111/ger.12606. PMID: 34779036.
Article14. Minakuchi S, Tsuga K, Ikebe K, Ueda T, Tamura F, Nagao K, et al. 2018; Oral hypofunction in the older population: position paper of the Japanese Society of Gerodontology in 2016. Gerodontology. 35:317–24. https://doi.org/10.1111/ger.12347. DOI: 10.1111/ger.12347. PMID: 29882364.
Article15. Ikebuchi K, Matsuda Y, Takeda M, Takeda M, Abe T, Tominaga K, et al. 2021; Relationship between masticatory function and bone mineral density in community-dwelling elderly: a cross-sectional study. Healthcare (Basel). 9:845. https://doi.org/10.3390/healthcare9070845. DOI: 10.3390/healthcare9070845. PMID: 34356223. PMCID: PMC8305999.
Article16. Sharma P, Fenton A, Dias IHK, Heaton B, Brown CLR, Sidhu A, et al. 2021; Oxidative stress links periodontal inflammation and renal function. J Clin Periodontol. 48:357–67. https://doi.org/10.1111/jcpe.13414. DOI: 10.1111/jcpe.13414. PMID: 33368493. PMCID: PMC7986430.
Article17. Choi HM, Han K, Park YG, Park JB. 2016; Associations between the number of natural teeth and renal dysfunction. Medicine (Baltimore). 95:e4681. https://doi.org/10.1097/md.0000000000004681. DOI: 10.1097/MD.0000000000004681. PMID: 27559974. PMCID: PMC5400341.
Article18. Kosaka S, Ohara Y, Naito S, Iimori S, Kado H, Hatta T, et al. 2020; Association among kidney function, frailty, and oral function in patients with chronic kidney disease: a cross-sectional study. BMC Nephrol. 21:357. https://doi.org/10.1186/s12882-020-02019-w. DOI: 10.1186/s12882-020-02019-w. PMID: 32819288. PMCID: PMC7441609.
Article19. Humphreys BD. 2018; Mechanisms of renal fibrosis. Annu Rev Physiol. 80:309–26. https://doi.org/10.1146/annurev-physiol-022516-034227. DOI: 10.1146/annurev-physiol-022516-034227. PMID: 29068765.
Article20. Chambrone L, Foz AM, Guglielmetti MR, Pannuti CM, Artese HP, Feres M, et al. 2013; Periodontitis and chronic kidney disease: a systematic review of the association of diseases and the effect of periodontal treatment on estimated glomerular filtration rate. J Clin Periodontol. 40:443–56. https://doi.org/10.1111/jcpe.12067. DOI: 10.1111/jcpe.12067. PMID: 23432795.
Article21. Serni L, Caroti L, Barbato L, Nieri M, Serni S, Cirami CL, et al. 2023; Association between chronic kidney disease and periodontitis. A systematic review and metanalysis. Oral Dis. 29:40–50. https://doi.org/10.1111/odi.14062. DOI: 10.1111/odi.14062. PMID: 34726333.
Article22. Kurt-Bayrakdar S, Kose O, Altin A, Akyildiz K, Mercantepe T, Bostan SA, et al. 2021; Periodontitis exacerbates the renal degenerative effects of obesity in rats. J Periodontal Res. 56:1058–69. https://doi.org/10.1111/jre.12919. DOI: 10.1111/jre.12919. PMID: 34328646.
Article23. Yoshihara A, Deguchi T, Hanada N, Miyazaki H. 2007; Renal function and periodontal disease in elderly Japanese. J Periodontol. 78:1241–8. https://doi.org/10.1902/jop.2007.070025. DOI: 10.1902/jop.2007.070025. PMID: 17608579.
Article24. Yoshihara A, Iwasaki M, Miyazaki H, Nakamura K. 2014; Association between low renal function and tooth loss over 5 years. Gerodontology. 31:111–6. https://doi.org/10.1111/ger.12015. DOI: 10.1111/ger.12015. PMID: 23176113.
Article25. Miyata Y, Obata Y, Mochizuki Y, Kitamura M, Mitsunari K, Matsuo T, et al. 2019; Periodontal disease in patients receiving dialysis. Int J Mol Sci. 20:3805. https://doi.org/10.3390/ijms20153805. DOI: 10.3390/ijms20153805. PMID: 31382656. PMCID: PMC6695931.
Article26. Pham TAV, Le DD. 2019; Dental condition and salivary characteristics in Vietnamese patients with chronic kidney disease. Int J Dent Hyg. 17:253–60. https://doi.org/10.1111/idh.12380. DOI: 10.1111/idh.12380. PMID: 30582881.
Article27. Lăzureanu PC, Popescu F, Tudor A, Stef L, Negru AG, Mihăilă R. 2021; Saliva pH and flow rate in patients with periodontal disease and associated cardiovascular disease. Med Sci Monit. 27:e931362. https://doi.org/10.12659/msm.931362. DOI: 10.12659/MSM.931362. PMID: 34305133. PMCID: PMC8323473.
Article28. Bassoukou IH, Nicolau J, dos Santos MT. 2009; Saliva flow rate, buffer capacity, and pH of autistic individuals. Clin Oral Investig. 13:23–7. https://doi.org/10.1007/s00784-008-0209-5. DOI: 10.1007/s00784-008-0209-5. PMID: 18594879.
Article29. Marinoski J, Bokor-Bratic M, Mitic I, Cankovic M. 2019; Oral mucosa and salivary findings in non-diabetic patients with chronic kidney disease. Arch Oral Biol. 102:205–11. https://doi.org/10.1016/j.archoralbio.2019.04.021. DOI: 10.1016/j.archoralbio.2019.04.021. PMID: 31078070.
Article30. Sugiura T, Takase H, Ohte N, Dohi Y. 2018; Dietary salt intake is a significant determinant of impaired kidney function in the general population. Kidney Blood Press Res. 43:1245–54. https://doi.org/10.1159/000492406. DOI: 10.1159/000492406. PMID: 30078009.
Article31. Nomura Y, Ishii Y, Suzuki S, Morita K, Suzuki A, Suzuki S, et al. 2020; Nutritional status and oral frailty: a community based study. Nutrients. 12:2886. https://doi.org/10.3390/nu12092886. DOI: 10.3390/nu12092886. PMID: 32967313. PMCID: PMC7551233.
Article32. Malta D, Petersen KS, Johnson C, Trieu K, Rae S, Jefferson K, et al. 2018; High sodium intake increases blood pressure and risk of kidney disease. From the science of salt: a regularly updated systematic review of salt and health outcomes (August 2016 to March 2017). J Clin Hypertens (Greenwich). 20:1654–65. https://doi.org/10.1111/jch.13408. DOI: 10.1111/jch.13408. PMID: 30402970. PMCID: PMC8030856.
Article33. Genco RJ, Graziani F, Hasturk H. 2020; Effects of periodontal disease on glycemic control, complications, and incidence of diabetes mellitus. Periodontol 2000. 83:59–65. https://doi.org/10.1111/prd.12271. DOI: 10.1111/prd.12271. PMID: 32385875.
Article34. Samsu N. 2021; Diabetic nephropathy: challenges in pathogenesis, diagnosis, and treatment. Biomed Res Int. 2021:1497449. https://doi.org/10.1155/2021/1497449. DOI: 10.1155/2021/1497449. PMID: 34307650. PMCID: PMC8285185.
Article35. Watanabe Y, Hirano H, Arai H, Morishita S, Ohara Y, Edahiro A, et al. 2017; Relationship between frailty and oral function in community-dwelling elderly adults. J Am Geriatr Soc. 65:66–76. https://doi.org/10.1111/jgs.14355. DOI: 10.1111/jgs.14355. PMID: 27655106.
Article36. Lertpimonchai A, Rattanasiri S, Arj-Ong Vallibhakara S, Attia J, Thakkinstian A. 2017; The association between oral hygiene and periodontitis: a systematic review and meta-analysis. Int Dent J. 67:332–43. https://doi.org/10.1111/idj.12317. DOI: 10.1111/idj.12317. PMID: 28646499. PMCID: PMC5724709.
Article37. Artese HP, de Sousa CO, Torres MC, Silva-Boghossian CM, Colombo AP. 2012; Effect of non-surgical periodontal treatment on the subgingival microbiota of patients with chronic kidney disease. Braz Oral Res. 26:366–72. https://doi.org/10.1590/s1806-83242012005000008. DOI: 10.1590/S1806-83242012005000008. PMID: 22714926.
Article38. Chen LP, Chiang CK, Peng YS, Hsu SP, Lin CY, Lai CF, et al. 2011; Relationship between periodontal disease and mortality in patients treated with maintenance hemodialysis. Am J Kidney Dis. 57:276–82. https://doi.org/10.1053/j.ajkd.2010.09.016. DOI: 10.1053/j.ajkd.2010.09.016. PMID: 21177012.
Article39. Yoshioka M, Shirayama Y, Imoto I, Hinode D, Yanagisawa S, Takeuchi Y. 2015; Current status of collaborative relationships between dialysis facilities and dental facilities in Japan: results of a nationwide survey. BMC Nephrol. 16:17. https://doi.org/10.1186/s12882-015-0001-0. DOI: 10.1186/s12882-015-0001-0. PMID: 25880326. PMCID: PMC4358784.
Article40. Betzler BK, Sultana R, Banu R, Tham YC, Lim CC, Wang YX, et al. 2021; Association between body mass index and chronic kidney disease in Asian populations: a participant-level meta-analysis. Maturitas. 154:46–54. https://doi.org/10.1016/j.maturitas.2021.09.005. DOI: 10.1016/j.maturitas.2021.09.005. PMID: 34736579.
Article41. Shepard BD. 2019; Sex differences in diabetes and kidney disease: mechanisms and consequences. Am J Physiol Renal Physiol. 317:F456–62. https://doi.org/10.1152/ajprenal.00249.2019. DOI: 10.1152/ajprenal.00249.2019. PMID: 31241989. PMCID: PMC6732459.
Article42. Duarte MP, Ribeiro HS, Neri SGR, Almeida LS, Oliveira JS, Viana JL, et al. 2023; Prevalence of low bone mineral density (T-score ≤ −2.5) in the whole spectrum of chronic kidney disease: a systematic review and meta-analysis. Osteoporos Int. 34:467–77. https://doi.org/10.1007/s00198-022-06598-2. DOI: 10.1007/s00198-022-06598-2. PMID: 36370217.
Article43. Ribeiro HS, Neri SGR, Oliveira JS, Bennett PN, Viana JL, Lima RM. 2022; Association between sarcopenia and clinical outcomes in chronic kidney disease patients: a systematic review and meta-analysis. Clin Nutr. 41:1131–40. https://doi.org/10.1016/j.clnu.2022.03.025. DOI: 10.1016/j.clnu.2022.03.025. PMID: 35430544.
Article44. Dhawan D, Sharma S. 2020; Abdominal obesity, adipokines and non-communicable diseases. J Steroid Biochem Mol Biol. 203:105737. https://doi.org/10.1016/j.jsbmb.2020.105737. DOI: 10.1016/j.jsbmb.2020.105737. PMID: 32818561. PMCID: PMC7431389.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Linear Association between Frailty as Assessed by the Kihon Checklist and Quality of Life in Community-Dwelling Older Adults: A Cross-Sectional Population-Based Study
- Influence of Advance Directives' Self-efficacy of Community-dwelling Older Adults on the Completion of Advance Directives: Mediating the Effect of Intention for Advance Directives: A Cross-Sectional Study
- Examination of Factors Associated with Self-Reported Cane Use among Community-Dwelling Older Adults
- Comparison of Comprehensive Health Status and Health-related Quality of Life between Institutionalized Older Adults and Community Dwelling Older Adults
- Influence of Cognitive Function and Depressive Symptoms on Instrumental Activities of Daily Living in Community-dwelling Older Adults