Ann Surg Treat Res.
2023 Nov;105(5):319-332. 10.4174/astr.2023.105.5.319.
Short-term and long-term clinical outcomes of combined major vessel resection for hilar cholangiocarcinoma: a propensity score analysis
- Affiliations
-
- 1Division of Biliary Tract Surgery, Department of General Surgery, West China Hospital, Sichuan University, Chengdu, China
- 2Research Center for Biliary Diseases, West China Hospital, Sichuan University, Chengdu, China
- KMID: 2547537
- DOI: http://doi.org/10.4174/astr.2023.105.5.319
Abstract
- Purpose
In the treatment of hilar cholangiocarcinoma (HCCA), combined resection of important hepatic vessels remains controversial. The purpose of this study was to compare the postoperative complications and prognosis of combined and non-combined major vessel resections in patients undergoing radical resection for HCCA.
Methods
In this study, patients with HCCA who underwent curative resection between January 2007 and December 2018 were retrospectively enrolled. Postoperative complications and prognosis between the groups were compared using propensity score-matching (PSM) analysis.
Results
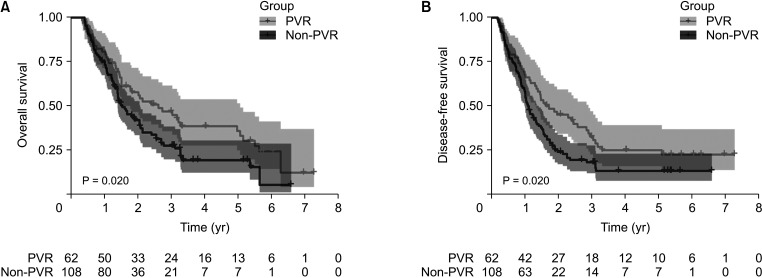
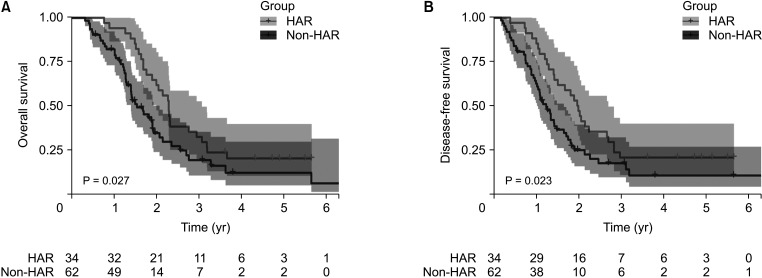
There were 310 patients included in this study. The portal vein resection (PVR) and hepatic artery resection (HAR) groups had a higher incidence of postoperative complications than the control group. Patients in the HAR group had an increased risk of abdominal and pleural effusion after surgery. Patients who underwent combined PVR had better overall survival (OS; P = 0.020) and disease-free survival (DFS; P = 0.020). After curative-intent resection, patients in the HAR group had improved OS (P = 0.027) and DFS (P = 0.023). The postoperative complications of combined vascular resection (VR) did not worsen long-term survival for patients.
Conclusion
In patients with HCCA, combined VR improved prognosis. The postoperative complications of combined VR do not worsen patient survival. Therefore, radical surgical resection is recommended.
Keyword
Figure
Reference
-
1. Zhou Q, Dong G, Zhu Q, Qiu Y, Mao L, Chen J, et al. Modification and comparison of CT criteria in the preoperative assessment of hepatic arterial invasion by hilar cholangiocarcinoma. Abdom Radiol (NY). 2021; 46:1922–1930. PMID: 33159559.
Article2. Soares KC, Kamel I, Cosgrove DP, Herman JM, Pawlik TM. Hilar cholangiocarcinoma: diagnosis, treatment options, and management. Hepatobiliary Surg Nutr. 2014; 3:18–34. PMID: 24696835.3. Serrablo A, Serrablo L, Alikhanov R, Tejedor L. Vascular resection in perihilar cholangiocarcinoma. Cancers (Basel). 2021; 13:5278. PMID: 34771439.
Article4. Capobianco I, Rolinger J, Nadalin S. Resection for Klatskin tumors: technical complexities and results. Transl Gastroenterol Hepatol. 2018; 3:69. PMID: 30363698.
Article5. Schimizzi GV, Jin LX, Davidson JT 4th, Krasnick BA, Ethun CG, Pawlik TM, et al. Outcomes after vascular resection during curative-intent resection for hilar cholangiocarcinoma: a multi-institution study from the US extrahepatic biliary malignancy consortium. HPB (Oxford). 2018; 20:332–339. PMID: 29169904.
Article6. Mizuno T, Ebata T, Yokoyama Y, Igami T, Yamaguchi J, Onoe S, et al. Combined vascular resection for locally advanced perihilar cholangiocarcinoma. Ann Surg. 2022; 275:382–390. PMID: 32976284.
Article7. de Jong MC, Marques H, Clary BM, Bauer TW, Marsh JW, Ribero D, et al. The impact of portal vein resection on outcomes for hilar cholangiocarcinoma: a multiinstitutional analysis of 305 cases. Cancer. 2012; 118:4737–4747. PMID: 22415526.
Article8. Wen N, Liu F, Zhang H, Lu J, Li B, Cheng N. Laparoscopic liver resection for hepatocellular carcinoma presents less respiratory complications compared with open procedure: a propensity score analysis in the elderly. Eur J Surg Oncol. 2021; 47:2675–2681. PMID: 34059378.
Article9. Vogel A, Bridgewater J, Edeline J, Kelley RK, Klümpen HJ, Malka D, et al. Electronic address: clinicalguidelines@esmo.org. Biliary tract cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. 2023; 34:127–140. PMID: 36372281.
Article10. Bismuth H, Nakache R, Diamond T. Management strategies in resection for hilar cholangiocarcinoma. Ann Surg. 1992; 215:31–38. PMID: 1309988.
Article11. Miyazaki M, Ohtsuka M, Miyakawa S, Nagino M, Yamamoto M, Kokudo N, et al. Classification of biliary tract cancers established by the Japanese Society of Hepato-Biliary-Pancreatic Surgery: 3(rd) English edition. J Hepatobiliary Pancreat Sci. 2015; 22:181–196. PMID: 25691463.
Article12. Song Y, Zhang Y, Zhen Z, Huang Z. Effects of portal vein resection and hepatic artery resection on long-term survival in Klatskin tumor: a meta-analysis. World J Surg Oncol. 2022; 20:230. PMID: 35821140.
Article13. Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg. 1999; 230:808–819. PMID: 10615936.
Article14. Lee SG, Song GW, Hwang S, Ha TY, Moon DB, Jung DH, et al. Surgical treatment of hilar cholangiocarcinoma in the new era: the Asan experience. J Hepatobiliary Pancreat Sci. 2010; 17:476–489. PMID: 19851704.
Article15. Noji T, Hirano S, Tanaka K, Matsui A, Nakanishi Y, Asano T, et al. Concomitant hepatic artery resection for advanced perihilar cholangiocarcinoma: a narrative review. Cancers (Basel). 2022; 14:2672. PMID: 35681652.
Article16. Noji T, Tsuchikawa T, Okamura K, Tanaka K, Nakanishi Y, Asano T, et al. Concomitant hepatic artery resection for advanced perihilar cholangiocarcinoma: a case-control study with propensity score matching. J Hepatobiliary Pancreat Sci. 2016; 23:442–448. PMID: 27207604.
Article17. Chun YS, Pawlik TM, Vauthey JN. 8th edition of the AJCC cancer staging manual: pancreas and hepatobiliary cancers. Ann Surg Oncol. 2018; 25:845–847. PMID: 28752469.
Article18. Wu Y, Mao A, Wang H, Fang G, Zhou J, He X, et al. Association of simultaneous vs delayed resection of liver metastasis with complications and survival among adults with colorectal cancer. JAMA Netw Open. 2022; 5:e2231956. PMID: 36121654.
Article19. Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, et al. The “50-50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg. 2005; 242:824–829. PMID: 16327492.20. Harimoto N, Araki K, Ishii N, Muranushi R, Hoshino K, Hagiwara K, et al. Predictors of postoperative ascites after hepatic resection in patients with hepatocellular carcinoma. Anticancer Res. 2020; 40:4343–4349. PMID: 32727762.
Article21. Rahbari NN, Garden OJ, Padbury R, Maddern G, Koch M, Hugh TJ, et al. Post-hepatectomy haemorrhage: a definition and grading by the International Study Group of Liver Surgery (ISGLS). HPB (Oxford). 2011; 13:528–535. PMID: 21762295.
Article22. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.23. Miyazaki M, Kato A, Ito H, Kimura F, Shimizu H, Ohtsuka M, et al. Combined vascular resection in operative resection for hilar cholangiocarcinoma: does it work or not? Surgery. 2007; 141:581–588. PMID: 17462457.
Article24. Higuchi R, Yazawa T, Uemura S, Izumo W, Ota T, Kiyohara K, et al. Surgical outcomes for perihilar cholangiocarcinoma with vascular invasion. J Gastrointest Surg. 2019; 23:1443–1453. PMID: 30203230.
Article25. Matsuyama R, Mori R, Ota Y, Homma Y, Kumamoto T, Takeda K, et al. Significance of vascular resection and reconstruction in surgery for hilar cholangiocarcinoma: with special reference to hepatic arterial resection and reconstruction. Ann Surg Oncol. 2016; 23(Suppl 4):475–484. PMID: 27387681.
Article26. Kawakatsu S, Ebata T, Watanabe N, Onoe S, Yamaguchi J, Mizuno T, et al. Mild prognostic impact of postoperative complications on long-term survival of perihilar cholangiocarcinoma. Ann Surg. 2022; 276:146–152. PMID: 32889874.
Article27. Saeki H, Tsutsumi S, Tajiri H, Yukaya T, Tsutsumi R, Nishimura S, et al. Prognostic significance of postoperative complications after curative resection for patients with esophageal squamous cell carcinoma. Ann Surg. 2017; 265:527–533. PMID: 28169928.
Article28. Tokunaga M, Tanizawa Y, Bando E, Kawamura T, Terashima M. Poor survival rate in patients with postoperative intra-abdominal infectious complications following curative gastrectomy for gastric cancer. Ann Surg Oncol. 2013; 20:1575–1583. PMID: 23076557.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preoperative Diagnosis and Management for Hilar Cholangiocarcinoma
- Robotic major liver resections: Surgical outcomes compared with open major liver resections
- Analysis of Long-Term Survivors after Resection for Hilar Bile Duct Cancer
- Prognostic factors in the Surgical Treatment of Hilar Cholangiocarcinoma
- Chronological analysis of surgical and oncological outcomes after the treatment of perihilar cholangiocarcinoma