Ann Surg Treat Res.
2023 Nov;105(5):281-289. 10.4174/astr.2023.105.5.281.
Real-world survival after colorectal surgery for malignancy in Korean patients with chronic kidney disease: an analysis of Korean healthcare big data, 2002–2019
- Affiliations
-
- 1Division of Colorectal Surgery, Department of Surgery, Dongnam Institute of Radiological and Medical Sciences. Busan, Korea
- 2RexSoft Corporation, Seoul, Korea
- 3Institute of Health and Environment, Seoul National University, Seoul, Korea
- 4Department of Surgery, Chung-Ang University College of Medicine, Seoul, Korea
- 5Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2547533
- DOI: http://doi.org/10.4174/astr.2023.105.5.281
Abstract
- Purpose
Globally, chronic kidney disease (CKD) is common and has been associated with an increased risk of colorectal cancer (CRC). There is a dearth of literature on the real-world morbidity and mortality associated with CKD comorbid with CRC. This study was performed to evaluate real-world survival outcomes of colorectal malignancy in Korean CKD patients.
Methods
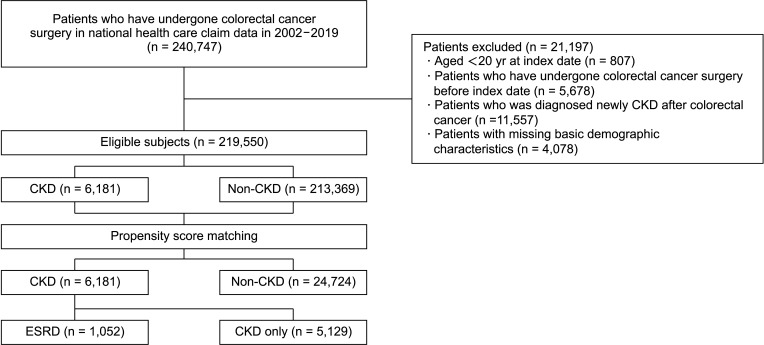
The National Health Insurance Service of Korea provided data on patients who underwent surgical resection among patients diagnosed with CRC from 2002 to 2019.
Results
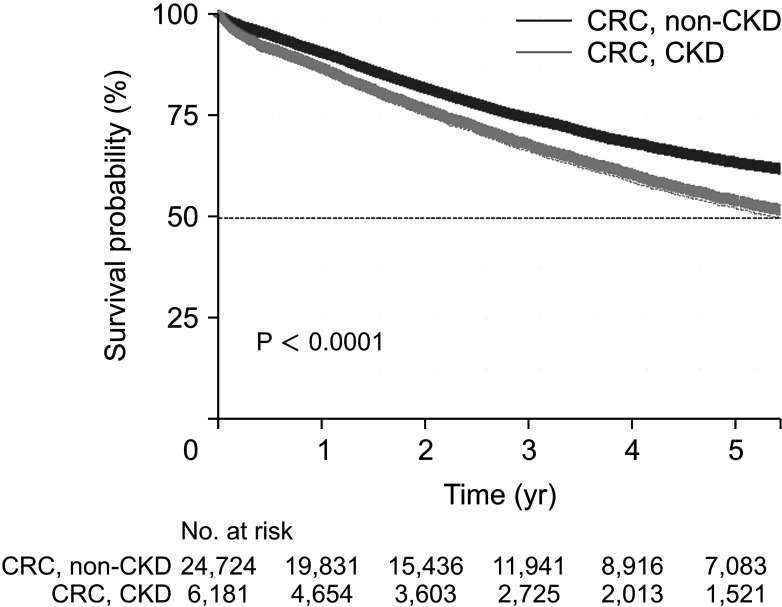
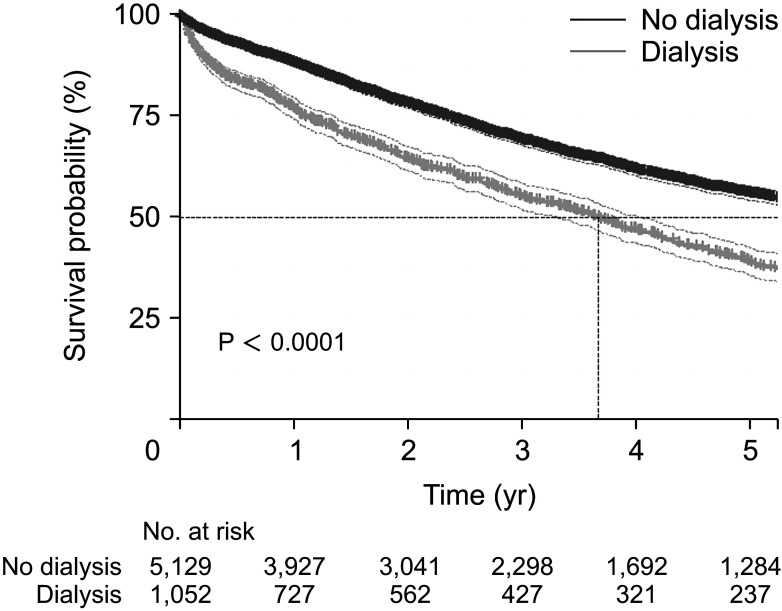
A total of 219,550 patients were included: 6,181 patients with underlying CKD and 213,369 patients without it. Each morbidity was significantly higher in the CKD-CRC group, and the postoperative mortality rates for the 30-day (3.11% vs. 1.78%, P < 0.001), 60-day (5.95% vs. 3.83%, P < 0.001), and 90-day mortality rate (8.12% vs. 5.32%, P < 0.001) were significantly higher in the CKD group. The median survival time (MST, year) was significantly lower in the CKD-CRC group (5.63; interquartile range [IQR], 5.26–5.91) than in the non-CKD-CRC group (8.71; IQR, 8.37–8.93). MST was significantly lower among CKD patients who received chemotherapy after adjustment by multivariate analysis (adjusted hazard ratio [HR], 1.43; 95% confidence interval [CI], 1.37–1.49; P < 0.001]). Subgroup analysis showed that in the CKD-CRC group, MST was lower in patients who received dialysis than in those who did not, even after multivariate analysis (adjusted HR, 2.38; 95% CI, 2.20–2.58; P < 0.001).
Conclusion
Prevention of CKD-to-end-stage renal disease progression should be adopted as a strategy to increase postoperative survival, along with active surveillance and cancer treatment.
Figure
Reference
-
1. Park JI, Baek H, Jung HH. Prevalence of chronic kidney disease in Korea: the Korean National Health and Nutritional Examination Survey 2011-2013. J Korean Med Sci. 2016; 31:915–923. PMID: 27247501.
Article2. Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007; 298:2038–2047. PMID: 17986697.
Article3. Paik JH, Ryu CG, Hwang DY. Risk factors of recurrence in TNM stage I colorectal cancer. Ann Surg Treat Res. 2023; 104:281–287. PMID: 37179701.
Article4. Myung J, Choi JH, Yi JH, Kim I. Cancer incidence according to the National Health Information Database in Korean patients with end-stage renal disease receiving hemodialysis. Korean J Intern Med. 2020; 35:1210–1219. PMID: 32066223.
Article5. Shebl FM, Warren JL, Eggers PW, Engels EA. Cancer risk among elderly persons with end-stage renal disease: a population-based case-control study. BMC Nephrol. 2012; 13:65. PMID: 22834953.
Article6. Kitchlu A, Shapiro J, Amir E, Garg AX, Kim SJ, Wald R, et al. Representation of patients with chronic kidney disease in trials of cancer therapy. JAMA. 2018; 319:2437–2439. PMID: 29922818.
Article7. Shin N, Han EC, Won S, Ryoo SB, Choe EK, Park BK, et al. The prognoses and postoperative outcomes of patients with both colorectal cancer and liver cirrhosis based on a nationwide cohort in Korea. Ann Surg Treat Res. 2020; 99:82–89. PMID: 32802813.
Article8. Lee YH, Han K, Ko SH, Ko KS, Lee KU. Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Data analytic process of a nationwide population-based study using National Health Information Database established by National Health Insurance Service. Diabetes Metab J. 2016; 40:79–82. PMID: 26912157.
Article9. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43:1130–1139. PMID: 16224307.
Article10. Swartling O, Rydell H, Stendahl M, Segelmark M, Trolle Lagerros Y, Evans M. CKD progression and mortality among men and women: a nationwide study in Sweden. Am J Kidney Dis. 2021; 78:190–199. PMID: 33434591.
Article11. Sprangers B, Abudayyeh A, Latcha S, Perazella MA, Jhaveri KD. How to determine kidney function in cancer patients? Eur J Cancer. 2020; 132:141–149. PMID: 32361629.
Article12. Huang CS, Huang LK, Chen CY, Wang WS, Yang SH. Prognostic value of postoperative serum carcinoembryonic antigen levels in colorectal cancer patients with chronic kidney disease. Am J Surg. 2021; 221:162–167. PMID: 32746979.
Article13. Chen DP, Davis BR, Simpson LM, Cushman WC, Cutler JA, Dobre M, et al. Association between chronic kidney disease and cancer mortality: a report from the ALLHAT. Clin Nephrol. 2017; 87(2017):11–20. PMID: 27900942.
Article14. Pedrazzoli P, Silvestris N, Santoro A, Secondino S, Brunetti O, Longo V, et al. Management of patients with end-stage renal disease undergoing chemotherapy: recommendations of the Associazione Italiana di Oncologia Medica (AIOM) and the Società Italiana di Nefrologia (SIN). ESMO Open. 2017; 2:e000167. PMID: 29209521.
Article15. Nishiyama K, Aono K, Fujimoto Y, Kuwamura M, Okada T, Tokumoto H, et al. Chronic kidney disease after 5/6 nephrectomy disturbs the intestinal microbiota and alters intestinal motility. J Cell Physiol. 2019; 234:6667–6678. PMID: 30317589.
Article16. Glorieux G, Gryp T, Perna A. Gut-derived metabolites and their role in immune dysfunction in chronic kidney disease. Toxins (Basel). 2020; 12:245. PMID: 32290429.
Article17. Ozawa S, Tsujimoto M, Uchiyama H, Ito N, Morishita S, Yamamoto M, et al. Uremic serum residue decreases SN-38 sensitivity through suppression of organic anion transporter polypeptide 2B1 in LS-180 colon cancer cells. Sci Rep. 2019; 9:15464. PMID: 31664047.
Article18. Saus E, Iraola-Guzmán S, Willis JR, Brunet-Vega A, Gabaldón T. Microbiome and colorectal cancer: roles in carcinogenesis and clinical potential. Mol Aspects Med. 2019; 69:93–106. PMID: 31082399.
Article19. Song M, Chan AT, Sun J. Influence of the gut microbiome, diet, and environment on risk of colorectal cancer. Gastroenterology. 2020; 158:322–340. PMID: 31586566.
Article20. Robinson BM, Akizawa T, Jager KJ, Kerr PG, Saran R, Pisoni RL. Factors affecting outcomes in patients reaching end-stage kidney disease worldwide: differences in access to renal replacement therapy, modality use, and haemodialysis practices. Lancet. 2016; 388:294–306. PMID: 27226132.
Article21. Canedo J, Ricciardi K, DaSilva G, Rosen L, Weiss EG, Wexner SD. Are postoperative complications more common following colon and rectal surgery in patients with chronic kidney disease? Colorectal Dis. 2013; 15:85–90. PMID: 22632259.
Article22. Drolet S, Maclean AR, Myers RP, Shaheen AA, Dixon E, Donald Buie W. Morbidity and mortality following colorectal surgery in patients with end-stage renal failure: a population-based study. Dis Colon Rectum. 2010; 53:1508–1516. PMID: 20940599.
Article23. Sirany AM, Chow CJ, Kunitake H, Madoff RD, Rothenberger DA, Kwaan MR. Colorectal surgery outcomes in chronic dialysis patients: an American College of Surgeons National Surgical Quality Improvement Program study. Dis Colon Rectum. 2016; 59:662–669. PMID: 27270519.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Real World Data and Artificial Intelligence in Diabetology
- Pediatric Cancer Research using Healthcare Big Data
- Potentiality of Big Data in the Medical Sector: Focus on How to Reshape the Healthcare System
- Medicine in the Fourth Industrial Revolution: What Should We Prepare?
- Clinical Research from a Health Insurance Database: Practice and Perspective