J Korean Neurosurg Soc.
2023 Nov;66(6):611-617. 10.3340/jkns.2023.0146.
The Sagittal Balance of Cervical Spine : Comprehensive Review of Recent Update
- Affiliations
-
- 1Departments of Neurosurgery, Hallym University Sacred Heart Hospital, Anyang, Korea
- 2Departments of Orthopedics, Hallym University Sacred Heart Hospital, Anyang, Korea
- 3Spine Center, Hallym University Sacred Heart Hospital, Anyang, Korea
- KMID: 2547455
- DOI: http://doi.org/10.3340/jkns.2023.0146
Abstract
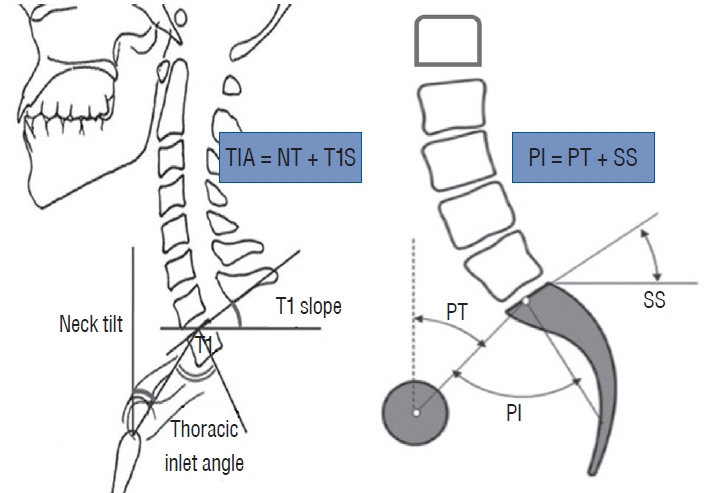
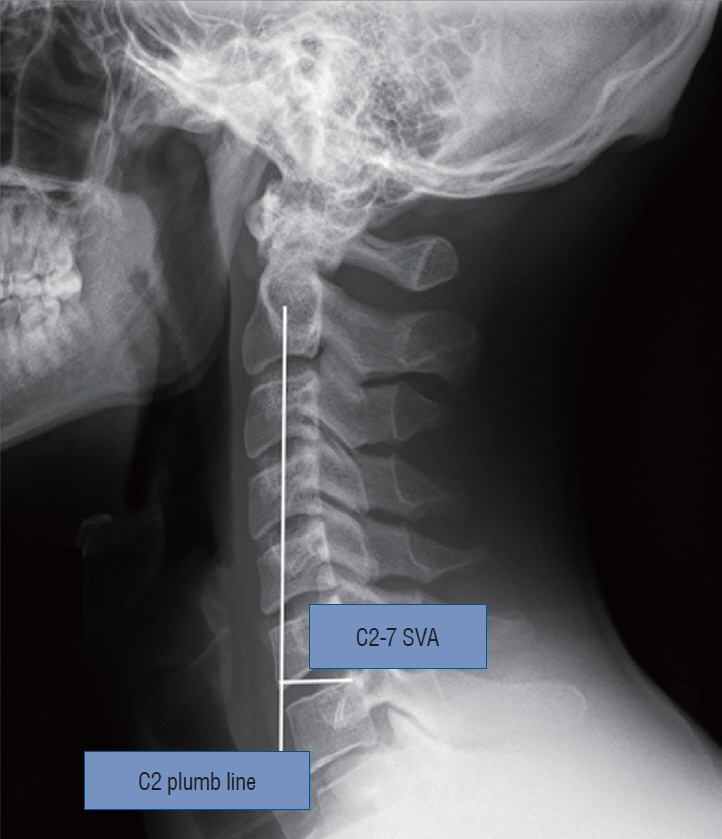
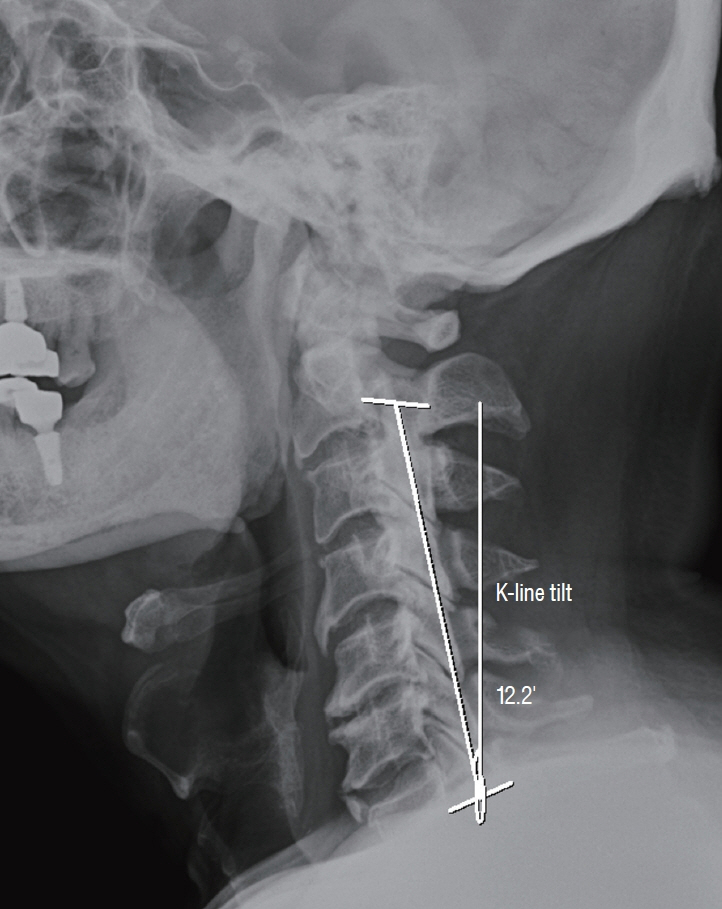
- The cervical spine plays a critical role in supporting the skull, maintaining horizontal gaze, and facilitating walking. Its unique characteristics, including the widest range of motion among spinal segments, have led to extensive research on cervical sagittal alignment. Various parameters have been proposed to evaluate cervical alignment, with studies investigating their clinical significance, correlation with symptoms, and implications for surgical interventions. Recent findings suggest that cervical sagittal alignment not only impacts the cervical spine but also influences global spine-pelvic alignment through compensatory mechanisms. This comprehensive review examines classical and new parameters of cervical sagittal alignment and considers the dynamic and muscular factors associated with it.
Keyword
Figure
Reference
-
References
1. Ames CP, Blondel B, Scheer JK, Schwab FJ, Le Huec JC, Massicotte EM, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976). 38(22 Suppl 1):S149–S160. 2013.2. Ames CP, Smith JS, Eastlack R, Blaskiewicz DJ, Shaffrey CI, Schwab F, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine. 23:673–683. 2015.
Article3. Ames CP, Smith JS, Scheer JK, Bess S, Bederman SS, Deviren V, et al. Impact of spinopelvic alignment on decision making in deformity surgery in adults: a review. J Neurosurg Spine. 16:547–564. 2012.
Article4. Buckland AJ, Vira S, Oren JH, Lafage R, Harris BY, Spiegel MA, et al. When is compensation for lumbar spinal stenosis a clinical sagittal plane deformity? Spine J. 16:971–981. 2016.
Article5. Chen J, Wang J, Wei X, Guan H, Wang B, Xu H, et al. The importance of preoperative t1 slope for determining proper postoperative c2-7 cobb’s angle in patients undergoing cervical reconstruction. J Orthop Surg Res. 15:507. 2020.
Article6. Fujiyoshi T, Yamazaki M, Kawabe J, Endo T, Furuya T, Koda M, et al. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spine (Phila Pa 1976). 33:E990–E993. 2008.7. Hardacker JW, Shuford RF, Capicotto PN, Pryor PW. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine (Phila Pa 1976). 22:1472–1480. discussion 1480. 1997.
Article8. Hey HWD, Teo AQA, Tan KA, Ng LWN, Lau LL, Liu KG, et al. How the spine differs in standing and in sitting-important considerations for correction of spinal deformity. Spine J. 17:799–806. 2017.
Article9. Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Clinical impact of t1 slope minus cervical lordosis after multilevel posterior cervical fusion surgery: a minimum 2-year follow up data. Spine (Phila Pa 1976). 42:1859–1864. 2017.
Article10. Iyer S, Lenke LG, Nemani VM, Fu M, Shifflett GD, Albert TJ, et al. Variations in occipitocervical and cervicothoracic alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine (Phila Pa 1976). 41:1837–1844. 2016.
Article11. Jun HS, Kim JH, Ahn JH, Chang IB, Song JH, Kim TH, et al. T1 slope and degenerative cervical spondylolisthesis. Spine (Phila Pa 1976). 40:E220–E226. 2015.
Article12. Kim CW, Hyun SJ, Kim KJ. Systematic review of reciprocal changes after spinal reconstruction surgery : do not miss the forest for the trees. J Korean Neurosurg Soc. 64:843–852. 2021.
Article13. Kim HJ, Virk S, Elysee J, Passias P, Ames C, Shaffrey CI, et al. The morphology of cervical deformities: a two-step cluster analysis to identify cervical deformity patterns. J Neurosurg Spine. 32:353–359. 2019.
Article14. Kim HS, Kim TH, Park MS, Kim SW, Chang HG, Kim JH, et al. K-line tilt as a novel radiographic parameter in cervical sagittal alignment. Eur Spine J. 27:2023–2028. 2018.
Article15. Kim N, Suk KS, Kwon JW, Seo J, Ju H, Lee BH, et al. Clinical significance of the c2 slope after multilevel cervical spine fusion. J Neurosurg Spine. 38:24–30. 2022.
Article16. Kim SW, Kim TH, Bok DH, Jang C, Yang MH, Lee S, et al. Analysis of cervical spine alignment in currently asymptomatic individuals: prevalence of kyphotic posture and its relationship with other spinopelvic parameters. Spine J. 18:797–810. 2018.
Article17. Koshimizu H, Sakai Y, Harada A, Ito S, Ito K, Hida T. The impact of sarcopenia on cervical spine sagittal alignment after cervical laminoplasty. Clin Spine Surg. 31:E342–E346. 2018.
Article18. Lan Z, Wu Z, Xu W, Huang Y. Analysis of a radiographic parameter Kline tilt following adjacent two-level anterior cervical discectomy and fusion: a retrospective study. J Orthop Surg Res. 15:131. 2020.
Article19. Lee JK, Hyun SJ, Yang SH, Kim KJ. Clinical impact and correlations of odontoid parameters following multilevel posterior cervical fusion surgery. Neurospine. 19:912–920. 2022.
Article20. Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech. 25:E41–E47. 2012.
Article21. Lee SH, Son DW, Lee JS, Sung SK, Lee SW, Song GS. Does extension dysfunction affect postoperative loss of cervical lordosis in patients who undergo laminoplasty? Spine (Phila Pa 1976). 44:E456–E464. 2019.
Article22. Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 7:99–103. 1998.
Article23. Mizutani J, Strom R, Abumi K, Endo K, Ishii K, Yagi M, et al. How cervical reconstruction surgery affects global spinal alignment. Neurosurgery. 84:898–907. 2019.
Article24. Nemani VM, Louie PK, Drolet CE, Rhee JM. Defining cervical sagittal plane deformity - when are sagittal realignment procedures necessary in patients presenting primarily with radiculopathy or myelopathy? Neurospine. 19:876–882. 2022.
Article25. Oe S, Togawa D, Nakai K, Yamada T, Arima H, Banno T, et al. The influence of age and sex on cervical spinal alignment among volunteers aged over 50. Spine (Phila Pa 1976). 40:1487–1494. 2015.
Article26. Passfall L, Williamson TK, Krol O, Lebovic J, Imbo B, Joujon-Roche R, et al. Do the newly proposed realignment targets for c2 and t1 slope bridge the gap between radiographic and clinical success in corrective surgery for adult cervical deformity? J Neurosurg Spine. 37:368–375. 2022.
Article27. Passias PG, Segreto FA, Bortz CA, Horn SR, Frangella NJ, Diebo BG, et al. Fatty infiltration of cervical spine extensor musculature: is there a relationship with cervical sagittal balance? Clin Spine Surg. 31:428–434. 2018.28. Passias PG, Segreto FA, Horn SR, Lafage V, Lafage R, Smith JS, et al. Fatty infiltration of the cervical extensor musculature, cervical sagittal balance, and clinical outcomes: an analysis of operative adult cervical deformity patients. J Clin Neurosci. 72:134–141. 2020.
Article29. Protopsaltis TS, Ramchandran S, Tishelman JC, Smith JS, Neuman BJ, Mundis GM Jr, et al. The importance of C2 slope, a singular marker of cervical deformity, correlates with patient-reported outcomes. Spine (Phila Pa 1976). 45:184–192. 2020.
Article30. Rao H, Chen Y, Xu W, Zhou Z. Clinical effects of preoperative k-line tilt on patient outcomes after laminoplasty for cervical ossification of the posterior longitudinal ligament. World Neurosurg. 150:e639–e644. 2021.
Article31. Sakai K, Yoshii T, Arai Y, Hirai T, Torigoe I, Inose H, et al. K-line tilt is a predictor of postoperative kyphotic deformity after laminoplasty for cervical myelopathy caused by ossification of the posterior longitudinal ligament. Global Spine J. 13:1005–1010. 2023.
Article32. Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976). 38:E803–E812. 2013.33. Smith JS, Lafage V, Ryan DJ, Shaffrey CI, Schwab FJ, Patel AA, et al. Association of myelopathy scores with cervical sagittal balance and normalized spinal cord volume: analysis of 56 preoperative cases from the aospine north america myelopathy study. Spine (Phila Pa 1976). 38(22 Suppl 1):S161–S170. 2013.34. Smith JS, Shaffrey CI, Lafage V, Blondel B, Schwab F, Hostin R, et al. Spontaneous improvement of cervical alignment after correction of global sagittal balance following pedicle subtraction osteotomy. J Neurosurg Spine. 17:300–307. 2012.
Article35. Song K, Su X, Zhang Y, Liu C, Tang X, Zhang G, et al. Optimal chin-brow vertical angle for sagittal visual fields in ankylosing spondylitis kyphosis. Eur Spine J. 25:2596–2604. 2016.
Article36. Sparrey CJ, Bailey JF, Safaee M, Clark AJ, Lafage V, Schwab F, et al. Etiology of lumbar lordosis and its pathophysiology: a review of the evolution of lumbar lordosis, and the mechanics and biology of lumbar degeneration. Neurosurg Focus. 36:E1. 2014.
Article37. Suk KS, Kim KT, Lee SH, Kim JM. Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine (Phila Pa 1976). 28:2001–2005. 2003.
Article38. Tang JA, Scheer JK, Smith JS, Deviren V, Bess S, Hart RA, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 71:662–669. discussion 669. 2012.
Article39. Wei B, Liu W, Wu H. Analysis between preoperative cervical radiographic parameters represented by the K-line tilt and the short-term prognosis of laminoplasty for posterior longitudinal ligament ossification: a retrospective study. Front Surg. 9:950707. 2022.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cervical Sagittal Alignment: Literature Review and Future Directions
- Sagittal Fracture of Cervical Spine: Case Report
- Surgical Impact on Global Sagittal Alignment and Health-Related Quality of Life Following Cervical Kyphosis Correction Surgery: Systematic Review
- Reciprocal Changes Following Cervical Realignment Surgery
- Spino-Pelvic Parameters in Adult Spinal Deformities