Brain Tumor Res Treat.
2023 Oct;11(4):266-270. 10.14791/btrt.2023.0025.
Recurrence of Rathke’s Cleft Cyst Following Surgery and Histopathological Considerations for Recurrence: A Case Presentation
- Affiliations
-
- 1Department of Neurosurgery, Anam Hospital, Korea University Medical Center, Korea University College of Medicine, Seoul, Korea
- KMID: 2547415
- DOI: http://doi.org/10.14791/btrt.2023.0025
Abstract
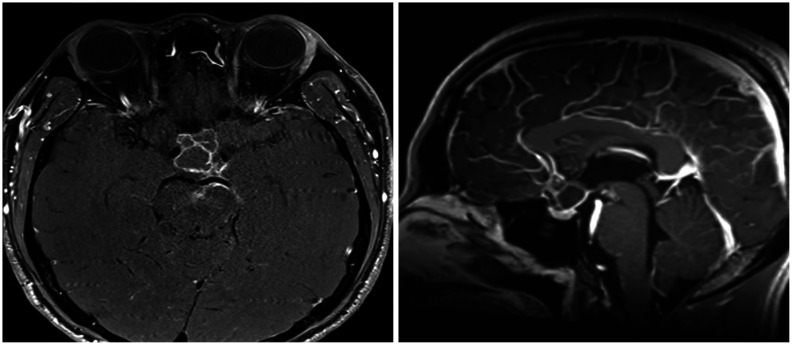
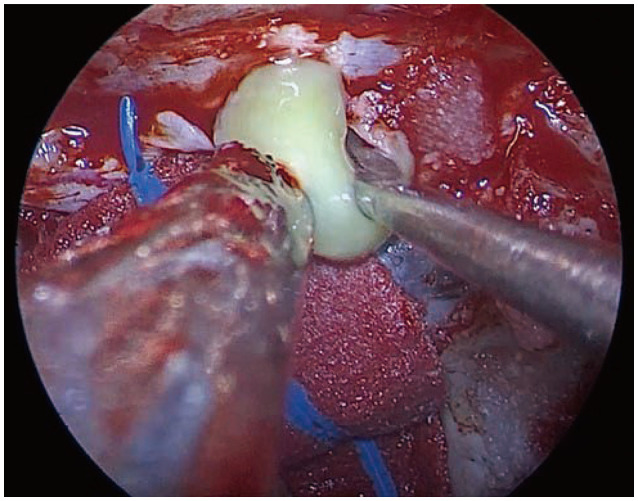
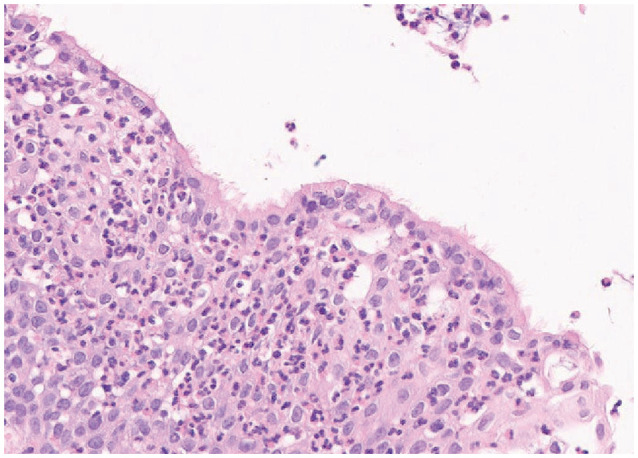
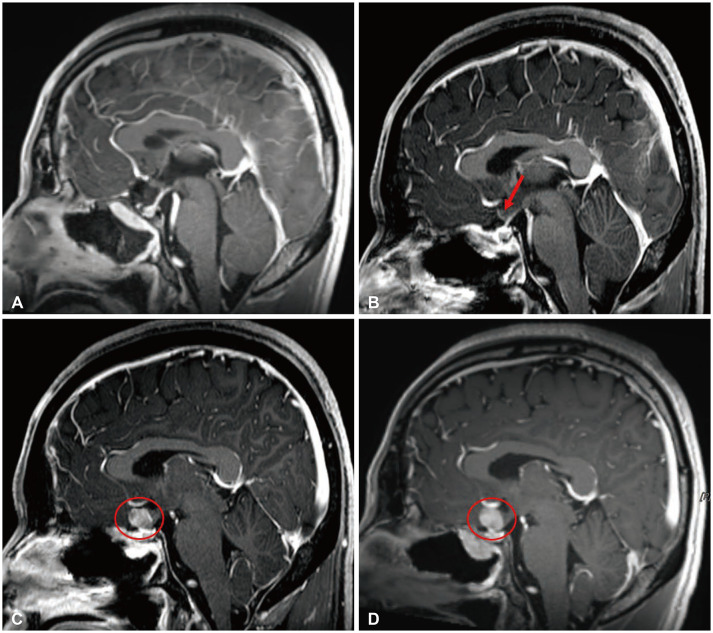
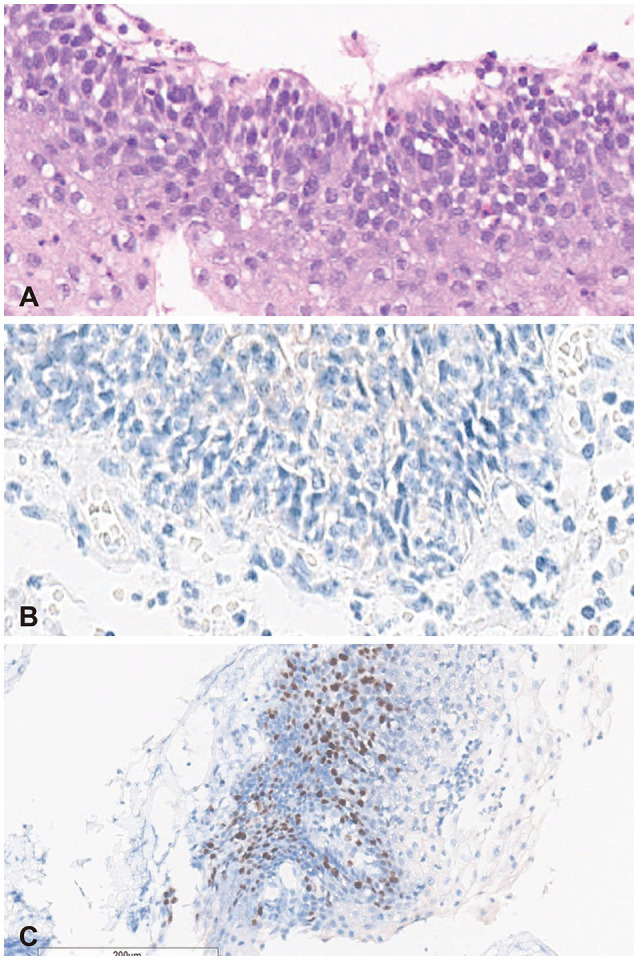
- Recurrence of Rathke’s cleft cysts (RCC) following surgery is not uncommon. We present a 33-yearold male patient with chronic headache and visual disturbances whose MRI showed mostly cystic, suprasellar mass with peripheral enhancement. Endoscopic extended transsphenoidal approach and tumor resection was performed and RCC was pathologically confirmed postoperatively. Early recurrence was first suspected at 3 months following surgery, and his serial MRIs showed a recurred mass without associated clinical symptoms. Upon further histopathological study, extensive squamous metaplasia and high Ki-67 were seen. Also, in this study, we discuss important factors associated with cyst recurrence following surgery.
Figure
Reference
-
1. Iannelli A, Martini C, Cosottini M, Castagna M, Bogazzi F, Muscatello L. Rathke’s cleft cysts in children: clinical, diagnostic, and surgical features. Childs Nerv Syst. 2012; 28:297–303. PMID: 22057478.
Article2. Han SJ, Rolston JD, Jahangiri A, Aghi MK. Rathke’s cleft cysts: review of natural history and surgical outcomes. J Neurooncol. 2014; 117:197–203. PMID: 24146189.
Article3. El-Mahdy W, Powell M. Transsphenoidal management of 28 symptomatic Rathke’s cleft cysts, with special reference to visual and hormonal recovery. Neurosurgery. 1998; 42:7–17. PMID: 9442498.
Article4. Raper DM, Besser M. Clinical features, management and recurrence of symptomatic Rathke’s cleft cyst. J Clin Neurosci. 2009; 16:385–389. PMID: 19147363.
Article5. Aho CJ, Liu C, Zelman V, Couldwell WT, Weiss MH. Surgical outcomes in 118 patients with Rathke cleft cysts. J Neurosurg. 2005; 102:189–193.
Article6. Benveniste RJ, King WA, Walsh J, Lee JS, Naidich TP, Post KD. Surgery for Rathke cleft cysts: technical considerations and outcomes. J Neurosurg. 2004; 101:577–584. PMID: 15481709.
Article7. Kim JE, Kim JH, Kim OL, Paek SH, Kim DG, Chi JG, et al. Surgical treatment of symptomatic Rathke cleft cysts: clinical features and results with special attention to recurrence. J Neurosurg. 2004; 100:33–40. PMID: 14743909.
Article8. Wait SD, Garrett MP, Little AS, Killory BD, White WL. Endocrinopathy, vision, headache, and recurrence after transsphenoidal surgery for Rathke cleft cysts. Neurosurgery. 2010; 67:837–843. PMID: 20657318.
Article9. Kinoshita Y, Tominaga A, Usui S, Arita K, Sakoguchi T, Sugiyama K, et al. The long-term recurrence of Rathke’s cleft cysts as predicted by histology but not by surgical procedure. J Neurosurg. 2016; 125:1002–1007. PMID: 26771852.
Article10. Alomari AK, Kelley BJ, Damisah E, Marks A, Hui P, DiLuna M, et al. Craniopharyngioma arising in a Rathke’s cleft cyst: case report. J Neurosurg Pediatr. 2015; 15:250–254. PMID: 25555112.
Article11. Mendelson ZS, Husain Q, Elmoursi S, Svider PF, Eloy JA, Liu JK. Rathke’s cleft cyst recurrence after transsphenoidal surgery: a meta-analysis of 1151 cases. J Clin Neurosci. 2014; 21:378–385. PMID: 24269553.
Article12. Fager CA, Carter H. Intrasellar epithelial cysts. J Neurosurg. 1966; 24:77–81. PMID: 5903300.
Article13. Baskin DS, Wilson CB. Transsphenoidal treatment of non-neoplastic intrasellar cysts. A report of 38 cases. J Neurosurg. 1984; 60:8–13. PMID: 6689730.14. Kuan EC, Yoo F, Chyu J, Bergsneider M, Wang MB. Treatment outcomes of Rathke’s cleft cysts managed with marsupialization. J Neurol Surg B Skull Base. 2017; 78:112–115. PMID: 28321372.
Article15. Ogawa Y, Watanabe M, Tominaga T. Spontaneous alteration from Rathke’s cleft cyst to craniopharyngioma--possible involvement of transformation between these pathologies. Endocr Pathol. 2014; 25:422–426. PMID: 25154633.
Article16. Schlaffer SM, Buchfelder M, Stoehr R, Buslei R, Hölsken A. Rathke’s cleft cyst as origin of a pediatric papillary craniopharyngioma. Front Genet. 2018; 9:49. PMID: 29520296.
Article17. Park YS, Ahn JY, Kim DS, Kim TS, Kim SH. Late development of craniopharyngioma following surgery for Rathke’s cleft cyst. Clin Neuropathol. 2009; 28:177–181. PMID: 19537134.
Article18. Zada G, Lin N, Ojerholm E, Ramkissoon S, Laws ER. Craniopharyngioma and other cystic epithelial lesions of the sellar region: a review of clinical, imaging, and histopathological relationships. Neurosurg Focus. 2010; 28:E4.
Article19. Brastianos PK, Taylor-Weiner A, Manley PE, Jones RT, Dias-Santagata D, Thorner AR, et al. Exome sequencing identifies BRAF mutations in papillary craniopharyngiomas. Nat Genet. 2014; 46:161–165. PMID: 24413733.