Neurointervention.
2023 Nov;18(3):209-213. 10.5469/neuroint.2023.00451.
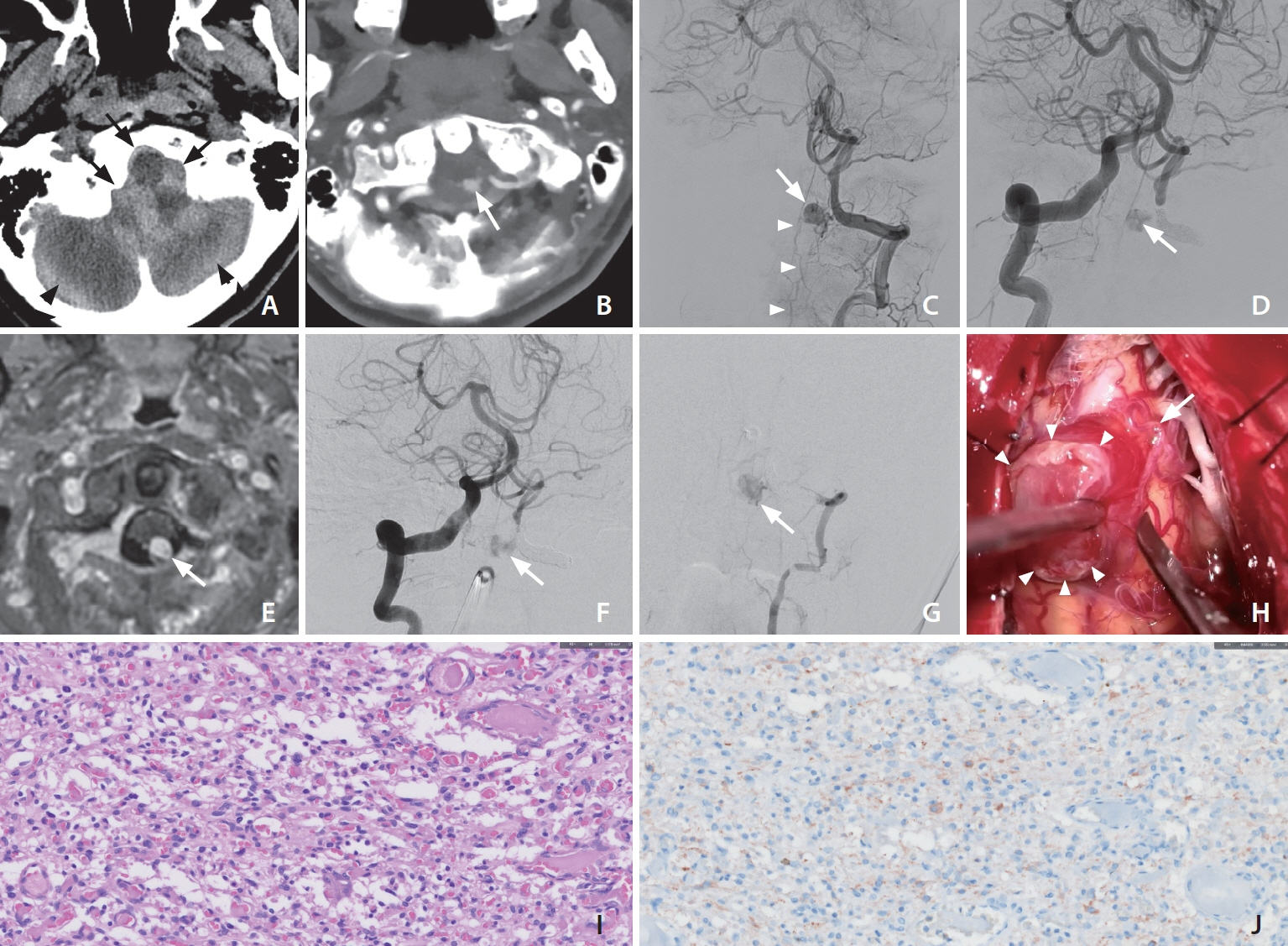
Ruptured Medullary Hemangioblastoma Mimicking a Craniocervical Junction Dural Arteriovenous Fistula with a Pseudoaneurysm
- Affiliations
-
- 1Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Neurosurgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2547285
- DOI: http://doi.org/10.5469/neuroint.2023.00451
Abstract
- Hemangioblastomas (HBMs) are rare vascular tumors commonly located in the posterior fossa of adults. A mid-50s patient presented with sudden unconsciousness. Computed tomography scans revealed acute hemorrhages around the posterior fossa, predominantly in the subarachnoid space. Digital subtraction angiography (DSA) revealed an 8-mm round lesion filled with contrast agent, fed by the C1 segmental artery of the left vertebral artery (VA), showing early venous drainage to the spinal cord and brainstem. Emergent embolization was attempted under suspicion of a ruptured dural arteriovenous fistula, resulting in parent artery occlusion due to feeder selection failure. Follow-up DSA after a month depicted a persistent aneurysm via collaterals from both VAs. Consequently, the decision was made to proceed with surgical intervention, leading to the resection of the lesion, confirming its diagnosis as a HBM through histological examination. This case underscores the potential for misdiagnosis when HBMs with an intratumoral shunt mimic vascular shunt lesions.
Figure
Reference
-
1. Wanebo JE, Lonser RR, Glenn GM, Oldfield EH. The natural history of hemangioblastomas of the central nervous system in patients with von Hippel-Lindau disease. J Neurosurg. 2003; 98:82–94.
Article2. Rachinger J, Buslei R, Prell J, Strauss C. Solid haemangioblastomas of the CNS: a review of 17 consecutive cases. Neurosurg Rev. 2009; 32:37–47. ; discussion 47-48.
Article3. Gupta S, Pal L, Sardhara JC, Jaiswal AK, Srivastava A, Mehrotra A, et al. Recurrent or symptomatic residual posterior fossa hemangioblastomas: how are they different from their primary counterparts? Acta Neurochir (Wien). 2017; 159:1497–1510.
Article4. Ji YC, Li Y, Hu JX, Zhang HB, Yan PX, Zuo HC. Cerebellar hemangioblastoma mimicking an aneurysm: a case report and literature review. Oncol Lett. 2016; 12:2622–2624.
Article5. Kamitani H, Hirano N, Takigawa H, Yokota M, Miyata H, Ohama E, et al. Attenuation of vascularity by preoperative radiosurgery facilitates total removal of a hypervascular hemangioblastoma at the cerebello-pontine angle: case report. Surg Neurol. 2004; 62:238–243. ; discussion 243-244.
Article6. Ho VB, Smirniotopoulos JG, Murphy FM, Rushing EJ. Radiologic-pathologic correlation: hemangioblastoma. AJNR Am J Neuroradiol. 1992; 13:1343–1352.7. Kim JD, Cho MY, Baik SK, Choi SS, Kim CS, Chung CP. MRI findings of intracranial hemangioblastoma. J Korean Radiol Soc. 1995; 33:705–711.
Article8. Baker KB, Moran CJ, Wippold FJ 2nd, Smirniotopoulos JG, Rodriguez FJ, Meyers SP, et al. MR imaging of spinal hemangioblastoma. AJR Am J Roentgenol. 2000; 174:377–382.
Article9. Gelabert González M. [Posterior fossa hemangioblastomas]. Neurologia. 2007; 22:853–859. Spanish.10. Gläsker S, Van Velthoven V. Risk of hemorrhage in hemangioblastomas of the central nervous system. Neurosurgery. 2005; 57:71–76. ; discussion 71-76.
Article11. Tuleasca C, Knafo S, David P, Richard S, Adam C, Aghakhani N, et al. A rare condition: spontaneous subarachnoid haemorrhage due to spinal hemangioblastoma: report of 2 cases and review of the literature. Neurochirurgie. 2020; 66:359–364.
Article12. Persad AR, Khormi YH, van Landeghem F, Chow MM. Unusual case of hemangioblastoma of the cerebellopontine angle. Surg Neurol Int. 2017; 8:264.
Article13. Nishimura Y, Hara M, Natsume A, Takemoto M, Fukuyama R, Wakabayashi T. Intra-extradural dumbbell-shaped hemangioblastoma manifesting as subarachnoid hemorrhage in the cauda equina. Neurol Med Chir (Tokyo). 2012; 52:659–665.
Article14. Rabadán AT, Hernández DA, Paz L. Hemangioblastoma located in the posterior incisural space mimicking a tentorial meningioma: a case report. J Med Case Rep. 2016; 10:183.
Article15. Healy V, O’Halloran PJ, Husien MB, Bolger C, Farrell M. Intermixed arteriovenous malformation and hemangioblastoma: case report and literature review. CNS Oncol. 2020; 9:CNS66.
Article16. Suzuki M, Umeoka K, Kominami S, Morita A. Successful treatment of a ruptured flow-related aneurysm in a patient with hemangioblastoma: case report and review of literature. Surg Neurol Int. 2014; 5(Suppl 9):S430–S433.
Article17. Takeuchi S, Tanaka R, Fujii Y, Abe H, Ito Y. Surgical treatment of hemangioblastomas with presurgical endovascular embolization. Neurol Med Chir (Tokyo). 2001; 41:246–251. ; discussion 251-252.
Article18. Yu J, Xu B, Guo Y, Xu K. Rupture of hemangioblastoma in the posterior part of the fourth ventricle is manifested as a ventricular system hemorrhage: a case report and literature review. Int J Clin Exp Med. 2016; 9:20281–20288.19. Dabus G, Pryor J, Spilberg G, Samaniego EA, Nogueira RG. Embolization of intra-axial hypervascular tumors with onyx: report of three cases. J Neurointerv Surg. 2013; 5:177–180.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Traumatic Intracerebral and Subarachnoid Hemorrhage Due to a Ruptured Pseudoaneurysm of Middle Meningeal Artery Accompanied by a Medial Sphenoid Wing Dural Arteriovenous Fistula
- Brainstem Congestion due to Dural Ateriovenous Fistula at the Craniocervical Junction
- Endovascular Treatment of Spinal Dural and Epidural Arteriovenous Fistula as Complication of Lumbar Surgery
- Stereotactic radiosurgery for dural arteriovenous fistula
- A Case of Dural Arteriovenous Fistula of the Anterior Condylar Vein