Neurointervention.
2023 Nov;18(3):166-171. 10.5469/neuroint.2023.00437.
Endovascular Treatment of Symptomatic Basilar Artery Stenosis
- Affiliations
-
- 1Department of Neurosurgery, Chosun University Hospital, Chosun University College of Medicine, Gwangju, Korea
- 2Department of Neurosurgery, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 3Department of Neurology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 4Department of Radiology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 5Severance Institute for Vascular and Metabolic Research, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2547278
- DOI: http://doi.org/10.5469/neuroint.2023.00437
Abstract
- Purpose
While symptomatic basilar artery (BA) stenosis is associated with a higher risk of recurrent stroke or death, there is no consensus on the management of these patients who are refractory to antiplatelet therapy. This study retrospectively assesses the outcomes of endovascular treatment (EVT) for symptomatic BA stenosis.
Materials and Methods
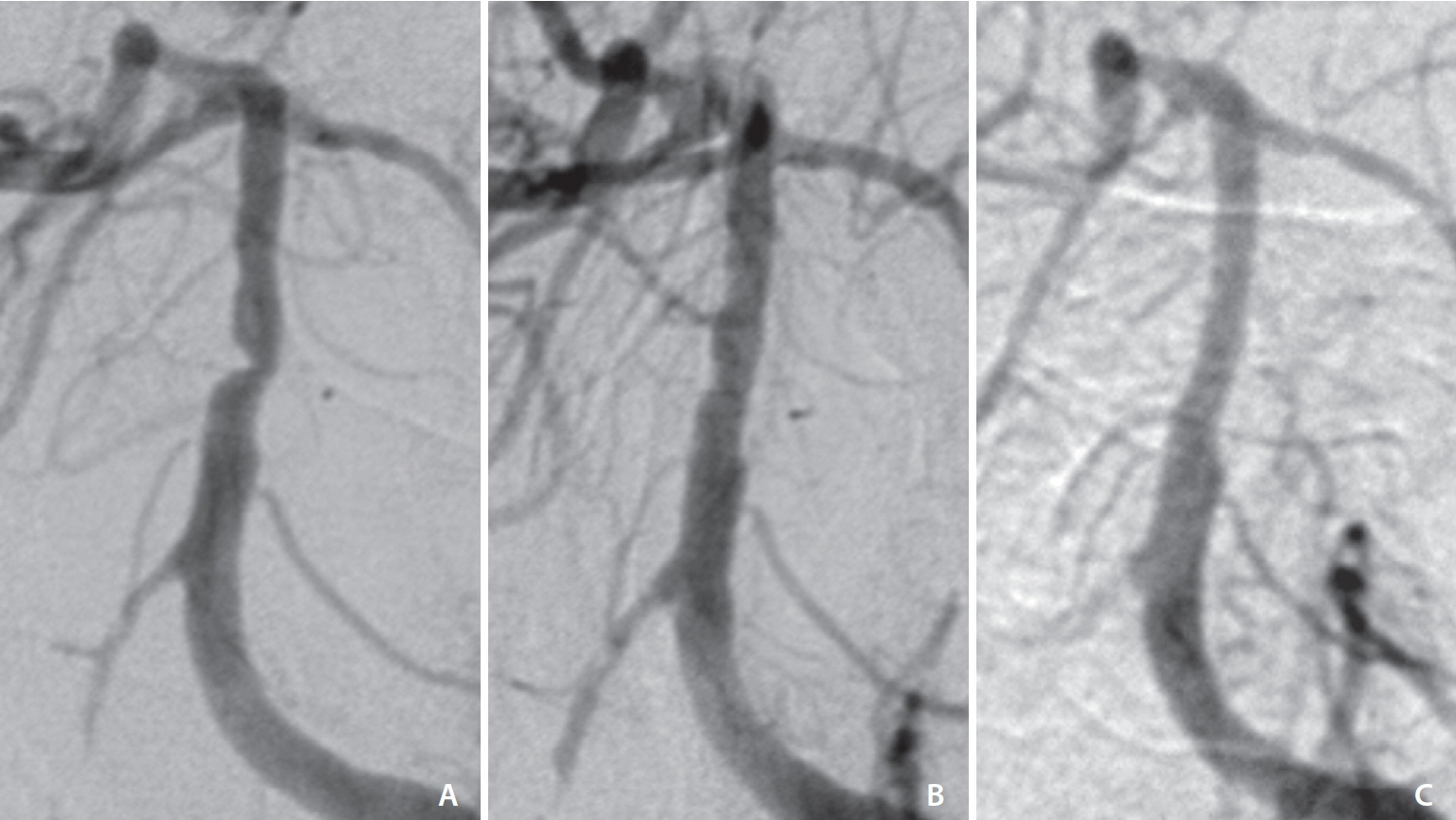
We conducted a retrospective review of patients with symptomatic BA stenosis who underwent EVT, including angioplasty or stenting, from 2006 to 2018. A total of 15 patients, who experienced transient ischemic attacks or strokes despite dual antiplatelet therapy, were included. EVT was performed under local anesthesia after pretreatment with antiplatelet medications. Angiographic follow-up was performed at 12 and 24 months post-EVT. Clinical outcomes were evaluated using the modified Rankin Scale (mRS).
Results
EVT was successfully completed in all patients. Peri/post-procedural complications occurred in 33% of cases, including in-stent thrombosis, intracranial hemorrhage, and pontine infarction. At long-term follow-up (mean 98.5±80.5 months), 73.3% of patients achieved a favorable functional outcome (mRS≤2) without disability or mortality. Patients with unfavorable outcomes had previous infarcts, with 2 experiencing new pontine infarctions after stenting.
Conclusion
This study suggests that EVT, including angioplasty and stenting, may offer promise as a treatment option for symptomatic BA stenosis refractory to medical therapy. However, the procedure carries a notable risk of complications, especially in patients with severe stenosis and previous infarcts. Careful patient selection, based on clinical and radiological criteria, is crucial.
Keyword
Figure
Reference
-
1. Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y, CICAS Study Group, et al. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke. 2014; 45:663–669.
Article2. Wong LK. Global burden of intracranial atherosclerosis. Int J Stroke. 2006; 1:158–159.
Article3. Caplan LR, Wityk RJ, Glass TA, Tapia J, Pazdera L, Chang HM, et al. New England Medical Center posterior circulation registry. Ann Neurol. 2004; 56:389–398.
Article4. Arai M. [Wallenberg’s syndrome following minor neck trauma: a case associated with atlanto-axial subluxation, an anomaly of the axis, and platelet activation]. Rinsho Shinkeigaku. 1995; 35:670–672. Japanese.5. Prognosis of patients with symptomatic vertebral or basilar artery stenosis. The warfarin-aspirin symptomatic intracranial disease (WASID) study group. Stroke. 1998; 29:1389–1392.6. Derdeyn CP, Fiorella D, Lynn MJ, Rumboldt Z, Cloft HJ, Gibson D, Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis Trial Investigators, et al. Mechanisms of stroke after intracranial angioplasty and stenting in the SAMMPRIS trial. Neurosurgery. 2013; 72:777–795. ; discussion 795.
Article7. Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, SAMMPRIS Trial Investigators, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011; 365:993–1003.8. Thijs VN, Albers GW. Symptomatic intracranial atherosclerosis: outcome of patients who fail antithrombotic therapy. Neurology. 2000; 55:490–497.
Article9. Mori T, Fukuoka M, Kazita K, Mori K. Follow-up study after intracranial percutaneous transluminal cerebral balloon angioplasty. AJNR Am J Neuroradiol. 1998; 19:1525–1533.
Article10. Samaniego EA, Shaban A, Ortega-Gutierrez S, Roa JA, Hasan DM, Derdeyn C, et al. Stroke mechanisms and outcomes of isolated symptomatic basilar artery stenosis. Stroke Vasc Neurol. 2019; 4:189–197.
Article11. Gulli G, Marquardt L, Rothwell PM, Markus HS. Stroke risk after posterior circulation stroke/transient ischemic attack and its relationship to site of vertebrobasilar stenosis: pooled data analysis from prospective studies. Stroke. 2013; 44:598–604.
Article12. Jiang WJ, Xu XT, Du B, Dong KH, Jin M, Wang QH, et al. Long-term outcome of elective stenting for symptomatic intracranial vertebrobasilar stenosis. Neurology. 2007; 68:856–858.
Article13. Bai WX, Gao BL, Li TX, Wang ZL, Cai DY, Zhu LF, et al. Wingspan stenting can effectively prevent long-term strokes for patients with severe symptomatic atherosclerotic basilar stenosis. Interv Neuroradiol. 2016; 22:318–324.
Article14. Jia B, Liebeskind DS, Ma N, Gao F, Mo D, Luo G, et al. Factors associated with perforator stroke after selective basilar artery angioplasty or stenting. J Neurointerv Surg. 2017; 9:738–742.
Article15. Maier IL, Karch A, Lipke C, Behme D, Mpotsaris A, Kabbasch C, et al. Transluminal angioplasty and stenting versus conservative treatment in patients with symptomatic basilar artery stenosis: perspective for future clinical trials. Clin Neuroradiol. 2018; 28:33–38.
Article16. Luo J, Bai X, Huang K, Wang T, Yang R, Li L, et al. Clinical relevance of plaque distribution for basilar artery stenosis. AJNR Am J Neuroradiol. 2023; 44:530–535.
Article17. Yang WJ, Fisher M, Zheng L, Niu CB, Paganini-Hill A, Zhao HL, et al. Histological characteristics of intracranial atherosclerosis in a Chinese population: a postmortem study. Front Neurol. 2017; 8:488.
Article18. Yu JH, Kwak HS, Chung GH, Hwang SB, Park MS, Park SH. Association of intraplaque hemorrhage and acute infarction in patients with basilar artery plaque. Stroke. 2015; 46:2768–2772.
Article19. Roth W, Morgello S, Goldman J, Mohr JP, Elkind MS, Marshall RS, et al. Histopathological differences between the anterior and posterior brain arteries as a function of aging. Stroke. 2017; 48:638–644.
Article20. Baik SH, Kim JY, Jung C. A review of endovascular treatment for posterior circulation strokes. Neurointervention. 2023; 18:90–106.
Article21. Jiang WJ, Du B, Hon SF, Jin M, Xu XT, Ma N, et al. Do patients with basilar or vertebral artery stenosis have a higher stroke incidence poststenting? J Neurointerv Surg. 2010; 2:50–54.
Article22. Palmisciano P, Hoz SS, Algburi HA, Ventre G, Street S, Agyeman N, et al. Percutaneous transluminal angioplasty and/or stenting for the treatment of basilar artery stenosis: a systematic review and meta-analysis. Neuroradiology. 2023; 65:985–1000.
Article23. Huang K, Yao W, Zha M, Qin S, Li Y, Xu Y, et al. Angiography-based hemodynamic features predict recurrent ischemic events after angioplasty and stenting of intracranial vertebrobasilar atherosclerotic stenosis. [published online ahead of print Sep 19, 2023] Eur Radiol 2023.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of High-Grade Basilar Artery Stenosis by Primary Stenting
- Locked-in Syndrome Performed Endovascular Treatment for Vertebral Artery Dissection and Basilar Artery Occlusion Caused by a Golf Swing
- Kissing Aneurysms at Fenestrated Proximal Basilar Artery: Double-barrel Stent-assisted Coiling Using Dual Closed-cell Stents
- Endovascular Treatment of Giant Basilar Trunk Aneurysm: Case Report
- A Case of ReVersible Basilar Artery Stenosis in Neuro-Behcet's Disease