J Stroke.
2023 Sep;25(3):361-370. 10.5853/jos.2023.00626.
Association of Unfavorable Social Determinants of Health With Stroke/Transient Ischemic Attack and Vascular Risk Factors in Hispanic/Latino Adults: Results From Hispanic Community Health Study/Study of Latinos
- Affiliations
-
- 1Department of Neurology and Rehabilitation, University of Illinois at Chicago College of Medicine, Chicago, IL, USA
- 2Department of Psychology, San Diego State University, San Diego, CA, USA
- 3Rush Alzheimer’s Disease Center and Department of Psychiatry and Behavioral Sciences, Rush University, Chicago, IL, USA
- 4Department of Medicine, Institute for Minority Health Research, University of Illinois at Chicago, Chicago, IL, USA
- 5Department of Social Medicine, School of Medicine, University of North Carolina, Chapel Hill, NC, USA
- 6Department of Psychology, San Diego State University, San Diego, CA, USA
- 7Department of Epidemiology and Population Health, Albert Einstein College of Medicine, Bronx, NY, USA
- 8Department of Biostatistics, Gillings School of Global Public Health, University of North Carolina, Chapel Hill, NC, USA
- KMID: 2546437
- DOI: http://doi.org/10.5853/jos.2023.00626
Abstract
- Background and Purpose
Social determinants of health (SDOH) are non-medical factors that may contribute to the development of diseases, with a higher representation in underserved populations. Our objective is to determine the association of unfavorable SDOH with self-reported stroke/transient ischemic attack (TIA) and vascular risk factors (VRFs) among Hispanic/Latino adults living in the US.
Methods
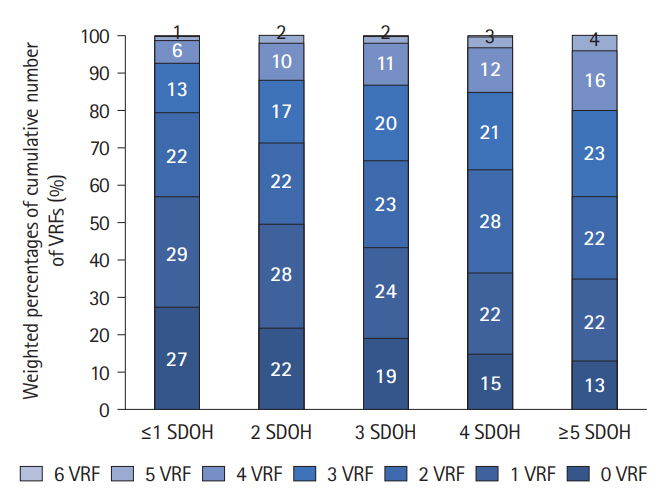
We used cross-sectional data from the Hispanic Community Health Study/Study of Latinos. SDOH and VRFs were assessed using questionnaires and validated scales and measurements. We investigated the association between the SDOH (individually and as count: ≤1, 2, 3, 4, or ≥5 SDOH), VRFs and stroke/TIA using regression analyses.
Results
For individuals with stroke/TIA (n=388), the mean age (58.9 years) differed from those without stroke/TIA (n=11,210; 46.8 years; P<0.0001). In bivariate analysis, income <$20,000, education less than high school, no health insurance, perceived discrimination, not currently employed, upper tertile for chronic stress, and lower tertiles for social support and language- and social-based acculturation were associated with stroke/TIA and retained further. A higher number of SDOH was directly associated with all individual VRFs investigated, except for at-risk alcohol, and with number of VRFs (β=0.11, 95% confidence interval [CI]=0.09–0.14). In the fully adjusted model, income, discrimination, social support, chronic stress, and employment status were individually associated with stroke/TIA; the odds of stroke/TIA were 2.3 times higher in individuals with 3 SDOH (95% CI 1.6–3.2) and 2.7 times (95% CI 1.9–3.7) for those with ≥5 versus ≤1 SDOH.
Conclusion
Among Hispanic/Latino adults, a higher number of SDOH is associated with increased odds for stroke/TIA and VRFs. The association remained significant after adjustment for VRFs, suggesting involvement of non-vascular mechanisms.
Figure
Reference
-
References
1. Morgenstern LB, Smith MA, Lisabeth LD, Risser JM, Uchino K, Garcia N, et al. Excess stroke in Mexican Americans compared with non-Hispanic Whites: the Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol. 2004; 160:376–383.2. Levine DA, Duncan PW, Nguyen-Huynh MN, Ogedegbe OG. Interventions targeting racial/ethnic disparities in stroke prevention and treatment. Stroke. 2020; 51:3425–3432.3. Guadamuz JS, Durazo-Arvizu RA, Daviglus ML, Perreira KM, Calip GS, Nutescu EA, et al. Immigration status and disparities in the treatment of cardiovascular disease risk factors in the Hispanic Community Health Study/Study of Latinos (visit 2, 2014–2017). Am J Public Health. 2020; 110:1397–1404.4. Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015; 132:873–898.5. Reshetnyak E, Ntamatungiro M, Pinheiro LC, Howard VJ, Carson AP, Martin KD, et al. Impact of multiple social determinants of health on incident stroke. Stroke. 2020; 51:2445–2453.6. Chambers EC, Hanna DB, Hua S, Duncan DT, Camacho-Rivera M, Zenk SN, et al. Relationship between area mortgage foreclosures, homeownership, and cardiovascular disease risk factors: the Hispanic Community Health Study/Study of Latinos. BMC Public Health. 2019; 19:77.7. Hernandez R, Carnethon M, Giachello AL, Penedo FJ, Wu D, Birnbaum-Weitzman O, et al. Structural social support and cardiovascular disease risk factors in Hispanic/Latino adults with diabetes: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Ethn Health. 2018; 23:737–751.8. Sorlie PD, Avilés-Santa LM, Wassertheil-Smoller S, Kaplan RC, Daviglus ML, Giachello AL, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010; 20:629–641.9. Hamilton CM, Strader LC, Pratt JG, Maiese D, Hendershot T, Kwok RK, et al. The PhenX Toolkit: get the most from your measures. Am J Epidemiol. 2011; 174:253–260.10. American Academy of Family Physicians. The everyONE projectTM [Internet]. Leawood, KS: American Academy of Family Physicians;[cited 2022 Oct 18]. Available from: https://www.aafp.org/dam/AAFP/documents/patient_care/everyone_project/hops19-physician-guide-sdoh.pdf.11. Finch BK, Hummer RA, Kol B, Vega WA. The role of discrimination and acculturative stress in the physical health of Mexican-origin adults. Hisp J Behav Sci. 2001; 23:399–429.12. Cohen S, Mermelstein RJ, Kamarck TW, Hoberman HM. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social Support: Theory, Research and Applications. Dordrecht: Springer;1985. p. 73–94.13. Lanz M, Maino E. Family environment scale. In: Michalos AC, editor. Encyclopedia of Quality of Life and Well-Being Research. Dordrecht: Springer;2014. p. 2170–2174.14. Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987; 9:183–205.15. Bromberger JT, Matthews KA. A longitudinal study of the effects of pessimism, trait anxiety, and life stress on depressive symptoms in middle-aged women. Psychol Aging. 1996; 11:207–213.16. Shivpuri S, Gallo LC, Crouse JR, Allison MA. The association between chronic stress type and C-reactive protein in the multi-ethnic study of atherosclerosis: does gender make a difference? J Behav Med. 2012; 35:74–85.17. Arellano-Morales L, Roesch SC, Gallo LC, Emory KT, Molina KM, Gonzalez P, et al. Prevalence and correlates of perceived ethnic discrimination in the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. J Lat Psychol. 2015; 3:160–176.18. Dimitrov DM. Testing for factorial invariance in the context of construct validation. Meas Eval Couns Dev. 2010; 43:121–149.19. Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychol. 2003; 22:300–309.20. McGuire S. U.S. Department of Agriculture and U.S. Department of Health and Human Services, Dietary Guidelines for Americans, 2010. 7th edition, Washington, DC: U.S. Government Printing Office, January 2011. Adv Nutr. 2011; 2:293–294.21. Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:2160–2236.22. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018; 71:1269–1324.23. Javed Z, Haisum Maqsood M, Yahya T, Amin Z, Acquah I, Valero-Elizondo J, et al. Race, racism, and cardiovascular health: applying a social determinants of health framework to racial/ethnic disparities in cardiovascular disease. Circ Cardiovasc Qual Outcomes. 2022; 15:e007917.24. Skolarus LE, Sharrief A, Gardener H, Jenkins C, Boden-Albala B. Considerations in addressing social determinants of health to reduce racial/ethnic disparities in stroke outcomes in the United States. Stroke. 2020; 51:3433–3439.25. Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. 2018; 137:2166–2178.26. Rodriguez CJ, Allison M, Daviglus ML, Isasi CR, Keller C, Leira EC, et al. Status of cardiovascular disease and stroke in Hispanics/Latinos in the United States: a science advisory from the American Heart Association. Circulation. 2014; 130:593–625.27. Christine PJ, Auchincloss AH, Bertoni AG, Carnethon MR, Sánchez BN, Moore K, et al. Longitudinal associations between neighborhood physical and social environments and incident type 2 diabetes mellitus: the Multi-Ethnic Study of Atherosclerosis (MESA). JAMA Intern Med. 2015; 175:1311–1320.28. Kaiser P, Diez Roux AV, Mujahid M, Carnethon M, Bertoni A, Adar SD, et al. Neighborhood environments and incident hypertension in the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2016; 183:988–997.29. Daviglus ML, Talavera GA, Avilés-Santa ML, Allison M, Cai J, Criqui MH, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012; 308:1775–1784.30. Piedra LM, Andrade FCD, Hernandez R, Perreira KM, Gallo LC, González HM, et al. Association of subjective social status with life’s simple 7s cardiovascular health index among Hispanic/Latino people: results from the HCHS/SOL. J Am Heart Assoc. 2021; 10:e012704.31. Gardener H, Sacco RL, Rundek T, Battistella V, Cheung YK, Elkind MSV. Race and ethnic disparities in stroke incidence in the Northern Manhattan Study. Stroke. 2020; 51:1064–1069.32. Langagergaard V, Palnum KH, Mehnert F, Ingeman A, Krogh BR, Bartels P, et al. Socioeconomic differences in quality of care and clinical outcome after stroke: a nationwide population-based study. Stroke. 2011; 42:2896–2902.33. Wagner JA, Tennen H, Feinn R, Osborn CY. Self-reported discrimination, diabetes distress, and continuous blood glucose in women with type 2 diabetes. J Immigr Minor Health. 2015; 17:566–573.34. McCurley JL, Mills PJ, Roesch SC, Carnethon M, Giacinto RE, Isasi CR, et al. Chronic stress, inflammation, and glucose regulation in U.S. Hispanics from the HCHS/SOL sociocultural ancillary study. Psychophysiology. 2015; 52:1071–1079.35. Sparrenberger F, Cichelero FT, Ascoli AM, Fonseca FP, Weiss G, Berwanger O, et al. Does psychosocial stress cause hypertension? A systematic review of observational studies. J Hum Hypertens. 2009; 23:12–19.36. Gallo LC, Roesch SC, Fortmann AL, Carnethon MR, Penedo FJ, Perreira K, et al. Associations of chronic stress burden, perceived stress, and traumatic stress with cardiovascular disease prevalence and risk factors in the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. Psychosom Med. 2014; 76:468–475.37. Booth J, Connelly L, Lawrence M, Chalmers C, Joice S, Becker C, et al. Evidence of perceived psychosocial stress as a risk factor for stroke in adults: a meta-analysis. BMC Neurol. 2015; 15:233.38. Mannoh I, Hussien M, Commodore-Mensah Y, Michos ED. Impact of social determinants of health on cardiovascular disease prevention. Curr Opin Cardiol. 2021; 36:572–579.39. Artiga S, Hinton E. Beyond health care: the role of social determinants in promoting health and health equity [Internet]. San Francisco, CA: KFF;[cited 2023 Jan 21]. Available from: https://www.kff.org/racial-equity-and-health-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/.40. Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circulation. 2023; 147:e93–e621.41. Galobardes B, Lynch J, Smith GD. Measuring socioeconomic position in health research. Br Med Bull. 2007; 81-82:21–37.42. Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021; 52:e364–e467.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Malnutrition Risk in Community-Dwelling Older Adults with Dual Sensory Declines: Focusing on Social Determinants of Health
- Antiplatelet Therapy for Secondary Stroke Prevention in Patients with Ischemic Stroke or Transient Ischemic Attack
- Cerebrovascular Disease : Overview and Classification
- Selective Gray Matter Infarction in the Basal Ganglia Associated With Transient Ischemic Attack
- Small Vessel Transient Ischemic Attack and Lacunar Infarction Detected with Perfusion-Weighted MRI