Pediatr Emerg Med J.
2023 Oct;10(4):175-181. 10.22470/pemj.2023.00808.
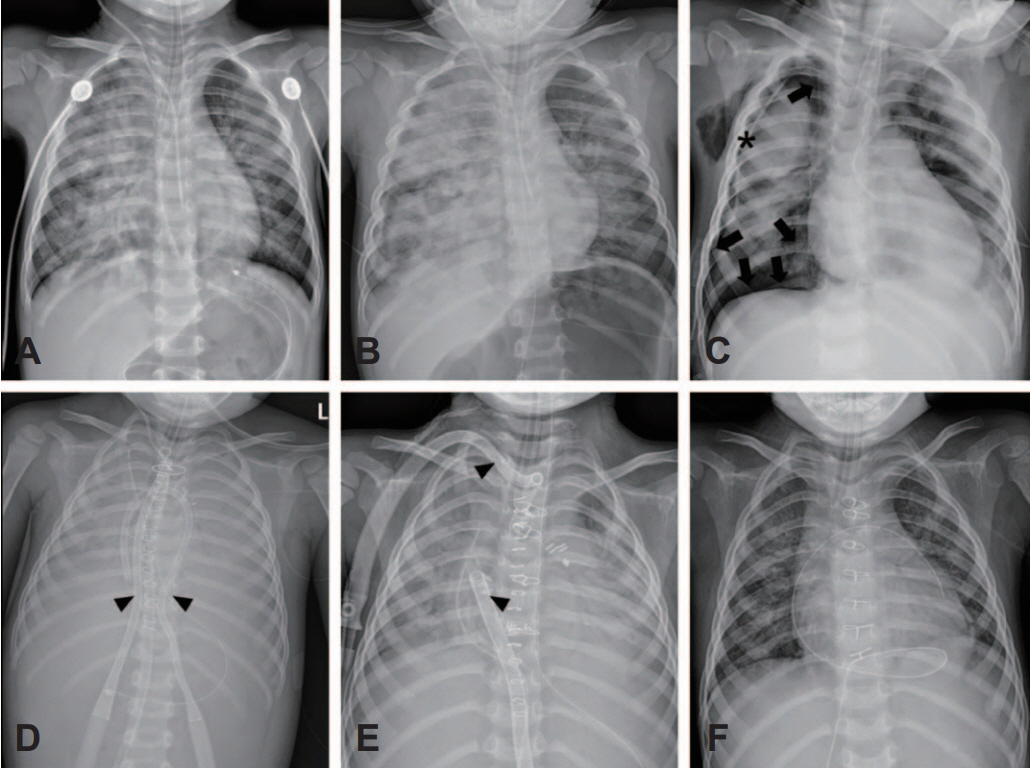
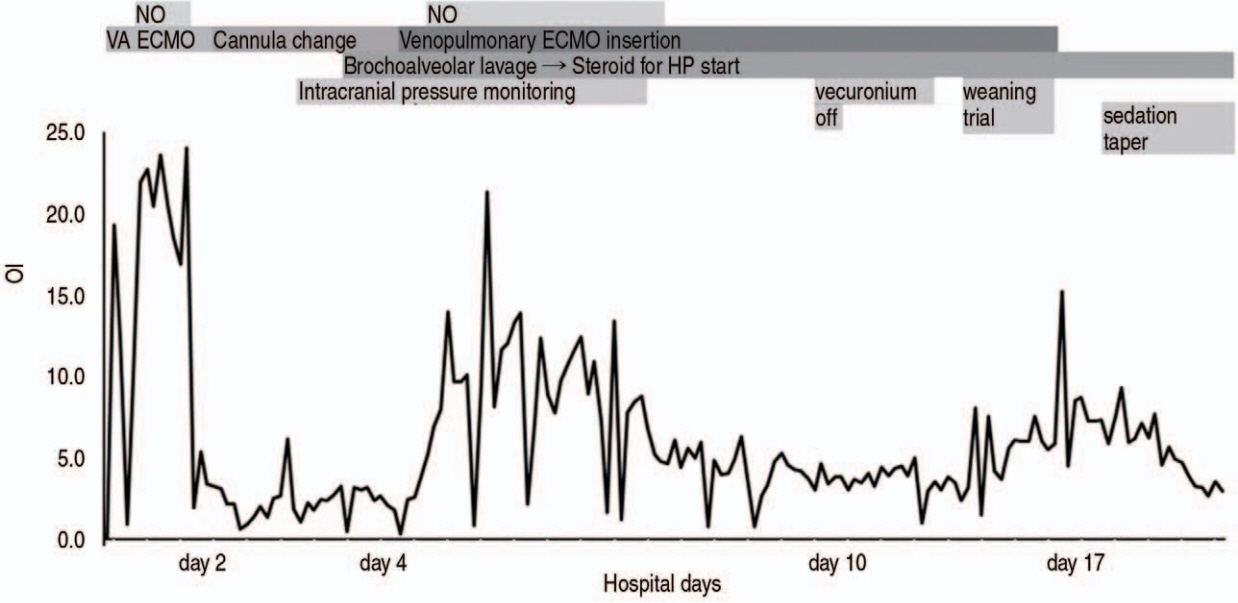
A 35-month-old boy who ingested laundry detergent pods and underwent veno-pulmonary extracorporeal membrane oxygenation support
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children’s Hospital, Seoul National University College of Medicine, Seoul, Republic of Korea
- 2Integrated Care Center, Seoul National University Hospital, Seoul, Republic of Korea
- 3Department of Emergency Medicine, Seoul National University Hospital, Seoul, Republic of Korea
- 4Department of Thoracic and Cardiovascular Surgery, Seoul National University Children’s Hospital, Seoul National University College of Medicine, Seoul, Republic of Korea
- KMID: 2546294
- DOI: http://doi.org/10.22470/pemj.2023.00808
Abstract
- Laundry detergent pod (LDP) exposure has been reported to be fatal in children younger than 2 years, leading to respiratory or central nervous system depression. While gastrointestinal irritation is the most common symptom, there are reported cases of severe acidosis with respiratory depression or pneumonia, resulting in mortality. To our best knowledge, there is no report on a case of LDP exposure presenting with acute respiratory distress syndrome requiring extracorporeal membrane oxygenation support. Here, we present a case of a child with severe acute respiratory distress syndrome following LDP exposure, who was successfully treated with veno-pulmonary extracorporeal membrane oxygenation and steroids.
Keyword
Figure
Reference
-
References
1. Centers for Disease Control and Prevention (CDC). Health hazards associated with laundry detergent pods - United States, May-June 2012. MMWR Morb Mortal Wkly Rep. 2012; 61:825–9.2. Roh DE. Laundry detergent pod: a rising cause of household poisoning. Pediatr Emerg Med J. 2020; 7:131–4.3. Rigaux-Barry F, Patat AM, Cordier L, Manel J, Sinno-Tellier S. Risks related to pods exposure compared to traditional laundry detergent products: study of cases recorded by French PCC from 2005 to 2012. Toxicol Anal Clin. 2017; 29:257–66.4. Settimi L, Giordano F, Lauria L, Celentano A, Sesana F, Davanzo F. Surveillance of paediatric exposures to liquid laundry detergent pods in Italy. Inj Prev. 2018; 24:5–11.5. Day R, Bradberry SM, Thomas SHL, Vale JA. Liquid laundry detergent capsules (PODS): a review of their composition and mechanisms of toxicity, and of the circumstances, routes, features, and management of exposure. Clin Toxicol (Phila). 2019; 57:1053–63.6. Williams H, Bateman DN, Thomas SH, Thompson JP, Scott RA, Vale JA. Exposure to liquid detergent capsules: a study undertaken by the UK National Poisons Information Service. Clin Toxicol (Phila). 2012; 50:776–80.7. Banner W, Yin S, Burns MM, Lucas R, Reynolds KM, Green JL. Clinical characteristics of exposures to liquid laundry detergent packets. Hum Exp Toxicol. 2020; 39:95–110.8. van Heemst RC, Sander I, Rooyackers J, de Jong L, Djamin RS, Aerts JG, et al. Hypersensitivity pneumonitis caused by occupational exposure to phytase. Eur Respir J. 2009; 33:1507–9.9. Patel A, Hasany A, Tarlo SM. Occupational hypersensitivity pneumonitis after polyurethane adhesive exposure. CMAJ. 2022; 194:E1027–30.10. Beuhler MC, Gala PK, Wolfe HA, Meaney PA, Henretig FM. Laundry detergent“ pod”ingestions: a case series and discussion of recent literature. Pediatr Emerg Care. 2013; 29:743–7.11. Nieuwenhuizen L, de Groot PG, Grutters JC, Biesma DH. A review of pulmonary coagulopathy in acute lung injury, acute respiratory distress syndrome and pneumonia. Eur J Haematol. 2009; 82:413–25.12. Sobiecka M, Szturmowicz M, Lewandowska K, Kowalik A, Łyz´wa E, Zimna K, et al. Chronic hypersensitivity pneumonitis is associated with an increased risk of venous thromboembolism: a retrospective cohort study. BMC Pulm Med. 2021; 21:416.13. Lal A, Akhtar J, Pinto S, Grewal H, Martin K. Recurrent pulmonary embolism and hypersensitivity pneumonitis secondary to Aspergillus, in a compost plant worker: case report and review of literature. Lung. 2018; 196:553–60.14. Zochios V, Yusuff H, Antonini MV, Schmidt M, Shekar K; for Protecting the Right Ventricle Network (PRORVnet). Veno-pulmonary arterial extracorporeal membrane oxygenation in severe acute respiratory distress syndrome: should we consider mechanical support of the pulmonary circulation from the outset? ASAIO J. 2023; 69:511–8.15. Oh DK, Shim TS, Jo KW, Park SI, Kim DK, Choi S, et al. Right ventricular assist device with an oxygenator using extracorporeal membrane oxygenation as a bridge to lung transplantation in a patient with severe respiratory failure and right heart decompensation. Acute Crit Care. 2020; 35:117–21.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laundry detergent pod: a rising cause of household poisoning
- Whole Lung Lavage in Pulmonary Alveolar Proteinosis associated with Lung Cancer Using Extracorporeal Membrane Oxygenation (ECMO)
- Extracorporeal Membrane Oxygenation for Complicated Scrub Typhus
- Veno-venous Extracorporeal Membrane Oxygenation with a Double Lumen Catheter for Pediatric Pulmonary Support
- A case of rescuing a patient with acute cardiovascular instability from sudden and massive intraoperative pulmonary thromboembolism by extracorporeal membrane oxygenation