Clin Endosc.
2023 Sep;56(5):650-657. 10.5946/ce.2022.190.
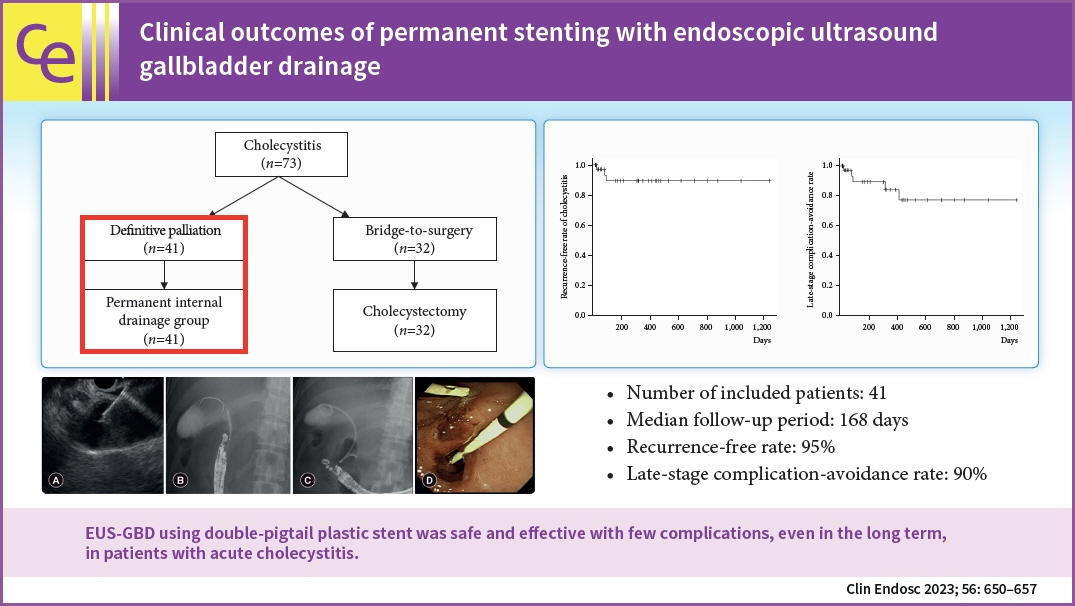
Clinical outcomes of permanent stenting with endoscopic ultrasound gallbladder drainage
- Affiliations
-
- 1Department of Hepato-Biliary-Pancreatic Medicine, NTT Tokyo Medical Center, Tokyo, Japan
- 2Department of Gastroenterology, NTT Tokyo Medical Center, Tokyo, Japan
- 3Department of Gastroenterology and Hepatology, Yokohama City University School of Medicine, Yokohama, Japan
- KMID: 2546143
- DOI: http://doi.org/10.5946/ce.2022.190
Abstract
- Background/Aims
Endoscopic ultrasound gallbladder drainage (EUS-GBD) is gaining attention as a treatment method for cholecystitis. However, only a few studies have assessed the outcomes of permanent stenting with EUS-GBD. Therefore, we evaluated the clinical outcomes of permanent stenting using EUS-GBD.
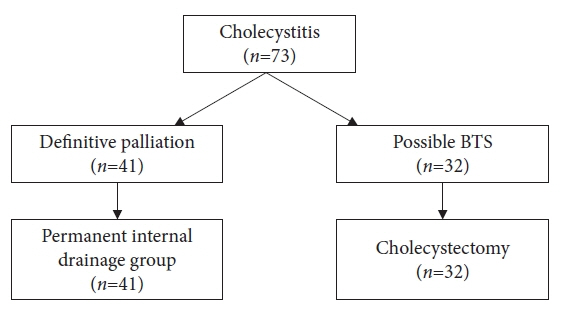
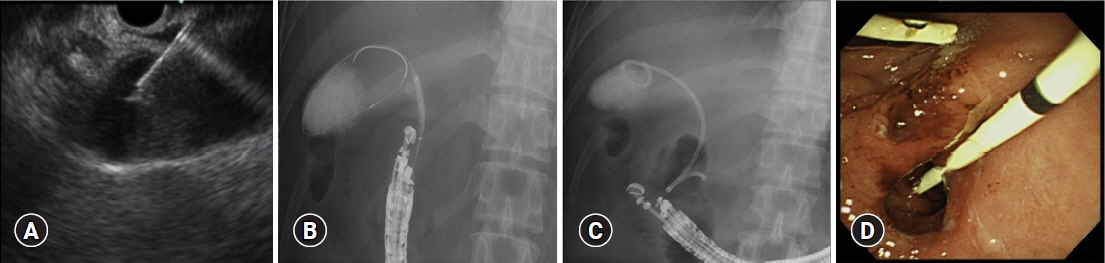
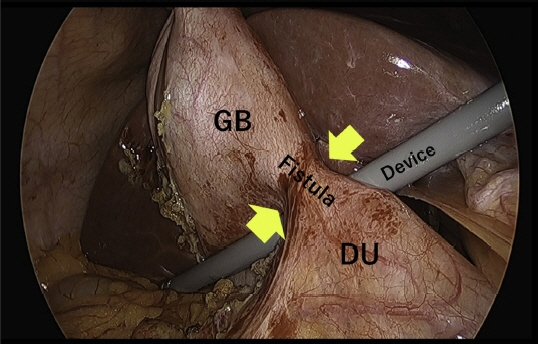
Methods
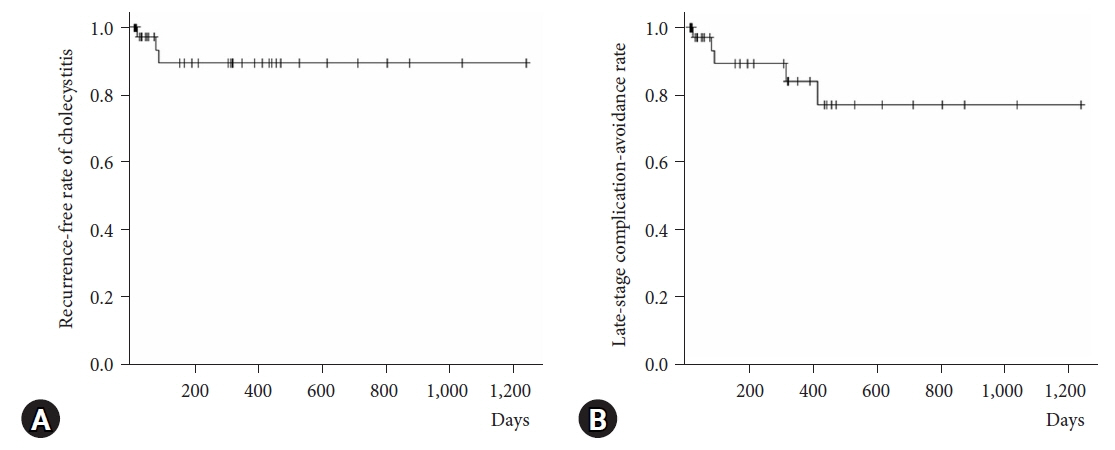
This was a retrospective, single-center cohort study. The criteria for EUS-GBD at our institution are a high risk for surgery, inability to perform surgery owing to poor performance status, and inability to obtain consent for emergency surgery. EUS-GBD was performed using a 7-Fr double-pigtail plastic stent with a dilating device. The primary outcomes were the recurrence-free rate of cholecystitis and the late-stage complication-avoidance rate. Secondary outcomes were technical success, clinical success, and procedural adverse events.
Results
A total of 41 patients were included in the analysis. The median follow-up period was 168 (range, 10–1,238) days. The recurrence-free and late-stage complication-avoidance rates during the follow-up period were 95% (38 cases) and 90% (36 cases), respectively. There were only two cases of cholecystitis recurrence during the study period.
Conclusions
EUS-GBD using double-pigtail plastic stent was safe and effective with few complications, even in the long term, in patients with acute cholecystitis.
Keyword
Figure
Reference
-
1. Takada T. Tokyo Guidelines 2018: updated Tokyo Guidelines for the management of acute cholangitis/acute cholecystitis. J Hepatobiliary Pancreat Sci. 2018; 25:1–2.2. Melin MM, Sarr MG, Bender CE, et al. Percutaneous cholecystostomy: a valuable technique in high-risk patients with presumed acute cholecystitis. Br J Surg. 1995; 82:1274–1277.3. Wiersema MJ, Sandusky D, Carr R, et al. Endosonography-guided cholangiopancreatography. Gastrointest Endosc. 1996; 43(2 Pt 1):102–106.4. Giovannini M, Moutardier V, Pesenti C, et al. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy. 2001; 33:898–900.5. Anderloni A, Buda A, Vieceli F, et al. Endoscopic ultrasound-guided transmural stenting for gallbladder drainage in high-risk patients with acute cholecystitis: a systematic review and pooled analysis. Surg Endosc. 2016; 30:5200–5208.6. Matsubara S, Isayama H, Nakai Y, et al. Endoscopic ultrasound-guided gallbladder drainage with a combined internal and external drainage tubes for acute cholecystitis. J Gastroenterol Hepatol. 2020; 35:1821–1827.7. Ryozawa S, Fujita N, Irisawa A, et al. Current status of interventional endoscopic ultrasound. Dig Endosc. 2017; 29:559–566.8. Dhir V, Isayama H, Itoi T, et al. Endoscopic ultrasonography-guided biliary and pancreatic duct interventions. Dig Endosc. 2017; 29:472–485.9. Lee SS, Park DH, Hwang CY, et al. EUS-guided transmural cholecystostomy as rescue management for acute cholecystitis in elderly or high-risk patients: a prospective feasibility study. Gastrointest Endosc. 2007; 66:1008–1012.10. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010; 71:446–454.11. Perez-Miranda M. Technical considerations in EUS-guided gallbladder drainage. Endosc Ultrasound. 2018; 7:79–82.12. James TW, Baron TH. EUS-guided gallbladder drainage: a review of current practices and procedures. Endosc Ultrasound. 2019; 8(Suppl 1):S28–S34.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Transpapillary Gallbladder Stenting for Acute Cholecystitis in a Patient with Metastatic Pancreatic Cancer
- Stent occlusion in endoscopic ultrasound-guided gallbladder drainage from bleeding mitigated by double pigtail plastic stent deployment within lumen apposing metal stent
- Single-pigtail plastic stent made from endoscopic nasobiliary drainage tubes in endoscopic ultrasound-guided gallbladder drainage: a retrospective case series
- Endoscopic Gallbladder Drainage for Acute Cholecystitis
- Current Status of Endoscopic Gallbladder Drainage