Obstet Gynecol Sci.
2023 Sep;66(5):395-406. 10.5468/ogs.22251.
High prevalence of hypovitaminosis D3 among pregnant women in central Iran: correlation with newborn vitamin D3 levels and negative association with gestational age
- Affiliations
-
- 1Infectious Disease Research Center, Arak University of Medical Sciences, Arak, Iran
- 2School of Medicine, Arak University of Medical Sciences, Arak, Iran
- 3Department of Research and Development, Islamic Azad University of Khomeyn (IAUK), Khomeyn, Iran
- 4Department of Pediatrics, Arak University of Medical Sciences, Arak, Iran
- 5Department of Obstetrics and Gynecology, Arak University of Medical Sciences, Arak, Iran
- 6Student Research Committee, Khomein University of Medical Sciences, Khomein, Iran
- 7Department of Basic and Laboratory Sciences, Khomein University of Medical Sciences, Khomein, Iran
- KMID: 2545886
- DOI: http://doi.org/10.5468/ogs.22251
Abstract
Objective
Hypovitaminosis D3 is a significant concern among pregnant women and their newborns because vitamin D3 (Vit-D3) plays a crucial role in embryonic growth, development, and health. This study aimed to evaluate the Vit-D3 status of a group of pregnant Iranian women and its association with newborn Vit-D3 levels, medical and clinical indices after delivery.
Methods
A total of 206 pregnant women and their newborns were assessed for Vit-D3 levels and their correlation with gestational age. Mean±standard deviation (SD) or the orders (non-parametric tests) of variables were compared, and correlation estimations were performed to elucidate any differences or associations between groups, with a confidence interval of at least 0.95.
Results
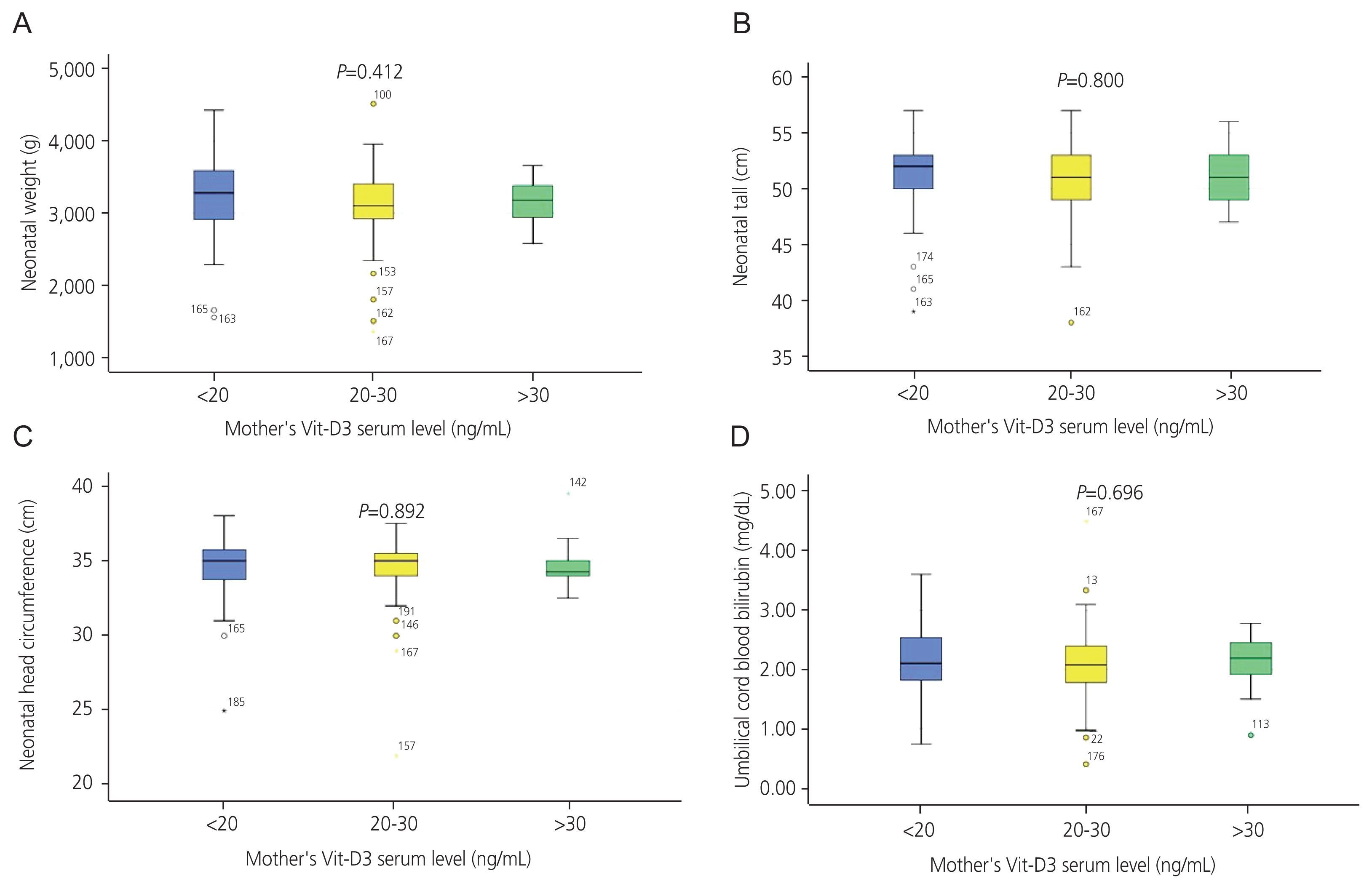
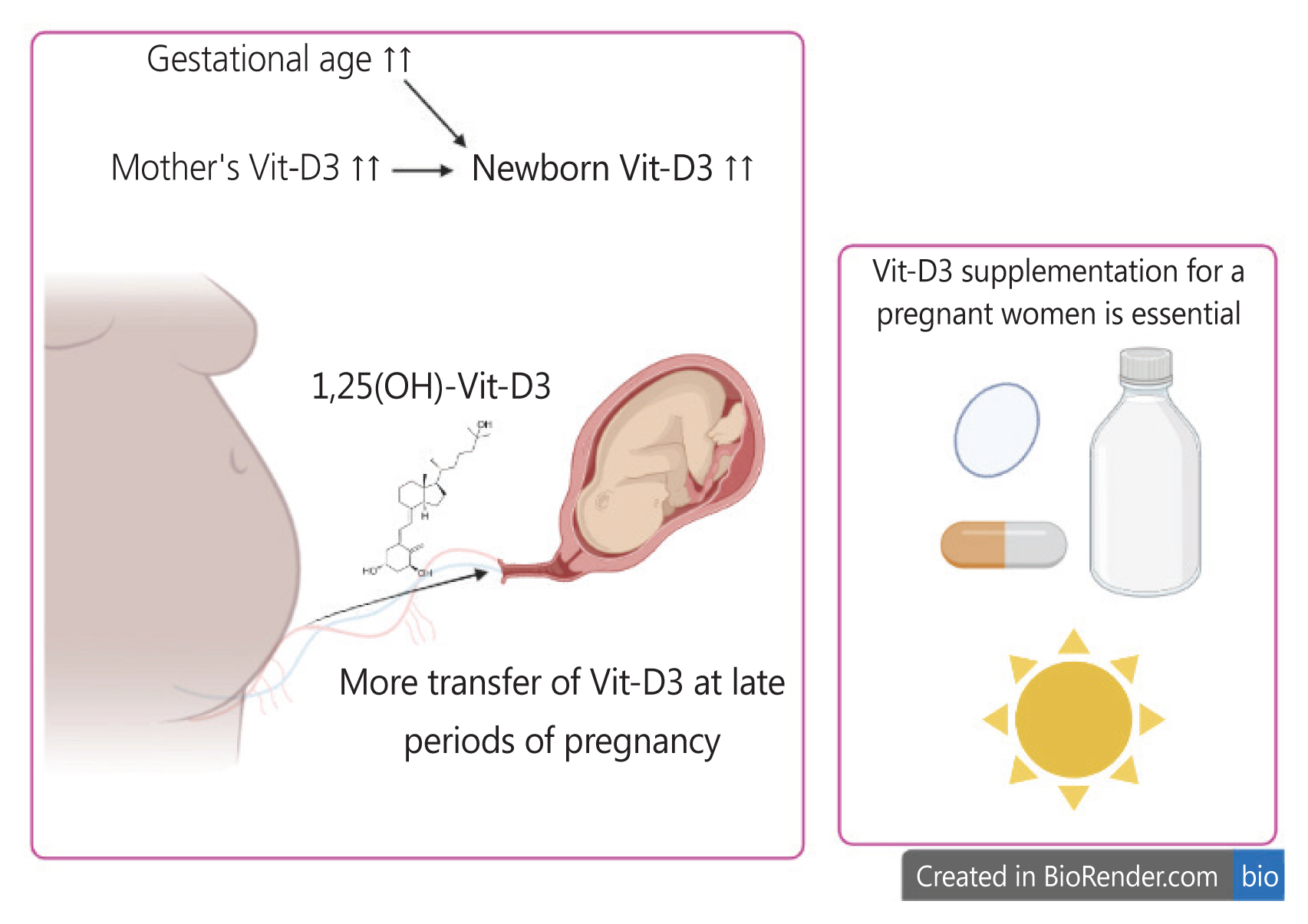
The mean±SD of mothers’ age and gestational age were 29.65±6.18 years and 35.59±1.6 weeks, respectively. Neonatal Vit-D3 levels were associated with maternal age. Using a 30 ng/mL cutoff point for serum Vit-D3 levels, 83.5% of pregnant women and 84.7% of newborns had hypovitaminosis D3. The average Vit-D3 levels of mothers and newborns at delivery time were 23.5±8.07 ng/mL and 20.76±9.14 ng/mL, respectively. Newborn Vit-D3 levels were positively correlated with maternal Vit-D3 serum levels (R=0.744; P<0.001) and gestational age (R=0.161; P=0.022). In newborns, head circumference was inversely correlated with bilirubin level (R=-0.302; P<0.001) but directly associated with weight (R=0.640; P<0.001).
Conclusion
Hypovitaminosis D3 remains a significant challenge for pregnant Iranian women. Maternal Vit-D3 levels provide for the newborn’s needs, particularly in the late stages of pregnancy. Therefore, Vit-D3 supplementation and regular monitoring are essential for pregnant women and their newborns.
Keyword
Figure
Reference
-
References
1. Preuss HG, Kaats GR, Mrvichin N, Bagchi D, Scheckenbach R. Correlating circulating vitamin D3 with aspects of the metabolic syndrome and nonalcoholic fatty liver disease in healthy female volunteers. J Am Coll Nutr. 2020; 39:585–90.2. Guo Y, Xu Y, Zhang T, Wang Y, Liu R, Chang M, et al. Medium and long-chain structured triacylglycerol enhances vitamin D bioavailability in an emulsion-based delivery system: combination of in vitro and in vivo studies. Food Funct. 2022; 13:1762–73.3. Gowtham T, Venkatesh S, Palanisamy S, Rathod S. Impact of maternal hypovitaminosis D on birth and neonatal outcome - a prospective cohort study. J Matern Fetal Neonatal Med. 2022; 35:9940–7.4. Muyayalo KP, Song S, Zhai H, Liu H, Huang DH, Zhou H, et al. Low vitamin D levels in follicular fluid, but not in serum, are associated with adverse outcomes in assisted reproduction. Arch Gynecol Obstet. 2022; 305:505–17.5. Pardabaevna IG, Sa’dullo qizi SN. Vitamin D and pregnancy. J Adv Res Stab. 2022; 2:93–5.6. Stenhouse C, Suva LJ, Gaddy D, Wu G, Bazer FW. Phosphate, calcium, and vitamin D: key regulators of fetal and placental development in mammals. Adv Exp Med Biol. 2022; 1354:77–107.7. Asiabanha M, Younesi B, Absalan A, Lashgari P. Status of serum level of vitamin D3 and its correlation with serum calcium level in patients referred to sarem hospital in tehrantal in tehran. Sarem J Rep Med. 2020; 5:172–9.8. Amiri M, Rostami M, Bidhendi-Yarandi R, Fallahzadeh A, Simbar M, Ramezani Tehrani F. Relationship between vitamin D status in the first trimester of the pregnancy and gestational weight gain: a mediation analysis. Arch Gynecol Obstet. 2020; 305:495–504.9. Rahnemaei FA, Gholamrezaei A, Afrakhteh M, Zayeri F, Vafa MR, Rashidi A, et al. Vitamin D supplementation for primary dysmenorrhea: a double-blind, randomized, placebo-controlled trial. Obstet Gynecol Sci. 2021; 64:353–63.10. Palacios C, Kostiuk LK, Peña-Rosas JP. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst Rev. 2019; 7:CD008873.11. Abd Aziz NH, Yazid NA, Abd Rahman R, Abd Rashid N, Wong SK, Mohamad NV, et al. Is first trimester maternal 25-hydroxyvitamin D level related to adverse maternal and neonatal pregnancy outcomes? A prospective cohort study among Malaysian women. Int J Environ Res Public Health. 2020; 17:3291.12. Olmos-Ortiz A, Avila E, Durand-Carbajal M, Díaz L. Regulation of calcitriol biosynthesis and activity: focus on gestational vitamin D deficiency and adverse pregnancy outcomes. Nutrients. 2015; 7:443–80.13. Amouzegar A, Azizi F, Ashrafivand S, Ahi Z, Saleh M, Mohaghegh S, et al. Prevalence of calcium and vitamin D deficiency and their association with feto-maternal outcomes in a sample of Iranian pregnant women. Hum Antibodies. 2020; 28:305–12.14. Bhat JA, Sheikh SA, Ara R. Correlation of 25-hydroxy vitamin D level with neonatal hyperbilirubinemia in term healthy newborn: a prospective hospital-based observation study. Int J Pediatr Adolesc Med. 2021; 8:5–9.15. Mehrpisheh S, Memarian A, Mahyar A, Valiahdi NS. Correlation between serum vitamin D level and neonatal indirect hyperbilirubinemia. BMC Pediatr. 2018; 18:178.16. Aydeniz EG, Sari U, Tekin I, Dilek TUK. The relationship between first trimester 25-hydroxyvitamin D3 levels and second trimester femur length and their effects on birth weight and length at birth: a preliminary study. Obstet Gynecol Int. 2019; 2019:3846485.17. Hajizadeh S, Rankin Shary J, Gayle Reed S, Lynn Wagner C. The prevalence of hypovitaminosis D and its risk factors in pregnant women and their newborns in the Middle East: a systematic review. Int J Reprod Biomed. 2019; 17:685–708.18. Hajhashemi M, Khorsandi A, Haghollahi F. Comparison of sun exposure versus vitamin D supplementation for pregnant women with vitamin D deficiency. J Matern Fetal Neonatal Med. 2019; 32:1347–52.19. Restriction FG. ACOG practice bulletin, number 227. Obstet Gynecol. 2021; 137:e16–28.20. Abdi F, Amjadi MA, Zaheri F, Rahnemaei FA. Role of vitamin D and calcium in the relief of primary dysmenorrhea: a systematic review. Obstet Gynecol Sci. 2021; 64:13–26.21. Apgar V. A proposal for a new method of evaluation of the newborn infant. Anesth Analg. 2015; 120:1056–9.22. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011; 96:1911–30.23. Azami M, Shamloo M, Nasirkandy M, Veisani Y, Rahmati S, YektaKooshali M, et al. Prevalence of vitamin D deficiency among pregnant women in Iran: a systematic review and meta-analysis. Koomesh. 2017; 19:Pe505–14.24. Hosseinzadeh Z, Kazemian M, Mashak B, Torkmandi H, Badfar G. Vitamin D status in pregnant women and their newborns in Karaj: a cross-sectional study in Iran. Int J Pediatr. 2018; 6:7117–27.25. Qahwaji DM. Association of age and serum vitamin D levels in men with metabolic syndrome. J Coll Physicians Surg Pak. 2022; 32:298–302.26. Zia Z, Hashemi Z, Moghtaderi M, Honar N, Saki F. The effect of maternal vitamin D deficiency on increased risk for hyperbilirubinemia in term newborns. Int J Pediatr. 2020; 8:11141–7.27. Wang H, Xiao Y, Zhang L, Gao Q. Maternal early pregnancy vitamin D status in relation to low birth weight and small-for-gestational-age offspring. J Steroid Biochem Mol Biol. 2018; 175:146–50.28. Noamam KH, Abdulla TN. Relationship of low maternal vitamin D3 level and adverse early neonatal outcomes. Indian J Forensic Med Toxicol. 2021; 15:1197–204.29. Boskabadi H, Zakerihamidi M, Faramarzi R. The vitamin D level in umbilical cord blood in premature infants with or without intra-ventricular hemorrhage: a cross-sectional study. Int J Reprod Biomed. 2018; 16:429–34.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Insulin-like Growth Factor-I and 1,25-(OH)2 Vitamin D3 Concentration on Intrauterine Growth of Newborns from Mothers with Preeclampsia
- Vitamin D in Full-term Neonates in Daegu and Gyeongbuk Province of Korea and the Association with Maternal and Neonatal Diseases
- Low Serum Vitamin D Is Associated with Anti-Thyroid Peroxidase Antibody in Autoimmune Thyroiditis
- Relationship of vitamin D status and obesity index in Korean women
- Vitamin D serum levels and risk of asthma in children