Korean J Sports Med.
2023 Sep;41(3):138-146. 10.5763/kjsm.2023.41.3.138.
Evaluation of Isometric Shoulder Muscle Contraction during Awakening after Arthroscopic Rotator Cuff Repair
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul Red Cross Hospital, Seoul, Korea
- 2Department of Orthopaedic Surgery, H Plus Yangji Hospital, Seoul, Korea
- 3Department of Orthopaedic Surgery, Ajou University School of Medicine, Suwon, Korea
- 4Department of Orthopaedic Surgery, Konkuk University School of M edicine, Seoul, Korea
- 5Department of Orthopaedic Surgery, Sarang Plus Hospital, Seoul, Korea
- KMID: 2545828
- DOI: http://doi.org/10.5763/kjsm.2023.41.3.138
Abstract
- Purpose
Most rotator cuff repairs are performed under general anesthesia, and the shoulder muscles undergo exertion during the patient’s awakening. These may lead to subsequent retear. The purpose of this study is to evaluate the characteristics of shoulder muscle contraction during awakening from general anesthesia after rotator cuff repair.
Methods
Twenty patients underwent arthroscopic rotator cuff repair. Surface electromyography was used to investigate the amplitude of shoulder (upper trapezius [UT] and biceps brachii [BB]) and body (rectus femoris, RF) muscles during awakening in the operating room and resting in the postanesthesia care unit (PACU).
Results
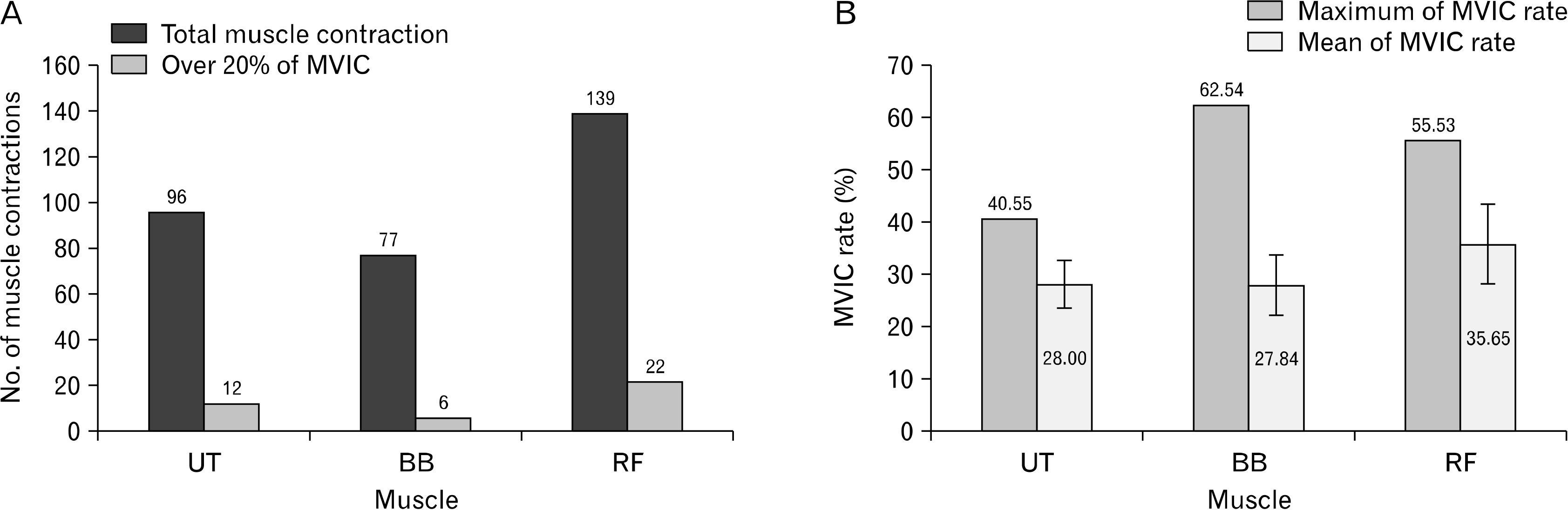
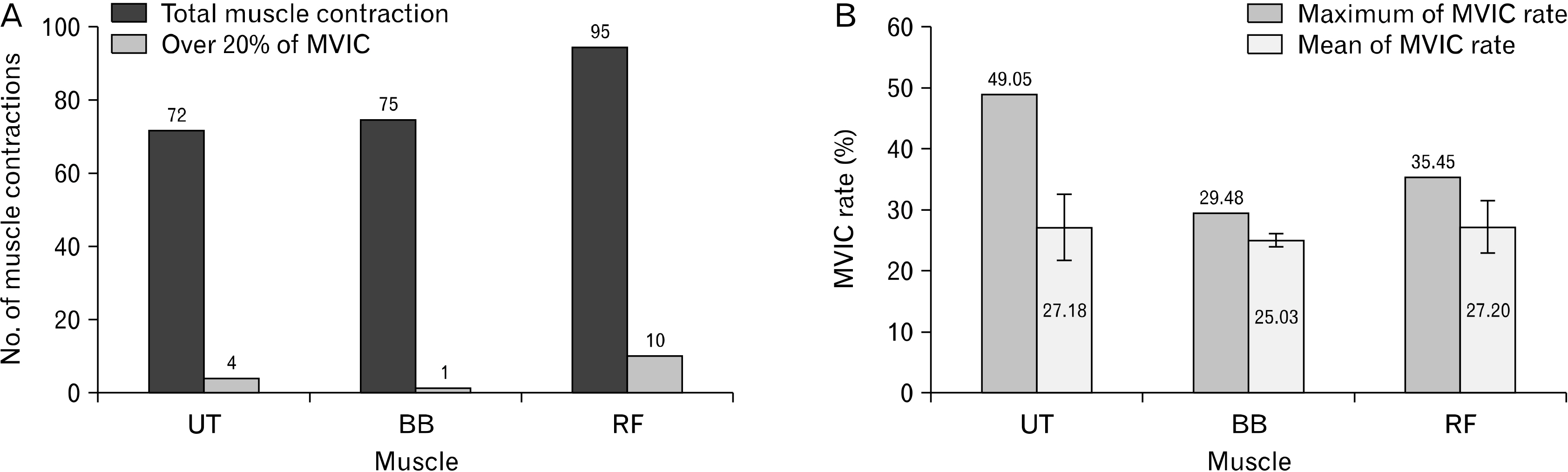
The mean maximum voluntary isometric contraction (MVIC) of the UT, BB, and RF during awakening were 28.00%, 27.84%, and 35.65%, and the mean durations of activation were 3.98, 2.50, and 2.71 seconds. In the PACU, the mean MVIC of the UT, BB, and RF were 27.18%, 25.03%, and 27.20%, and the mean durations were 2.72, 0.26, and 0.67 seconds. No correlation between muscle contraction and postoperative pain was identified.
Conclusion
Less than 10% of the involuntary muscle contractions of the UT and BB measured in this study exceeded 20% of the MVIC and the contractions lasted less than 4 seconds. As the percentage of the MVIC of the rotator cuff is typically lower than that of the UT and BB, strong contractions of the rotator cuff muscle with detrimental effects occur at a low frequency and short duration. Therefore, retear due to muscle contraction during awakening is unlikely.
Figure
Reference
-
1. Harryman DT, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA. 1991; Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 73:982–9. DOI: 10.2106/00004623-199173070-00004. PMID: 1874784.
Article2. Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. 2004; The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 86:219–24. DOI: 10.2106/00004623-200402000-00002. PMID: 14960664.
Article3. Nikolaidou O, Migkou S, Karampalis C. 2017; Rehabilitation after rotator cuff repair. Open Orthop J. 11:154–62. DOI: 10.2174/1874325001711010154. PMID: 28400883. PMCID: PMC5366376.
Article4. Barth J, Andrieu K, Fotiadis E, Hannink G, Barthelemy R, Saffarini M. 2017; Critical period and risk factors for retear following arthroscopic repair of the rotator cuff. Knee Surg Sports Traumatol Arthrosc. 25:2196–204. DOI: 10.1007/s00167-016-4276-x. PMID: 27522591.
Article5. Iannotti JP, Deutsch A, Green A, et al. 2013; Time to failure after rotator cuff repair: a prospective imaging study. J Bone Joint Surg Am. 95:965–71. DOI: 10.2106/JBJS.L.00708. PMID: 23780533.6. Miller BS, Downie BK, Kohen RB, et al. 2011; When do rotator cuff repairs fail? Serial ultrasound examination after arthroscopic repair of large and massive rotator cuff tears. Am J Sports Med. 39:2064–70. DOI: 10.1177/0363546511413372. PMID: 21737833.
Article7. Wei B, Feng Y, Chen W, Ren D, Xiao D, Chen B. 2021; Risk factors for emergence agitation in adults after general anesthesia: a systematic review and meta-analysis. Acta Anaesthesiol Scand. 65:719–29. DOI: 10.1111/aas.13774. PMID: 33370461.
Article8. Kanaya A. 2016; Emergence agitation in children: risk factors, prevention, and treatment. J Anesth. 30:261–7. DOI: 10.1007/s00540-015-2098-5. PMID: 26601849.
Article9. Hollman F, Wolterbeek N, Zijl JA, van Egeraat SP, Wessel RN. 2017; Abduction brace versus antirotation sling after arthroscopic cuff repair: the effects on pain and function. Arthroscopy. 33:1618–26. DOI: 10.1016/j.arthro.2017.02.010. PMID: 28427872.10. Park JH, Chung SW, Lee SJ, Lee JW, Oh KS. 2020; Evaluation of the electromyographic amplitude-to-work ratio in the infraspinatus muscle during external shoulder rotation exercises: a comparison of concentric isotonic and isokinetic exercises. Orthop J Sports Med. 8:2325967120932459. DOI: 10.1177/2325967120932459. PMID: 32685567. PMCID: PMC7343369.
Article11. Solomonow M, Baten C, Smit J, et al. 1990; Electromyogram power spectra frequencies associated with motor unit recruitment strategies. J Appl Physiol (1985). 68:1177–85. DOI: 10.1152/jappl.1990.68.3.1177. PMID: 2341343.
Article12. McCann PD, Wootten ME, Kadaba MP, Bigliani LU. 1993; A kinematic and electromyographic study of shoulder rehabilitation exercises. Clin Orthop Relat Res. 179–88. DOI: 10.1097/00003086-199303000-00023.
Article13. Uhl TL, Muir TA, Lawson L. 2010; Electromyographical assessment of passive, active assistive, and active shoulder rehabilitation exercises. PM R. 2:132–41. DOI: 10.1016/j.pmrj.2010.01.002. PMID: 20193940.
Article14. Cools AM, Tongel AV, Berckmans K, et al. 2020; Electromyographic analysis of selected shoulder muscles during a series of exercises commonly used in patients with symptomatic degenerative rotator cuff tears. J Shoulder Elbow Surg. 29:e361–73. DOI: 10.1016/j.jse.2020.03.019. PMID: 32951644.
Article15. Edwards PK, Ebert JR, Littlewood C, Ackland T, Wang A. 2017; A systematic review of electromyography studies in normal shoulders to inform postoperative rehabilitation following rotator cuff repair. J Orthop Sports Phys Ther. 47:931–44. DOI: 10.2519/jospt.2017.7271. PMID: 28704624.
Article16. Long JL, Ruberte Thiele RA, Skendzel JG, et al. 2010; Activation of the shoulder musculature during pendulum exercises and light activities. J Orthop Sports Phys Ther. 40:230–7. DOI: 10.2519/jospt.2010.3095. PMID: 20200451.
Article17. Park JY, Bang JY, Oh KS. 2016; Blind suprascapular and axillary nerve block for post-operative pain in arthroscopic rotator cuff surgery. Knee Surg Sports Traumatol Arthrosc. 24:3877–83. DOI: 10.1007/s00167-015-3902-3. PMID: 26733274.
Article18. Kendall FP ME, Provance PG, Rodgers MM, Romani WA. Muscles: Testing and Function With Posture and Pain Lippincott. Williams & Wilkins;2005. 5th ed.19. Cross JA, deVries J, Mocarski M, et al. 2020; Electromyography of the shoulder musculature during passive rehabilitation exercises. J Shoulder Elbow Surg. 4:doi:10.1177/2471549220960044. DOI: 10.1177/2471549220960044.
Article20. Kim JH, Koh HJ, Kim DK, et al. 2018; Interscalene brachial plexus bolus block versus patient-controlled interscalene indwelling catheter analgesia for the first 48 hours after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 27:1243–50. DOI: 10.1016/j.jse.2018.02.048. PMID: 29605659.
Article21. Sethi PM, Brameier DT, Mandava NK, Miller SR. 2019; Liposomal bupivacaine reduces opiate consumption after rotator cuff repair in a randomized controlled trial. J Shoulder Elbow Surg. 28:819–27. DOI: 10.1016/j.jse.2019.01.008. PMID: 30928396.
Article22. Uquillas CA, Capogna BM, Rossy WH, Mahure SA, Rokito AS. 2016; Postoperative pain control after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 25:1204–13. DOI: 10.1016/j.jse.2016.01.026. PMID: 27079219.
Article23. Burns KA, Robbins LM, LeMarr AR, Childress AL, Morton DJ, Wilson ML. 2021; Healing rates after rotator cuff repair for patients taking either celecoxib or placebo: a double-blind randomized controlled trial. JSES Int. 5:247–53. DOI: 10.1016/j.jseint.2020.10.011. PMID: 33681844. PMCID: PMC7910746.
Article24. Lee SJ, Sung TY. 2020; Emergence agitation: current knowledge and unresolved questions. Korean J Anesthesiol. 73:471–85. DOI: 10.4097/kja.20097. PMID: 32209961. PMCID: PMC7714637.
Article25. Postaci A, Tiryaki C, Sacan O, Ornek D, Kalyoncu M, Dikmen B. 2013; Rocuronium-sugammadex decreases the severity of post-electroconvulsive therapy agitation. J ECT. 29:e2–3. DOI: 10.1097/YCT.0b013e31825de0de. PMID: 23422529.
Article26. Lee SJ, Sung TY, Cho CK. 2019; Comparison of emergence agitation between succinylcholine and rocuronium-sugammadex in adults following closed reduction of a nasal bone fracture: a prospective randomized controlled trial. BMC Anesthesiol. 19:228. DOI: 10.1186/s12871-019-0907-3. PMID: 31842841. PMCID: PMC6916043.
Article27. Cho HR, Kim HK, Baek SH, Jung KY. 2008; The effect of remifentanil infusion on coughing during emergence from general anesthesia with desflurane. Korean J Anesthesiol. 55:670–4. DOI: 10.4097/kjae.2008.55.6.670.
Article28. Kim YS, Lee HJ, Jeon SB. 2015; Management of pain and agitation for patients in the intensive care unit. J Neurocrit Care. 8:53–65. DOI: 10.18700/jnc.2015.8.2.53.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Various Regimens for the Functional Recovery after Arthroscopic Shoulder Surgery
- Arthroscopic Partial Repair of Massive Contracted Rotator Cuff Tears
- Revisional Rotator Cuff Repair
- New Retear Pattern after Rotator Cuff Repair at Previous Intact Portion of Rotator Cuff
- MRI Follow-up Study After Arthroscopic Repair of Multiple Rotator Cuff Tendons