J Korean Med Sci.
2023 Aug;38(33):e259. 10.3346/jkms.2023.38.e259.
Needs Assessment for the Development of Training Curricula for Internal Medicine Residents
- Affiliations
-
- 1Department of Medical Education, Gachon University College of Medicine, Incheon, Korea
- 2Department of Medical Education, CHA University School of Medicine, Pocheon, Korea
- 3Department of Medical Education, Wonkwang University College of Medicine, Iksan, Korea
- 4Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Medical Education, Chungnam National University College of Medicine, Daejeon, Korea
- 6Department of Psychiatry, Chungnam National University College of Medicine, Daejeon, Korea
- 7Department of Internal Medicine, Inje University College of Medicine, Busan, Korea
- KMID: 2545211
- DOI: http://doi.org/10.3346/jkms.2023.38.e259
Abstract
- Background
Patient-centered outcomes can be achieved when common core and specialist competencies are achieved in a balanced manner. This study was conducted to assess the need to fill the gap between the defined competencies and learners’ achievement, in order to improve the internal medicine (IM) training education curriculum for promoting patientcentered outcomes.
Methods
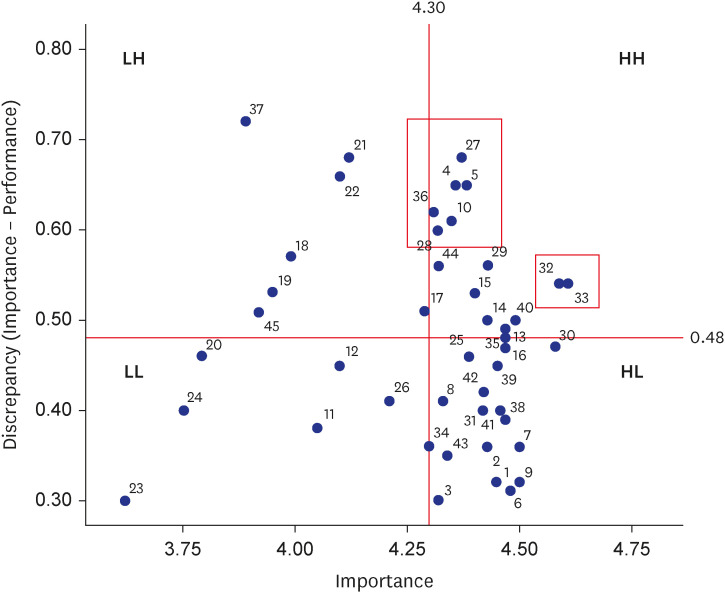
A cross-sectional online survey was conducted. The participants were 202 IM specialists who obtained board certification in 2020−2021. We developed a questionnaire to investigate the self-evaluation of common core competencies and achievement level of IM essential competencies. For analysis, frequency tests, paired t-test, Borich priority formula, and χ 2 were performed.
Results
In common core competencies, IM specialists recognized that their achievement levels in all competency categories were lower than their importance level (P < 0.001), and the highest educational demands were related to self-management. They assessed their five essential procedure skill levels as novice or advanced beginner status. The achievement level for the essential symptoms and signs that IM specialists should be able to manage was predominantly competent level. However, on average, 34.9% answered that they had never assessed during training for essential skills, and 29.7% answered the same for essential symptoms and signs.
Conclusion
We identified the priorities of core competencies, the level of achievement in essential procedures and patient care with essential symptoms and signs for IM training, and the related educational methods and assessment status. This study is expected to be used as basic data for developing and revising IM training educational curriculum.
Keyword
Figure
Reference
-
1. Wang KC. Reformation of post-graduate medical education system in Korea. J Korean Med Assoc. 2011; 54(4):352–354.2. O YH. A study on the number of residents in each training hospital. J Korean Hosp Assoc. 2004; 33(5):78–85.3. Jung HY. Not change, but innovation in training system of internal medicine. Korean J Med. 2016; 91(2):93–105.4. Kim JJ. Residency training: training program renewal and evaluation of training. J Korean Med Assoc. 2014; 57(11):896–898.5. Oh SH, Kim JS. Training dropout intention and related factors of residents. J Digit Converg. 2021; 19(8):257–264.6. Korean Law Information Center. Act on the improvement of training conditions and status of medical residents. Updated 2020. Accessed October 17, 2022. https://www.law.go.kr/LSW/eng/engLsSc.do?menuId=2§ion=lawNm&query=resident+training&x=26&y=44#liBgcolor0 .7. Accreditation Council for Graduate Medical Education. Accreditation council for graduate medical education. Updated 2021. Accessed October 17, 2022. http://acgme.org/About-Us/Overview .8. Frank JR, Snell L, Sherbino J, Can ME. 2015 Physician competency framework. Updated 2015. Accessed October 19, 2022. http://www.royalcollege.ca/rcsite/documents/CanMEDS/CanMEDS-full-framework-e.pdf .9. Ahn DS. Korean doctor’s role. J Korean Med Assoc. 2014; 57(1):3–7.10. Jeon WT, Jung HN, Kim YJ, Kim CW, Yune SJ, Lee GH, et al. Patient-centered doctor’s competency framework in Korea. Korean Med Educ Rev. 2022; 24(2):79–92.11. Meng KH. History of the medical education accreditation system in Korea: implementation and activities in the early stages. J Educ Eval Health Prof. 2020; 17:29. PMID: 33085996.12. The Korean Association of Internal Medicine. A Core Competency Guidebook for Internal Medicine Residency Training. Seoul, Korea: The Korean Association of Internal Medicine;2017.13. Korean Academy of Medical Science. A Study on the Improvement of Resident Training Program According to the Specialties. Seoul, Korea: Korean Academy of Medical Sciences;2013.14. Green ML, Aagaard EM, Caverzagie KJ, Chick DA, Holmboe E, Kane G, et al. Charting the road to competence: developmental milestones for internal medicine residency training. J Grad Med Educ. 2009; 1(1):5–20. PMID: 21975701.15. Weinberger SE, Pereira AG, Iobst WF, Mechaber AJ, Bronze MS. Alliance for Academic Internal Medicine Education Redesign Task Force II. Competency-based education and training in internal medicine. Ann Intern Med. 2010; 153(11):751–756. PMID: 21135298.16. Kim YM, Choi MH, Lee JH, Lim YJ, Kim YJ, Park JS, et al. Development of entrustable professional activity, core competencies, and guidelines in 2021 radiology competency education project. J Korean Soc Radiol. 2022; 83(2):284–292.17. Lee MS, Ahn DS, Kim MG, Kim YR, Bea JY. Development of Generic Curriculum for Graduate Medical Education. Seoul, Korea: KMA Research Institute for Healthcare Policy;2021.18. Lee SW. Concept and development of resident training program for general competencies. Korean Med Educ Rev. 2017; 19(2):63–69.19. Accreditation Council for Graduate Medical Education (ACGME). Milestones guidebook for residents and fellows. Updated 2020. Accessed October 19, 2022. https://www.acgme.org/globalassets/pdfs/milestones/milestonesguidebookforresidentsfellows.pdf .20. General Medical Council. Good medical practice. Updated 2013. Accessed October 19, 2022. https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice .21. Ahn MS, Lee SW, Lee HJ. National Support Plan for General Competency Education for Medical Residents. Seoul, Korea: KMA Research Institute for Healthcare Policy;2021.22. The Korean Association of Internal Medicine. Updated 2021. Accessed October 19, 2022. https://kaim.or.kr/major/?sn=1&sn2=2 .23. General Medical Council. Good medical practice. Internal medicine-stage one. Updated 2019. Accessed October 19, 2022. https://www.gmc-uk.org/-/media/documents/im-stage-one-curriculum-2019-final-v1_1_pdf-91785394.pdf .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Geriatrics in Family Medicine Residency Program: Training Conditions and Suggestions
- Endoscopic Sedation: From Training to Performance
- Implementing Competency-Based Medical Education in Internal Medicine Residency Training Program: the Process and Impact on Residents' Satisfaction
- A Recognition Survey by Psychiatry Residents and Psychiatrists Regarding the Quality of Residency Training and Clinical Competence in Korea
- Evaluation of the Educational Status of Internal Medicine Residency Program in Korea