Ewha Med J.
2023 Jul;46(3):e6. 10.12771/emj.2023.e6.
Prognostic Significance of 24-Hour Ambulatory Blood Pressure and Holter Monitoring in Patients without Atrial Fibrillation
- Affiliations
-
- 1Ewha Womans University College of Medicine, Seoul, Korea
- 2Department of Cardiology, Ewha Womans University College of Medicine, Seoul, Korea
- KMID: 2545171
- DOI: http://doi.org/10.12771/emj.2023.e6
Abstract
Objectives
This study investigated the 24-hour ambulatory blood pressure monitoring (ABPM) and Holter parameters for evaluating their prognostic significance of cardiovascular events including stroke in population without atrial fibrillation (AF).
Methods
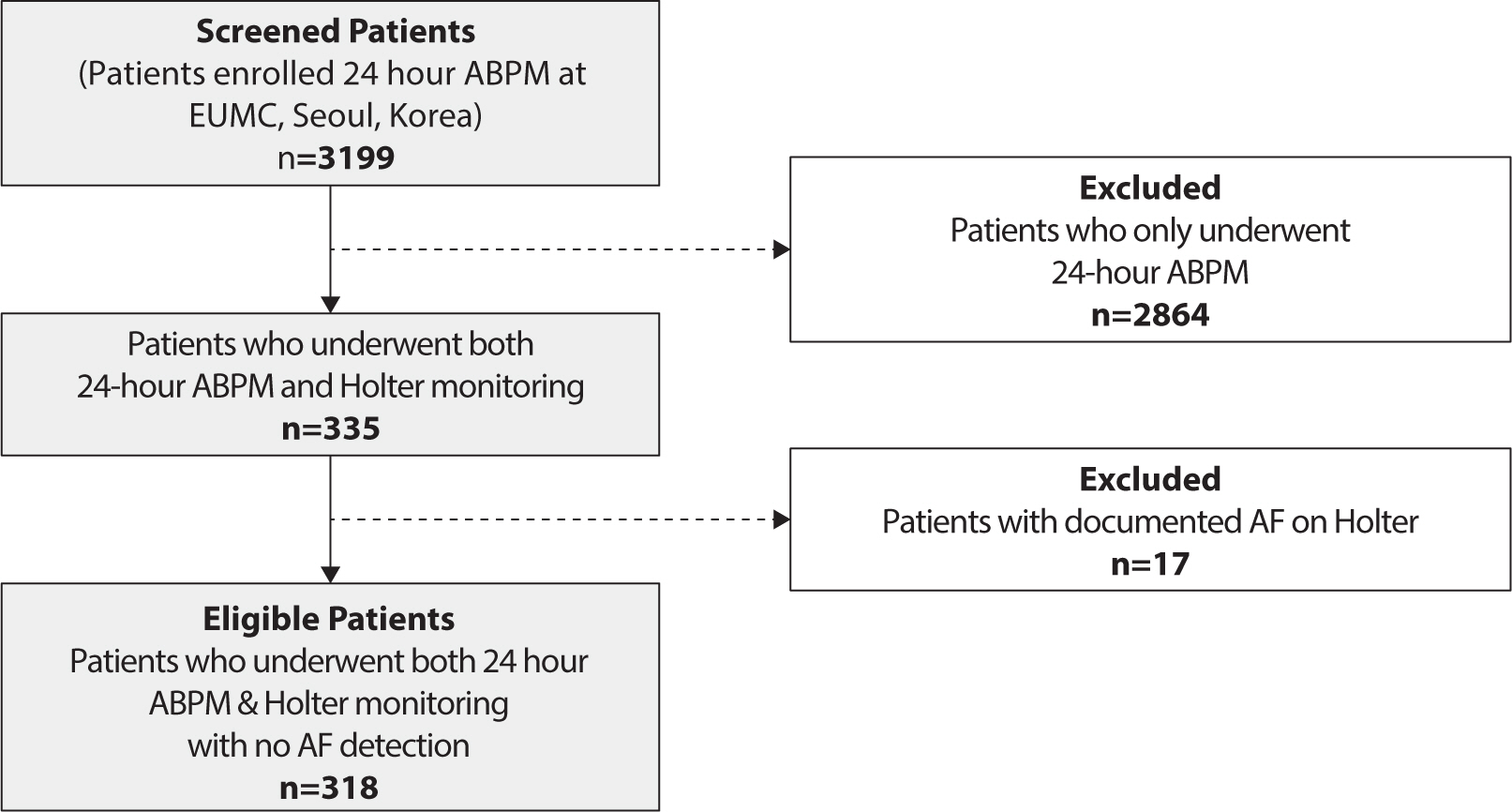
Among 3,199 patients that underwent ABPM, 335 who also underwent Holter recordings were selected in a tertiary hospital. Seventeen patients who had been documented with AF on Holter monitoring or diagnosed with AF were excluded, and finally 318 patients were analyzed. The association between cardiovascular events and ABPM/Holter parameters was analyzed by a logistic regression model, and the risk factors were estimated by a Cox hazard model. Age, sex, and histories of cardiovascular disease were adjusted by a multivariable analysis, and the cut-off values were suggested by a Kaplan-Meyer analysis.
Results
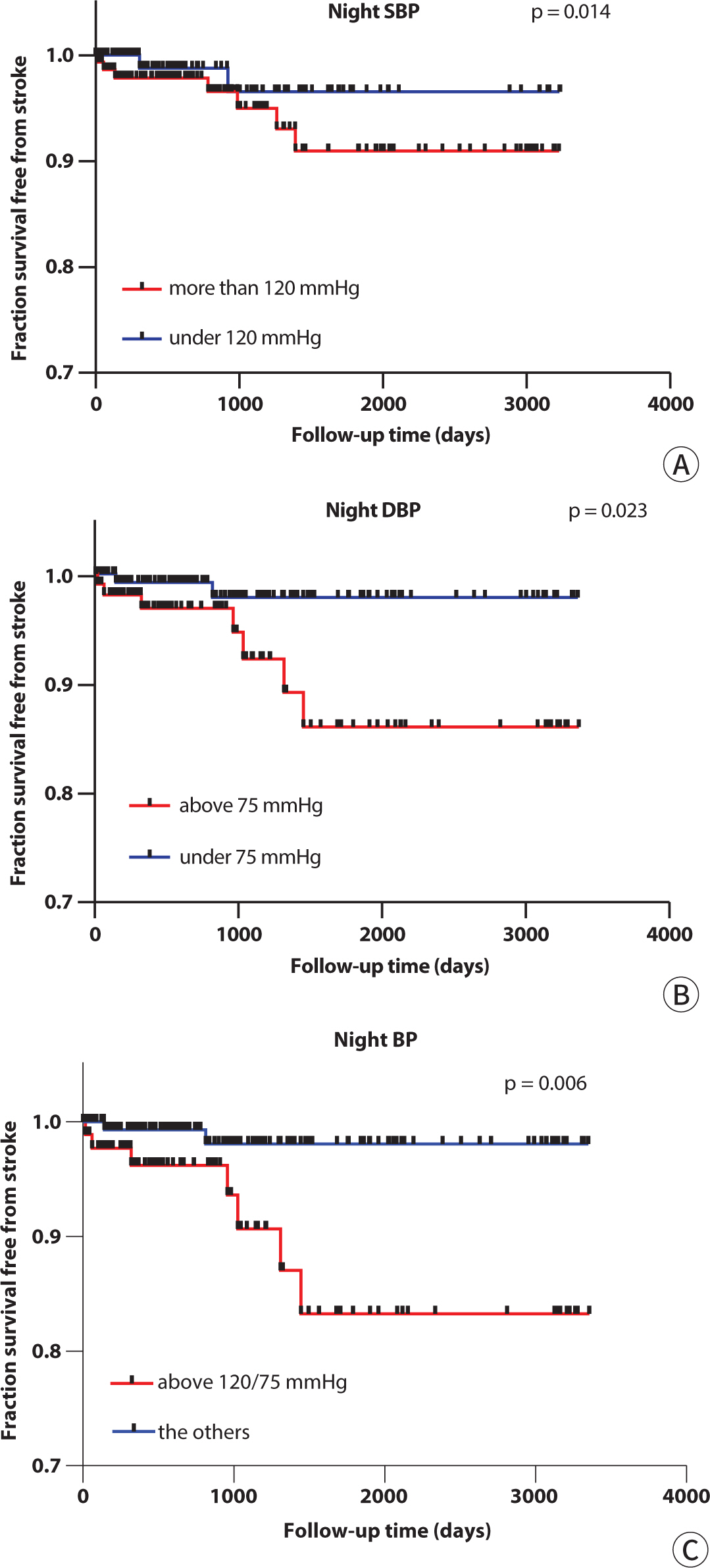
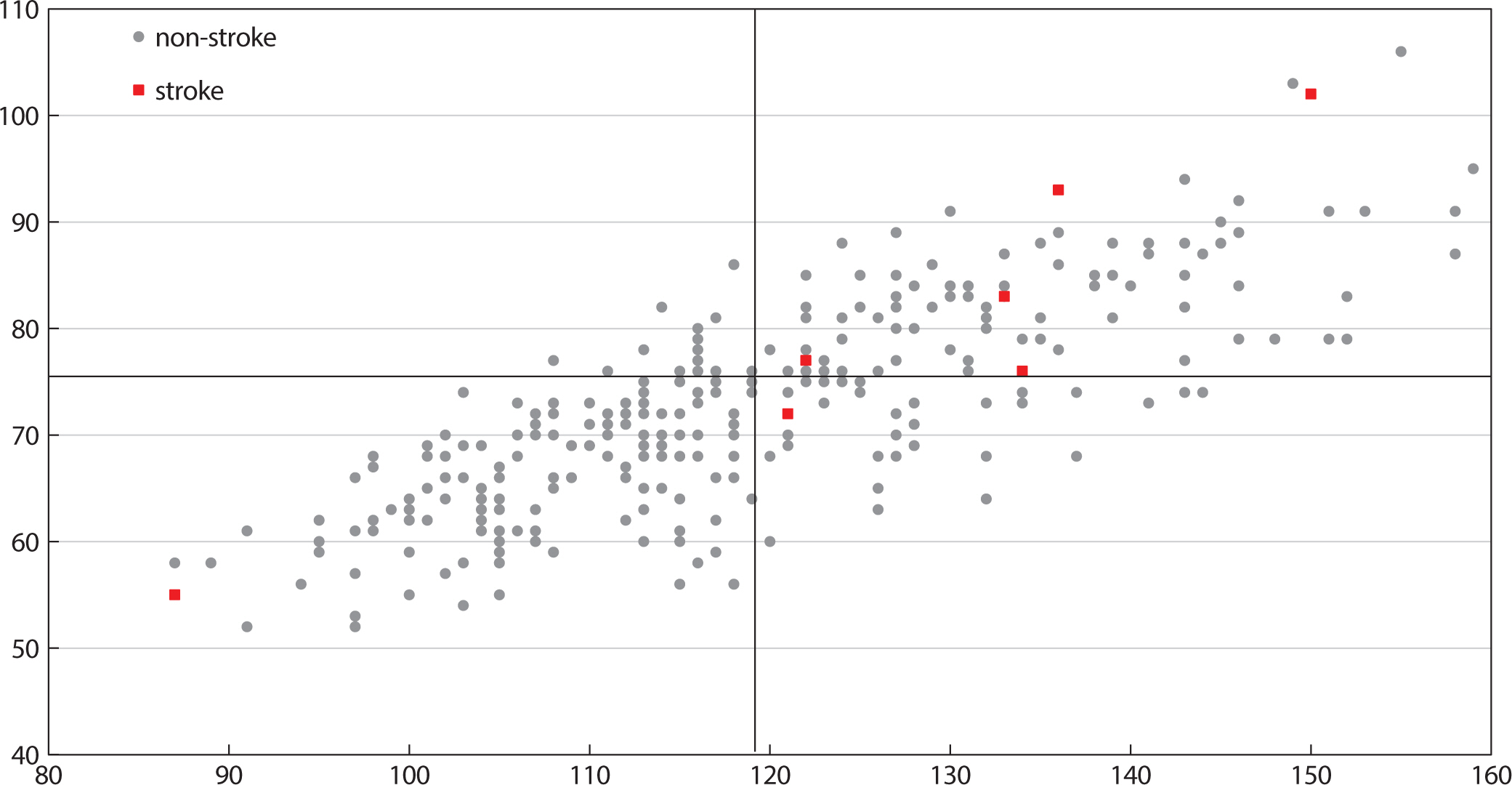
During the total follow-up (28.5±1.7 months), 13 (4.1%) stroke, 6 (1.9%) heart failure, and 12 (3.8%) acute coronary syndrome incidences were observed. In the univariate analysis of the ABPM parameters, an increment in the night systolic BP (hazard ratio=1.034, P=0.020) and night diastolic BP (hazard ratio=1.063, P=0.031) significantly elevated the risk of a stroke occurrence. According to the Kaplan-Meyer analysis, there was a significant difference in the stroke incidence between the groups divided by a cut-off value of the night systolic BP of 120 mmHg (P=0.014) and night diastolic BP of 75 mmHg (P=0.023).
Conclusion
In a population without AF, the nocturnal BP was a significant predictor of a stroke incidence. At this point, the cut-off value of mean 120/75 mmHg in 24 ABPM was advisable.
Figure
Reference
-
References
1. Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N Engl J Med. 2006; 354:2368–2374. DOI: 10.1056/NEJMra060433. PMID: 16738273.
Article2. Eguchi K, Pickering TG, Hoshide S, Ishikawa J, Ishikawa S, Schwartz JE, et al. Ambulatory blood pressure is a better marker than clinic blood pressure in predicting cardiovascular events in patients with/without type 2 diabetes. Am J Hypertens. 2008; 21((4)):443–450. DOI: 10.1038/ajh.2008.4. PMID: 18292756. PMCID: PMC3881175.
Article3. Galli A, Ambrosini F, Lombardi F. Holter monitoring and loop recorders: from research to clinical practice. Arrhythm Electrophysiol Rev. 2016; 5((2)):136–143. DOI: 10.15420/AER.2016.17.2. PMID: 27617093. PMCID: PMC5013174.
Article4. Zimetbaum P, Goldman A. Ambulatory arrhythmia monitoring: choosing the right device. Circulation. 2010; 122((16)):1629–1636. DOI: 10.1161/CIRCULATIONAHA.109.925610. PMID: 20956237.5. Paudel B, Paudel K. The diagnostic significance of the holter monitoring in the evaluation of palpitation. J Clin Diagn Res. 2013; 7((3)):480–483. DOI: 10.7860/JCDR/2013/4923.2802. PMID: 23634400. PMCID: PMC3616560.
Article6. Shaffer F, Ginsberg JP. An overview of heart rate variability metrics and norms. Front Public Health. 2017; 5:258. DOI: 10.3389/fpubh.2017.00258. PMID: 29034226. PMCID: PMC5624990.
Article7. Nelson BW, Allen NB. Accuracy of consumer wearable heart rate measurement during an ecologically valid 24-hour period: intraindividual validation study. JMIR Mhealth Uhealth. 2019; 7(3):e10828. DOI: 10.2196/10828. PMID: 30855232. PMCID: PMC6431828.
Article8. Lewalter T, Boriani G. Relevance of monitoring atrial fibrillation in clinical practice. Arrhythm Electrophysiol Rev. 2012; 1((1)):54–58. DOI: 10.15420/aer.2012.1.54. PMID: 26835031. PMCID: PMC4711515.
Article9. Minutolo R, Gabbai FB, Chiodini P, Garofalo C, Stanzione G, Liberti ME, et al. Reassessment of ambulatory blood pressure improves renal risk stratification in nondialysis chronic kidney disease: long-term cohort study. Hypertension. 2015; 66((3)):557–562. DOI: 10.1161/HYPERTENSIONAHA.115.05820. PMID: 26150434.
Article10. Paoletti E, Bellino D, Amidone M, Rolla D, Cannella G. Relationship between arterial hypertension and renal damage in chronic kidney disease: insights from ABPM. J Nephrol. 2006; 19((6)):778–782.11. Scheppach JB, Raff U, Toncar S, Ritter C, Klink T, Störk S, et al. Blood pressure pattern and target organ damage in patients with chronic kidney disease. Hypertension. 2018; 72((4)):929–936. DOI: 10.1161/HYPERTENSIONAHA.118.11608. PMID: 30354716.
Article12. Cho J. Current status and prospects of health-related sensing technology in wearable devices. J Healthc Eng. 2019; 2019:3924508. DOI: 10.1155/2019/3924508. PMID: 31316740. PMCID: PMC6604299.
Article13. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham study. Stroke. 1991; 22((8)):983–988. DOI: 10.1161/01.STR.22.8.983. PMID: 1866765.
Article14. Kario K, Schwartz JE, Pickering TG. Changes of nocturnal blood pressure dipping status in hypertensives by nighttime dosing of α-adrenergic blocker, doxazosin: results from the HALT study. Hypertension. 2000; 35((3)):787–794. DOI: 10.1161/01.HYP.35.3.787. PMID: 10720596.
Article15. Perloff D, Sokolow M, Cowan RM, Juster RP. Prognostic value of ambulatory blood pressure measurements: further analyses. J Hypertens Suppl Off J Int Soc Hypertens. 1989; 7(3):S3–S10.16. Verdecchia P, Porcellati C, Schillaci G, Borgioni C, Ciucci A, Battistelli M, et al. Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994; 24((6)):793–801. DOI: 10.1161/01.HYP.24.6.793. PMID: 7995639.
Article17. de la Sierra A, Banegas JR, Segura J, Gorostidi M, Ruilope LM. Ambulatory blood pressure monitoring and development of cardiovascular events in high-risk patients included in the Spanish ABPM registry: the CARDIORISC event study. J Hypertens. 2012; 30((4)):713–719. DOI: 10.1097/HJH.0b013e328350bb40. PMID: 22306850.
Article18. Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007; 370((9594)):1219–1229. DOI: 10.1016/S0140-6736(07)61538-4. PMID: 17920917.
Article19. Roush GC, Fagard RH, Salles GF, Pierdomenico SD, Reboldi G, Verdecchia P, et al. Prognostic impact from clinic, daytime, and night-time systolic blood pressure in nine cohorts of 13,844 patients with hypertension. J Hypertens. 2014; 32((12)):2332–2340. DOI: 10.1097/HJH.0000000000000355. PMID: 25333682.
Article20. Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008; 51((1)):55–61. DOI: 10.1161/HYPERTENSIONAHA.107.100727. PMID: 18039980.
Article21. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018; 71((6)):1269–1324. DOI: 10.1161/HYP.0000000000000066. PMID: 29133354.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 24 Hour Holter EKG Findings in Patients with Dilated Cardiomyopathy
- Study of 24 Hour Ambulatory Blood Pressure Monitoring in Acute Stroke Patients
- A representative value for 24-hour monitored ambulatory blood pressure
- The Joint Multicenter Study on the Atrial Fibrillation in Korea
- Predicting Intermittent Atrial Fibrillation in Outpatient Clinics