Brain Tumor Res Treat.
2023 Jul;11(3):204-209. 10.14791/btrt.2023.0023.
Role of Immediate Postoperative Prolactin Measurement in Female Prolactinoma Patients: Predicting Long-Term Remission After Complete Tumor Removal
- Affiliations
-
- 1Department of Neurosurgery, Armed Forces Capital Hospital, Seongnam, Korea
- 2Department of Neurosurgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea
- 4Endocrine Research Institute, Yonsei University College of Medicine, Seoul, Korea
- 5Pituitary Tumor Center, Severance Hospital, Seoul, Korea
- KMID: 2545117
- DOI: http://doi.org/10.14791/btrt.2023.0023
Abstract
- Background
Transsphenoidal surgery is one of the important treatment options in the manage- ment of prolactinomas; however, complete resection of the tumor does not always lead to endocrinological remission. While many studies have investigated preoperative factors associated with surgical outcome, little has been known about the relationship between postoperative factors and long-term surgical outcomes; moreover, there is no consistency in results. The aim of this study was to demonstrate the reliability of immediate postoperative prolactin levels as predictors of long-term outcomes.
Methods
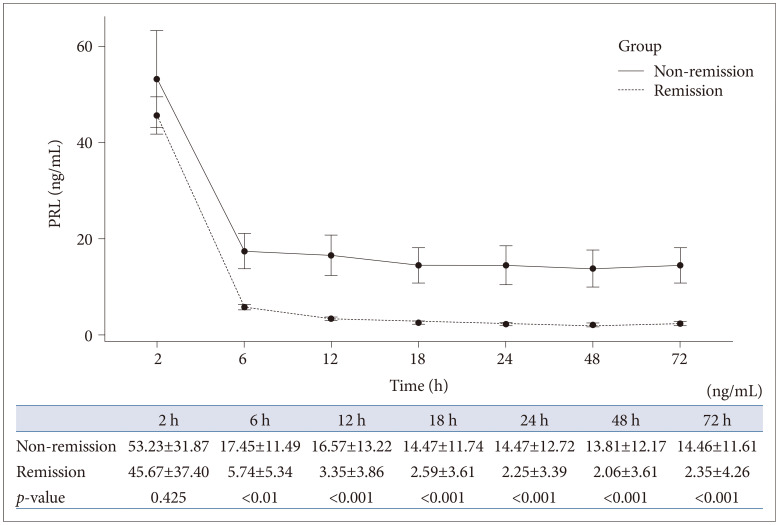
A total of 105 female patients who underwent complete removal of their histologically confirmed prolactinomas were included, and their medical records were retrospectively reviewed. To evaluate the predictability of immediate postoperative prolactin levels for long-term remission, prolactin levels were measured at 2, 6, 12, 18, 24, 48, and 72 h after surgery.
Results
From the 105 included patients, 95 (90.5%) and 10 (9.5%) belonged to the remission and non-remission groups, respectively. A significant difference was observed in the prolactin level measured 6 h after surgery between the remission and non-remission groups, and this difference stayed apparent until 72 h after surgery. We derived a cut-off value for every postoperative time point that showed a significant relationship with disease remission.
Conclusion
Our study suggests that immediate postoperative measurement of prolactin levels is a reliable predictor of long-term remission and can contribute to early identification of patients who require adjuvant treatment after surgery.
Keyword
Figure
Reference
-
1. Krysiak R, Okopień B, Marek B, Szkróbka W. [Prolactinoma]. Przegl Lek. 2009; 66:198–205. Polish. PMID: 19708510.2. Ciccarelli E, Camanni F. Diagnosis and drug therapy of prolactinoma. Drugs. 1996; 51:954–965. PMID: 8736617.3. Schlechte JA. Long-term management of prolactinomas. J Clin Endocrinol Metab. 2007; 92:2861–2865. PMID: 17682084.4. Zamanipoor Najafabadi AH, Zandbergen IM, de Vries F, Broersen LHA, van den Akker-van Marle ME, Pereira AM, et al. Surgery as a viable alternative first-line treatment for prolactinoma patients. A systematic review and meta-analysis. J Clin Endocrinol Metab. 2020; 105:e32–e41. PMID: 31665485.5. Andereggen L, Frey J, Andres RH, El-Koussy M, Beck J, Seiler RW, et al. 10-year follow-up study comparing primary medical vs. surgical therapy in women with prolactinomas. Endocrine. 2017; 55:223–230. PMID: 27688009.6. Huber M, Luedi MM, Schubert GA, Musahl C, Tortora A, Frey J, et al. Machine learning for outcome prediction in first-line surgery of prolactinomas. Front Endocrinol (Lausanne). 2022; 13:810219. PMID: 35250868.7. Park JY, Choi W, Hong AR, Yoon JH, Kim HK, Jang WY, et al. Surgery is a safe, effective first-line treatment modality for noninvasive prolactinomas. Pituitary. 2021; 24:955–963. PMID: 34189717.8. Penn MC, Cardinal T, Zhang Y, Abt B, Bonney PA, Lorenzo P, et al. Cure and hormonal control after prolactinoma resection: case series and systematic review. J Endocr Soc. 2021; 5:bvab074. PMID: 34466765.9. Gillam MP, Molitch ME, Lombardi G, Colao A. Advances in the treatment of prolactinomas. Endocr Rev. 2006; 27:485–534. PMID: 16705142.10. Melmed S, Casanueva FF, Hoffman AR, Kleinberg DL, Montori VM, Schlechte JA, et al. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011; 96:273–288. PMID: 21296991.11. Ku CR, Kim EH, Oh MC, Lee EJ, Kim SH. Surgical and endocrinological outcomes in the treatment of growth hormone-secreting pituitary adenomas according to the shift of surgical paradigm. Neurosurgery. 2012; 71:ons192–ons203. PMID: 22743357.12. Neal JH, Weiss MH. Management of prolactin-secreting pituitary adenomas. West J Med. 1990; 153:546–547. PMID: 2260295.13. Molitch ME. Diagnosis and treatment of pituitary adenomas: a review. JAMA. 2017; 317:516–524. PMID: 28170483.14. Paluzzi A, Fernandez-Miranda JC, Tonya Stefko S, Challinor S, Snyderman CH, Gardner PA. Endoscopic endonasal approach for pituitary adenomas: a series of 555 patients. Pituitary. 2014; 17:307–319. PMID: 23907570.15. Losa M, Mortini P, Barzaghi R, Gioia L, Giovanelli M. Surgical treatment of prolactin-secreting pituitary adenomas: early results and long-term outcome. J Clin Endocrinol Metab. 2002; 87:3180–3186. PMID: 12107221.16. Babey M, Sahli R, Vajtai I, Andres RH, Seiler RW. Pituitary surgery for small prolactinomas as an alternative to treatment with dopamine agonists. Pituitary. 2011; 14:222–230. PMID: 21170594.17. Lee EJ, Ahn JY, Noh T, Kim SH, Kim TS, Kim SH. Tumor tissue identification in the pseudocapsule of pituitary adenoma: should the pseudocapsule be removed for total resection of pituitary adenoma? Neurosurgery. 2009; 64(3 Suppl):ONS62–ONS70. PMID: 19240574.18. Oldfield EH, Vortmeyer AO. Development of a histological pseudocapsule and its use as a surgical capsule in the excision of pituitary tumors. J Neurosurg. 2006; 104:7–19. PMID: 16509142.19. Ceylan S, Cabuk B, Koc K, Anik I, Vural C. Endoscopic distinction between capsule and pseudocapsule of pituitary adenomas. Acta Neurochir (Wien). 2013; 155:1611–1619. PMID: 23686633.20. Qu X, Wang M, Wang G, Han T, Mou C, Han L, et al. Surgical outcomes and prognostic factors of transsphenoidal surgery for prolactinoma in men: a single-center experience with 87 consecutive cases. Eur J Endocrinol. 2011; 164:499–504. PMID: 21252173.21. Alimohamadi M, Sanjari R, Shirani M, Alikhani F, Amirjamshidi A. Initial experience with diffusion-weighted imaging to predict the tumor consistency and surgical success in solid growth hormone producing pituitary macroadenomas. Asian J Neurosurg. 2019; 14:698–701. PMID: 31497087.22. Melmed S. Mechanisms for pituitary tumorigenesis: the plastic pituitary. J Clin Invest. 2003; 112:1603–1618. PMID: 14660734.23. Kim EH, Oh MC, Lee EJ, Kim SH. Predicting long-term remission by measuring immediate postoperative growth hormone levels and oral glucose tolerance test in acromegaly. Neurosurgery. 2012; 70:1106–1113. PMID: 22067418.24. Kim SH, Ku CR, Na M, Yoo J, Kim W, Jung IH, et al. Immediate postoperative measurement of thyroid-stimulating hormone as an early predictor of remission in thyroid-stimulating hormone-secreting pituitary adenomas. J Neurosurg. 2020; 134:794–800. PMID: 32168476.25. Amar AP, Couldwell WT, Chen JC, Weiss MH. Predictive value of serum prolactin levels measured immediately after transsphenoidal surgery. J Neurosurg. 2002; 97:307–314. PMID: 12186458.