Intest Res.
2023 Jul;21(3):385-391. 10.5217/ir.2022.00030.
Submucosal fat accumulation in Crohn’s disease: evaluation with sonography
- Affiliations
-
- 1Department of Radiology Doctor Peset University Hospital, Valencia, Spain
- 2Department of Gastroenterology, Doctor Peset University Hospital, Valencia, Spain
- KMID: 2544761
- DOI: http://doi.org/10.5217/ir.2022.00030
Abstract
- Background/Aims
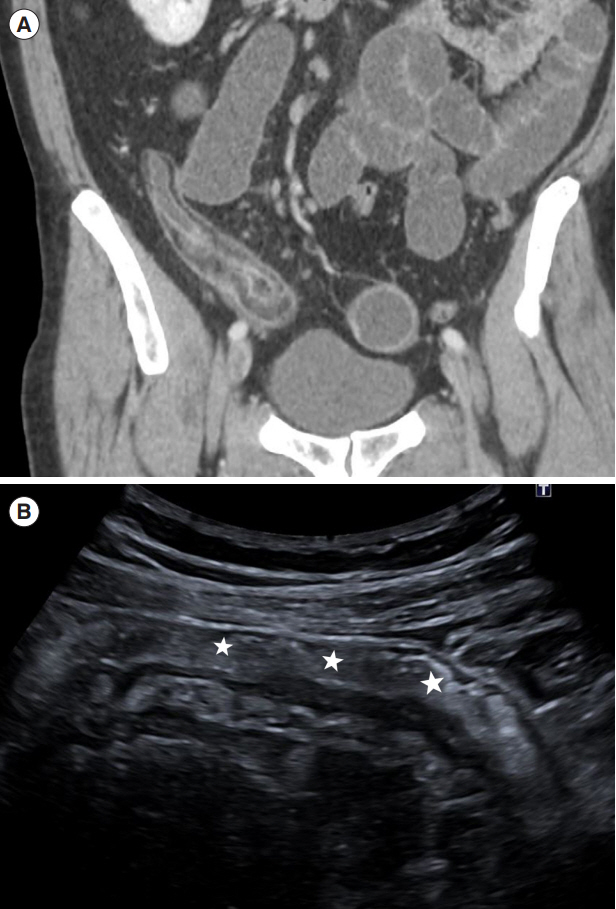
The study objective is to investigate the ultrasound features that allow suspecting the presence of submucosal fat deposition, called the fat halo sign (FHS), in the intestinal wall of patients with Crohn’s disease.
Methods
Computed tomography (CT) examinations over a period of 10 years were reviewed for the presence of the FHS in the bowel wall. A measurement of less than –10 Hounsfield units was regarded as indicative of fat. We included only patients who had undergone ultrasound examinations 3 months before or after CT. The study cohort group comprised 68 patients. Wall and submucosal thickness were measured on longitudinal ultrasound sections. A receiver operating characteristic curve was constructed to determine the best cutoff of ultrasound submucosal wall thickness value for predicting FHS in the bowel wall determined on CT.
Results
The FHS was present in 22 patients (31%) on CT. There were significant differences between submucosal thickness of patients with FHS and patients without FHS (4.19 mm vs. 2.41 mm). From the receiver operating characteristic curve, a threshold value of 3.1 mm of submucosal thickness had the best sensitivity and specificity to suspect FHS (95.5% and 89.1%, respectively; area under the curve, 0.962), with an odds ratio of 172. All of 16 patients with a submucosal thickness >3.9 mm had FHS.
Conclusions
FHS in patients with Crohn’s disease can be suspected on ultrasound in cases with marked thickening of the submucosa layer. In these cases, the activity of the disease should be measured by other parameters such as the color Doppler.
Keyword
Figure
Cited by 1 articles
-
A novel serum biomarker of endoscopic mucosal healing in inflammatory bowel disease
Hyoun Woo Kang
Intest Res. 2024;22(1):3-4. doi: 10.5217/ir.2023.00198.
Reference
-
1. Gomollón F, Dignass A, Annese V, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 1: diagnosis and medical management. J Crohns Colitis. 2017; 11:3–25.
Article2. Maaser C, Sturm A, Vavricka SR, et al. ECCO-ESGAR guideline for diagnostic assessment in IBD Part 1: initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis. 2019; 13:144–164.
Article3. Maconi G, Nylund K, Ripolles T, et al. EFSUMB recommendations and clinical guidelines for intestinal ultrasound (GIUS) in inflammatory bowel diseases. Ultraschall Med. 2018; 39:304–317.
Article4. Panés J, Bouzas R, Chaparro M, et al. Systematic review: the use of ultrasonography, computed tomography and magnetic resonance imaging for the diagnosis, assessment of activity and abdominal complications of Crohn’s disease. Aliment Pharmacol Ther. 2011; 34:125–145.
Article5. Calabrese E, Maaser C, Zorzi F, et al. Bowel ultrasonography in the management of Crohn’s disease: a review with recommendations of an International Panel of Experts. Inflamm Bowel Dis. 2016; 22:1168–1183.
Article6. Ripollés T, Martínez-Pérez MJ, Blanc E, et al. Contrast-enhanced ultrasound (CEUS) in Crohn’s disease: technique, image interpretation and clinical applications. Insights Imaging. 2011; 2:639–652.7. Quaia E. Contrast-enhanced ultrasound of the small bowel in Crohn’s disease. Abdom Imaging. 2013; 38:1005–1013.8. Jones B, Fishman EK, Hamilton SR, et al. Submucosal accumulation of fat in inflammatory bowel disease: CT/pathologic correlation. J Comput Assist Tomogr. 1986; 10:759–763.9. Amitai MM, Arazi-Kleinman T, Avidan B, et al. Fat halo sign in the bowel wall of patients with Crohn’s disease. Clin Radiol. 2007; 62:994–997.10. Rimola J, Rodríguez S, Cabanas ML, Ayuso C, Panés J, Cuatrecasas M. MRI of Crohn’s disease: from imaging to pathology. Abdom Imaging. 2012; 37:387–396.11. Kimmey MB, Martin RW, Haggitt RC, Wang KY, Franklin DW, Silverstein FE. Histologic correlates of gastrointestinal ultrasound images. Gastroenterology. 1989; 96(2 Pt 1):433–441.
Article12. Punwani S, Rodriguez-Justo M, Bainbridge A, et al. Mural inflammation in Crohn disease: location-matched histologic validation of MR imaging features. Radiology. 2009; 252:712–720.
Article13. Zappa M, Stefanescu C, Cazals-Hatem D, et al. Which magnetic resonance imaging findings accurately evaluate inflammation in small bowel Crohn’s disease? A retrospective comparison with surgical pathologic analysis. Inflamm Bowel Dis. 2011; 17:984–993.
Article14. Bryant RV, Friedman AB, Wright EK, et al. Gastrointestinal ultrasound in inflammatory bowel disease: an underused resource with potential paradigm-changing application. Gut. 2018; 67:973–985.
Article15. Moreno N, Ripollés T, Paredes JM, et al. Usefulness of abdominal ultrasonography in the analysis of endoscopic activity in patients with Crohn’s disease: changes following treatment with immunomodulators and/or anti-TNF antibodies. J Crohns Colitis. 2014; 8:1079–1087.
Article16. Novak KL, Nylund K, Maaser C, et al. Expert consensus on optimal acquisition and development of the International Bowel Ultrasound Segmental Activity Score [IBUS-SAS]: a reliability and inter-rater variability study on intestinal ultrasonography in Crohn’s disease. J Crohns Colitis. 2021; 15:609–616.17. Medellin-Kowalewski A, Wilkens R, Wilson A, Ruan J, Wilson SR. Quantitative contrast-enhanced ultrasound parameters in Crohn disease: their role in disease activity determination with ultrasound. AJR Am J Roentgenol. 2016; 206:64–73.18. Sævik F, Eriksen R, Eide GE, Gilja OH, Nylund K. Development and validation of a simple ultrasound activity score for Crohn’s disease. J Crohns Colitis. 2021; 15:115–124.19. Novak KL, Kaplan GG, Panaccione R, et al. A simple ultrasound score for the accurate detection of inflammatory activity in Crohn’s disease. Inflamm Bowel Dis. 2017; 23:2001–2010.20. Ripollés T, Poza J, Suarez Ferrer C, Martínez-Pérez MJ, Martín-Algíbez A, de Las Heras Paez B. Evaluation of Crohn’s disease activity: development of an ultrasound score in a multicenter study. Inflamm Bowel Dis. 2021; 27:145–154.
Article21. Castiglione F, de Sio I, Cozzolino A, et al. Bowel wall thickness at abdominal ultrasound and the one-year-risk of surgery in patients with Crohn’s disease. Am J Gastroenterol. 2004; 99:1977–1983.
Article22. Ripollés T, Paredes JM, Martínez-Pérez MJ, et al. Ultrasonographic changes at 12 weeks of anti-TNF drugs predict 1-year sonographic response and clinical outcome in Crohn’s disease: a multicenter study. Inflamm Bowel Dis. 2016; 22:2465–2473.
Article23. Kucharzik T, Wittig BM, Helwig U, et al. Use of intestinal ultrasound to monitor Crohn’s disease activity. Clin Gastroenterol Hepatol. 2017; 15:535–542.
Article24. Medellin A, Merrill C, Wilson SR. Role of contrast-enhanced ultrasound in evaluation of the bowel. Abdom Radiol (NY). 2018; 43:918–933.
Article25. Ripollés T, Martínez-Pérez MJ, Paredes JM, Vizuete J, Martin G. The role of intravenous contrast agent in the sonographic assessment of Crohn’s disease activity: is contrast agent injection necessary? J Crohns Colitis. 2019; 13:585–592.
Article26. Schoepfer AM, Dehlavi MA, Fournier N, et al. Diagnostic delay in Crohn’s disease is associated with a complicated disease course and increased operation rate. Am J Gastroenterol. 2013; 108:1744–1753.
Article27. Muldowney SM, Balfe DM, Hammerman A, Wick MR. “Acute” fat deposition in bowel wall submucosa: CT appearance. J Comput Assist Tomogr. 1995; 19:390–393.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of secondary renal amyloidosis complicating Crohn's disease
- Primary hypertrophic osteoarthropathy accompanied by Crohn's disease: a case report
- A case of Crohn disease
- Visceral Fat as a Useful Parameter in the Differential Diagnosis of Crohn's Disease and Intestinal Tuberculosis
- Comparative Study between Axial and Coronal Planes of CT Enterography in Evaluation of Disease Activity and Complications of Crohn Disease