Intest Res.
2023 Jul;21(3):363-374. 10.5217/ir.2023.00015.
Vaccination in patients with inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine and Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
- 3Department of Internal Medicine, Inje University Busan Paik Hospital, Busan, Korea
- 4Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea
- 5Department of Internal Medicine, National Taiwan University Hospital, Taipei, Taiwan
- 6Division of Gastroenterology, The First University Hospital, Sun Yat-sen University, Guangzhou, China
- 7Division of Gastroenterology and Hepatology, Department of Internal Medicine, Toho University Sakura Medical Center, Sakura, Japan
- KMID: 2544759
- DOI: http://doi.org/10.5217/ir.2023.00015
Abstract
- Background/Aims
Long-term immunosuppressive therapies used to treat inflammatory bowel disease (IBD) are associated with an increased risk of infections, many of which can be prevented by vaccination. We assessed physicians’ current approaches and clinical practices regarding vaccinations for IBD patients in different Asian countries/regions.
Methods
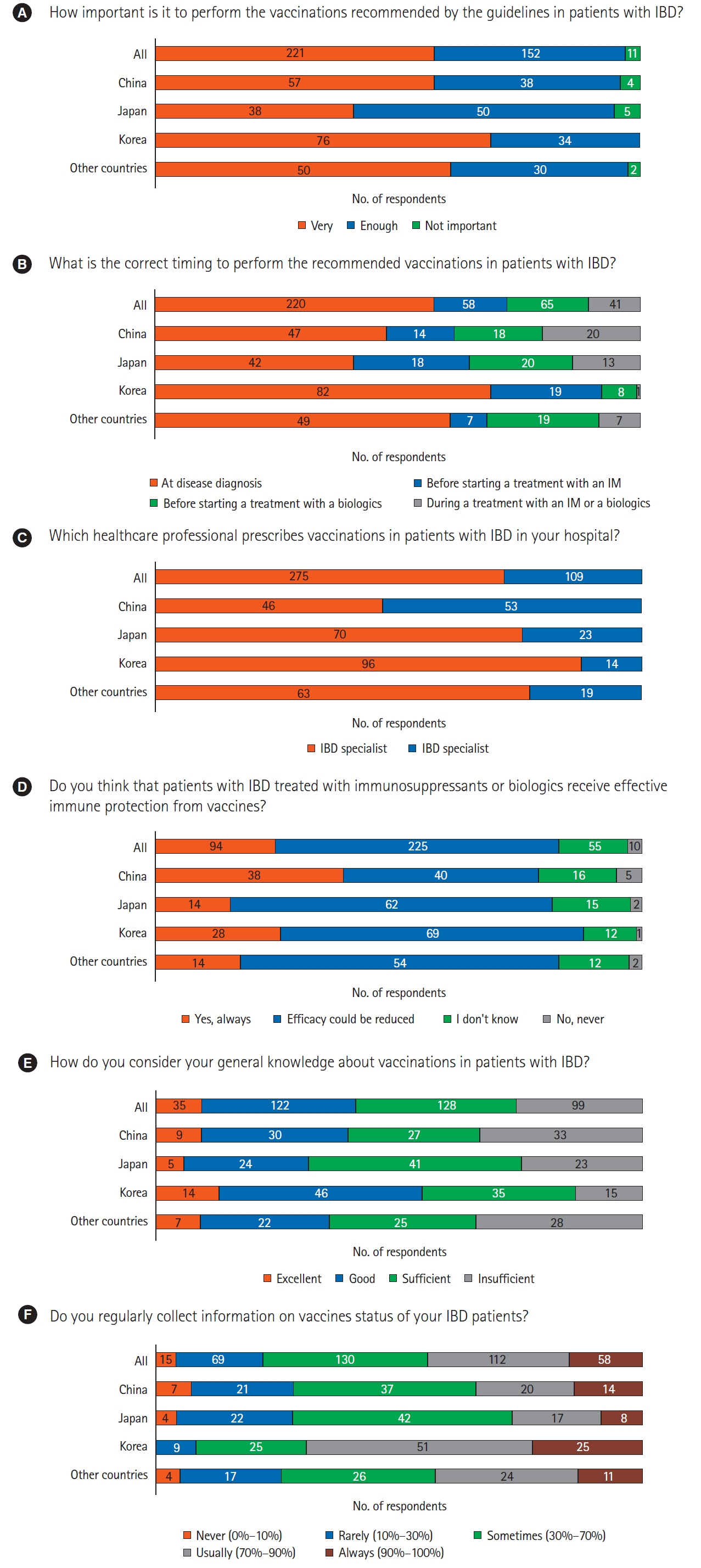
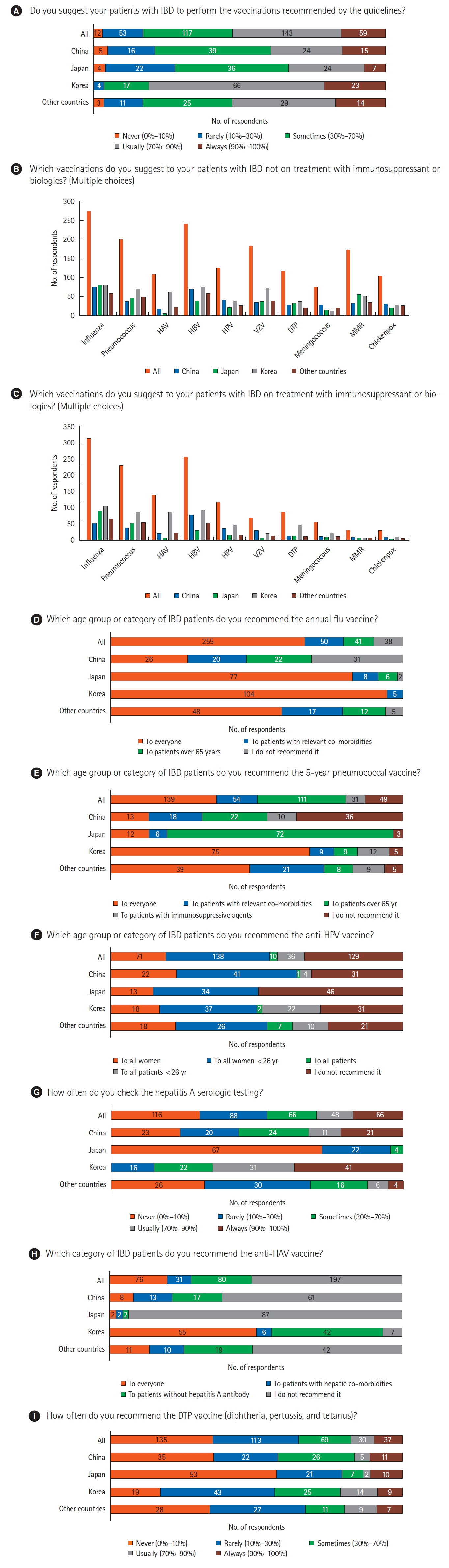
An internet-based survey was conducted among members of the Asian Organization for Crohn’s and Colitis from September 2020 to November 2020. The questionnaire consisted of 2 parts covering general opinion on the relevance of vaccinations and clinical practice of vaccination.
Results
Overall, 384 Asian medical doctors responded to the survey. The majority of respondents considered it very (57.6%) or sufficiently (39.6%) important to perform vaccinations as recommended by the guidelines. About half of the Asian physicians (52.6%) were usually or always performing vaccinations. The influenza vaccine was the most frequently recommended vaccine for IBD patients. Half of the respondents (51.3%) did not recommend hepatitis A vaccine, especially in China (61.6%) and Japan (93.6%). The diphtheria, tetanus, and pertussis vaccine were never (35.2%) or rarely (29.4%) recommended.
Conclusions
The findings of this survey indicated similarities among countries/regions in terms of the current approaches and practices regarding vaccination of IBD patients; however, there are some differences that might reflect each country’s domestic vaccination guidelines and health insurance particularly with certain vaccines in some countries/regions. Although Asian physicians largely recommend vaccination, more awareness among doctors and Asian consensus regarding differences in IBD vaccination among countries/regions may be required.
Figure
Reference
-
1. Kochar B, Herfarth HH. Vaccinations in adult patients with inflammatory bowel diseases in the West. Inflamm Intest Dis. 2018; 3:11–15.
Article2. Kim ES, Chen M, Lee J, Lee CK, Kim YS. Diagnosis of inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 2(nd) Asian Organization for Crohn’s and Colitis (AOCC) meeting in Seoul. Intest Res. 2016; 14:224–230.
Article3. Manser CN, Maillard MH, Rogler G, et al. Vaccination in patients with inflammatory bowel diseases. Digestion. 2020; 101 Suppl 1(Suppl 1):58–68.
Article4. Rahier JF, Magro F, Abreu C, et al. Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2014; 8:443–468.
Article5. Farraye FA, Melmed GY, Lichtenstein GR, Kane SV. ACG clinical guideline: preventive care in inflammatory bowel disease. Am J Gastroenterol. 2017; 112:241–258.
Article6. Wasan SK, Calderwood AH, Long MD, Kappelman MD, Sandler RS, Farraye FA. Immunization rates and vaccine beliefs among patients with inflammatory bowel disease: an opportunity for improvement. Inflamm Bowel Dis. 2014; 20:246–250.
Article7. Melmed GY, Ippoliti AF, Papadakis KA, et al. Patients with inflammatory bowel disease are at risk for vaccine-preventable illnesses. Am J Gastroenterol. 2006; 101:1834–1840.
Article8. Malhi G, Rumman A, Thanabalan R, et al. Vaccination in inflammatory bowel disease patients: attitudes, knowledge, and uptake. J Crohns Colitis. 2015; 9:439–444.
Article9. Coenen S, Weyts E, Jorissen C, et al. Effects of education and information on vaccination behavior in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2017; 23:318–324.
Article10. Manthiram K, Blood EA, Kuppuswamy V, et al. Predictors of optional immunization uptake in an urban south Indian population. Vaccine. 2014; 32:3417–3423.
Article11. Tinsley A, Navabi S, Williams ED, et al. Increased risk of influenza and influenza-related complications among 140,480 patients with inflammatory bowel disease. Inflamm Bowel Dis. 2019; 25:369–376.12. Bonovas S, Minozzi S, Lytras T, et al. Risk of malignancies using anti-TNF agents in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis: a systematic review and metaanalysis. Expert Opin Drug Saf. 2016; 15(sup1):35–54.13. Narula N, Dhillon AS, Chauhan U, Marshall JK. An audit of influenza vaccination status in adults with inflammatory bowel disease. Can J Gastroenterol. 2012; 26:593–596.14. Wasan SK, Coukos JA, Farraye FA. Vaccinating the inflammatory bowel disease patient: deficiencies in gastroenterologists knowledge. Inflamm Bowel Dis. 2011; 17:2536–2540.15. Yeung JH, Goodman KJ, Fedorak RN. Inadequate knowledge of immunization guidelines: a missed opportunity for preventing infection in immunocompromised IBD patients. Inflamm Bowel Dis. 2012; 18:34–40.
Article16. Jung YS, Park JH, Kim HJ, et al. Insufficient knowledge of Korean gastroenterologists regarding the vaccination of patients with inflammatory bowel disease. Gut Liver. 2014; 8:242–247.
Article17. Gupta A, Macrae FA, Gibson PR. Vaccination and screening for infections in patients with inflammatory bowel disease: a survey of Australian gastroenterologists. Intern Med J. 2011; 41:462–467.
Article18. Visser LG. The immunosuppressed traveler. Infect Dis Clin North Am. 2012; 26:609–624.
Article19. Reich J, Wasan S, Farraye FA. Vaccinating patients with inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2016; 12:540–546.20. Nguyen DL, Nguyen ET, Bechtold ML. Effect of immunosuppressive therapies for the treatment of inflammatory bowel disease on response to routine vaccinations: a meta-analysis. Dig Dis Sci. 2015; 60:2446–2453.
Article21. Gelinck LB, van der Bijl AE, Beyer WE, et al. The effect of antitumour necrosis factor alpha treatment on the antibody response to influenza vaccination. Ann Rheum Dis. 2008; 67:713–716.
Article22. Dotan I, Werner L, Vigodman S, et al. Normal response to vaccines in inflammatory bowel disease patients treated with thiopurines. Inflamm Bowel Dis. 2012; 18:261–268.
Article23. Lee YJ, Kim ES. Vaccination strategies for Korean patients with inflammatory bowel disease. Korean J Intern Med. 2022; 37:920–930.
Article24. Long MD, Martin C, Sandler RS, Kappelman MD. Increased risk of herpes zoster among 108 604 patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2013; 37:420–429.
Article25. Winthrop KL, Melmed GY, Vermeire S, et al. Herpes zoster infection in patients with ulcerative colitis receiving tofacitinib. Inflamm Bowel Dis. 2018; 24:2258–2265.
Article26. Khan N, Patel D, Trivedi C, et al. Overall and comparative risk of herpes zoster with pharmacotherapy for inflammatory bowel diseases: a nationwide cohort study. Clin Gastroenterol Hepatol. 2018; 16:1919–1927.
Article27. Harpaz R, Ortega-Sanchez IR, Seward JF; Advisory Committee on Immunization Practices (ACIP) Centers for Disease Control and Prevention (CDC). Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2008; 57(RR-5):1–30.28. Lee YJ, Kim SE, Park YE, et al. SARS-CoV-2 vaccination for adult patients with inflammatory bowel disease: expert consensus statement by KASID. Intest Res. 2022; 20:171–183.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
- Treatment of inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 2nd Asian Organization of Crohn's and Colitis (AOCC) meeting in Seoul
- Diagnosis of inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 2nd Asian Organization for Crohn's and Colitis (AOCC) meeting in Seoul
- Treatment of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
- Infectious complications in patients with inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting