Clin Endosc.
2023 Jul;56(4):423-432. 10.5946/ce.2023.104.
Management of complications related to colorectal endoscopic submucosal dissection
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2544563
- DOI: http://doi.org/10.5946/ce.2023.104
Abstract
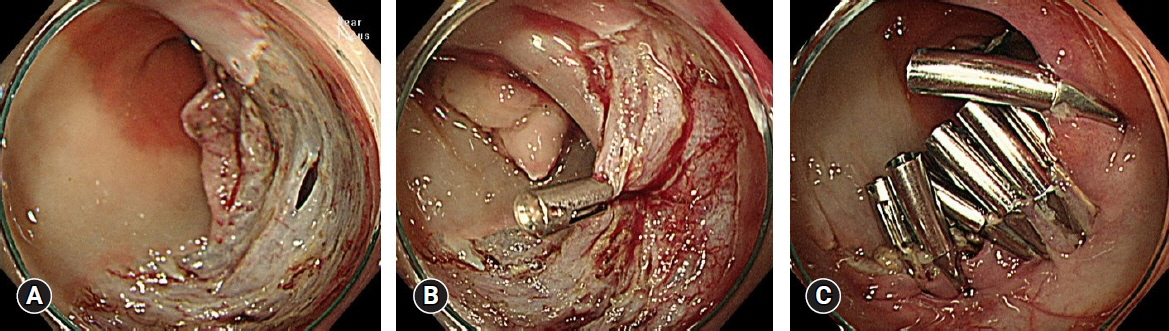
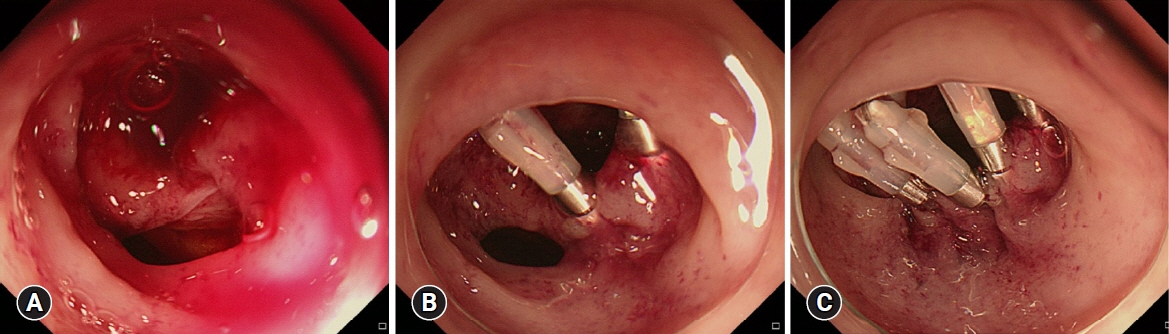
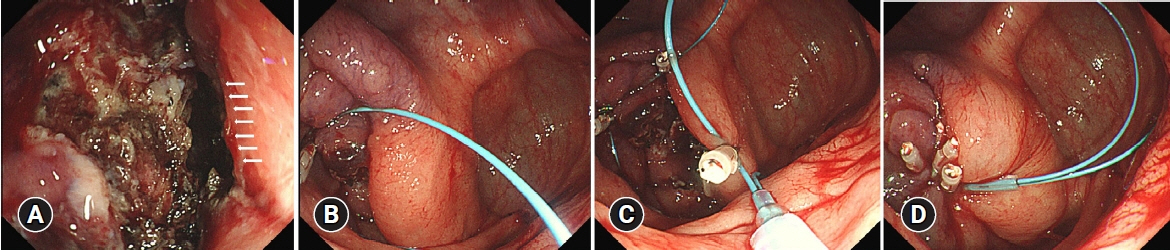
- Compared to endoscopic mucosal resection (EMR), colonoscopic endoscopic submucosal dissection (C-ESD) has the advantages of higher en bloc resection rates and lower recurrence rates of colorectal neoplasms. Therefore, C-ESD is considered an effective treatment method for laterally spread tumors and early colorectal cancer. However, C-ESD is technically more difficult and requires a longer procedure time than EMR. In addition to therapeutic efficacy and procedural difficulty, safety concerns should always be considered when performing C-ESD in clinical practice. Bleeding and perforation are the main adverse events associated with C-ESD and can occur during C-ESD or after the completion of the procedure. Most bleeding associated with C-ESD can be managed endoscopically, even if it occurs during or after the procedure. More recently, most perforations identified during C-ESD can also be managed endoscopically, unless the mural defect is too large to be sutured with endoscopic devices or the patient is hemodynamically unstable. Delayed perforations are quite rare, but they require surgical treatment more frequently than endoscopically identified intraprocedural perforations or radiologically identified immediate postprocedural perforations. Post-ESD coagulation syndrome is a relatively underestimated adverse event, which can mimic localized peritonitis from perforation. Here, we classify and characterize the complications associated with C-ESD and recommend management options for them.
Keyword
Figure
Reference
-
1. Saunders BP, Tsiamoulos ZP. Endoscopic mucosal resection and endoscopic submucosal dissection of large colonic polyps. Nat Rev Gastroenterol Hepatol. 2016; 13:486–496.2. Kim ER, Chang DK. Management of complications of colorectal submucosal dissection. Clin Endosc. 2019; 52:114–119.3. Chow CWS, Fung TLD, Chan PT, et al. Endoscopic submucosal dissection for colorectal polyps: outcome determining factors. Surg Endosc. 2023; 37:1293–1302.4. Tamaru Y, Oka S, Tanaka S. Prevention and management of spouting bleeding during endoscopic submucosal dissection for large subpedunculated-type colonic tumor. Dig Endosc. 2018; 30:128–129.5. Hong SN, Byeon JS, Lee BI, et al. Prediction model and risk score for perforation in patients undergoing colorectal endoscopic submucosal dissection. Gastrointest Endosc. 2016; 84:98–108.6. Fuccio L, Hassan C, Ponchon T, et al. Clinical outcomes after endoscopic submucosal dissection for colorectal neoplasia: a systematic review and meta-analysis. Gastrointest Endosc. 2017; 86:74–86.7. Takamaru H, Saito Y, Yamada M, et al. Clinical impact of endoscopic clip closure of perforations during endoscopic submucosal dissection for colorectal tumors. Gastrointest Endosc. 2016; 84:494–502.8. Kamigaichi Y, Oka S, Tanaka S, et al. Factors for conversion risk of colorectal endoscopic submucosal dissection: a multicenter study. Surg Endosc. 2022; 36:5698–5709.9. Kang DU, Choi Y, Lee HS, et al. Endoscopic and clinical factors affecting the prognosis of colorectal endoscopic submucosal dissection-related perforation. Gut Liver. 2016; 10:420–428.10. Santos JB, Nobre MRC, Oliveira CZ, et al. Risk factors for adverse events of colorectal endoscopic submucosal dissection: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2021; 33(1S Suppl 1):e33–e41.11. Kuroha M, Shiga H, Kanazawa Y, et al. Factors associated with fibrosis during colorectal endoscopic submucosal dissection: does pretreatment biopsy potentially elicit submucosal fibrosis and affect endoscopic submucosal dissection outcomes? Digestion. 2021; 102:590–598.12. Odagiri H, Yasunaga H. Complications following endoscopic submucosal dissection for gastric, esophageal, and colorectal cancer: a review of studies based on nationwide large-scale databases. Ann Transl Med. 2017; 5:189.13. Misumi Y, Nonaka K. Prevention and management of complications and education in endoscopic submucosal dissection. J Clin Med. 2021; 10:2511.14. Hotta K, Oyama T, Shinohara T, et al. Learning curve for endoscopic submucosal dissection of large colorectal tumors. Dig Endosc. 2010; 22:302–306.15. Sakamoto T, Saito Y, Fukunaga S, et al. Learning curve associated with colorectal endoscopic submucosal dissection for endoscopists experienced in gastric endoscopic submucosal dissection. Dis Colon Rectum. 2011; 54:1307–1312.16. Yang DH, Jeong GH, Song Y, et al. The feasibility of performing colorectal endoscopic submucosal dissection without previous experience in performing gastric endoscopic submucosal dissection. Dig Dis Sci. 2015; 60:3431–3441.17. Jung Y. Endoscopic management of iatrogenic colon perforation. Clin Endosc. 2020; 53:29–36.18. Paspatis GA, Arvanitakis M, Dumonceau JM, et al. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement: update 2020. Endoscopy. 2020; 52:792–810.19. Okamoto Y, Oka S, Tanaka S, et al. Indications and outcomes of colorectal hybrid endoscopic submucosal dissection: a large multicenter 10-year study. Surg Endosc. 2022; 36:1894–1902.20. Romagnuolo J. Endoscopic clips: past, present and future. Can J Gastroenterol. 2009; 23:158–160.21. Galloro G, Zullo A, Luglio G, et al. Endoscopic clipping in non-variceal upper gastrointestinal bleeding treatment. Clin Endosc. 2022; 55:339–346.22. Morgan SA, Sapci I, Hrabe JE, et al. Endoscopic submucosal dissection with closure of colonic perforation using over-the-scope clip system. Dis Colon Rectum. 2019; 62:379.23. Kuwabara H, Chiba H, Tachikawa J, et al. Endoscopic closure using over-the-scope clip for delayed colonic perforation after hybrid endoscopic submucosal dissection. Endoscopy. 2020; 52:E368–E369.24. Wei MT, Ahn JY, Friedland S, et al. Over-the-Scope clip in the treatment of gastrointestinal leaks and perforations. Clin Endosc. 2021; 54:798–804.25. Matthes K, Jung Y, Kato M, et al. Efficacy of full-thickness GI perforation closure with a novel over-the-scope clip application device: an animal study. Gastrointest Endosc. 2011; 74:1369–1375.26. Lee JH, Kedia P, Stavropoulos SN, et al. AGA clinical practice update on endoscopic management of perforations in gastrointestinal tract: expert review. Clin Gastroenterol Hepatol. 2021; 19:2252–2261.27. Nakagawa Y, Nagai T, Soma W, et al. Endoscopic closure of a large ERCP-related lateral duodenal perforation by using endoloops and endoclips. Gastrointest Endosc. 2010; 72:216–217.28. Nomura T, Kobayashi M, Morikawa T, et al. Clip-fixed endoloop: an efficacious new method for mucosal defect closure. Endoscopy. 2018; 50:E126–E127.29. Ryu JY, Park BK, Kim WS, et al. Endoscopic closure of iatrogenic colon perforation using dual-channel endoscope with an endoloop and clips: methods and feasibility data (with videos). Surg Endosc. 2019; 33:1342–1348.30. Abe S, Wu SY, Ego M, et al. Efficacy of current traction techniques for endoscopic submucosal dissection. Gut Liver. 2020; 14:673–684.31. Hu X, Xu QW, Liu WH. Endoscopic loop string-assisted clip suturing closure of large mucosal defects after endoscopic submucosal dissection in the sigmoid colon. Am J Gastroenterol. 2020; 115:15.32. Repici A, Hassan C, De Paula Pessoa D, et al. Efficacy and safety of endoscopic submucosal dissection for colorectal neoplasia: a systematic review. Endoscopy. 2012; 44:137–150.33. Sakamoto T, Mori G, Yamada M, et al. Endoscopic submucosal dissection for colorectal neoplasms: a review. World J Gastroenterol. 2014; 20:16153–16158.34. Chiapponi C, Stocker U, Körner M, et al. Emergency percutaneous needle decompression for tension pneumoperitoneum. BMC Gastroenterol. 2011; 11:48.35. Raju GS, Saito Y, Matsuda T, et al. Endoscopic management of colonoscopic perforations (with videos). Gastrointest Endosc. 2011; 74:1380–1388.36. Katano T, Shimura T, Nomura S, et al. Optimal definition of coagulation syndrome after colorectal endoscopic submucosal dissection: a post hoc analysis of randomized controlled trial. Int J Colorectal Dis. 2021; 36:1479–1485.37. Ito S, Hotta K, Imai K, et al. Risk factors of post-endoscopic submucosal dissection electrocoagulation syndrome for colorectal neoplasm. J Gastroenterol Hepatol. 2018; 33:2001–2006.38. Cha JM, Lim KS, Lee SH, et al. Clinical outcomes and risk factors of post-polypectomy coagulation syndrome: a multicenter, retrospective, case-control study. Endoscopy. 2013; 45:202–207.39. Jung D, Youn YH, Jahng J, et al. Risk of electrocoagulation syndrome after endoscopic submucosal dissection in the colon and rectum. Endoscopy. 2013; 45:714–717.40. Lee SP, Sung IK, Kim JH, et al. A randomized controlled trial of prophylactic antibiotics in the prevention of electrocoagulation syndrome after colorectal endoscopic submucosal dissection. Gastrointest Endosc. 2017; 86:349–357.41. Kim SJ, Kim SY, Lee J. Prognosis and risk factors of electrocoagulation syndrome after endoscopic submucosal dissection in the colon and rectum. Large cohort study. Surg Endosc. 2022; 36:6243–6249.42. Arimoto J, Higurashi T, Kato S, et al. Risk factors for post-colorectal endoscopic submucosal dissection (ESD) coagulation syndrome: a multicenter, prospective, observational study. Endosc Int Open. 2018; 6:E342–E349.43. Shichijo S, Takeuchi Y, Shimodate Y, et al. Performance of perioperative antibiotics against post-endoscopic submucosal dissection coagulation syndrome: a multicenter randomized controlled trial. Gastrointest Endosc. 2022; 95:349–359.44. Osada T, Sakamoto N, Ritsuno H, et al. Closure with clips to accelerate healing of mucosal defects caused by colorectal endoscopic submucosal dissection. Surg Endosc. 2016; 30:4438–4444.45. Yamasaki Y, Takeuchi Y, Iwatsubo T, et al. Line-assisted complete closure for a large mucosal defect after colorectal endoscopic submucosal dissection decreased post-electrocoagulation syndrome. Dig Endosc. 2018; 30:633–641.46. Lee SP, Sung IK, Kim JH, et al. Effect of prophylactic endoscopic closure for an artificial ulceration after colorectal endoscopic submucosal dissection: a randomized controlled trial. Scand J Gastroenterol. 2019; 54:1291–1299.47. Liu M, Zhang Y, Wang Y, et al. Effect of prophylactic closure on adverse events after colorectal endoscopic submucosal dissection: a meta-analysis. J Gastroenterol Hepatol. 2020; 35:1869–1877.48. Albéniz E, Montori S, Rodríguez de Santiago E, et al. Preventing postendoscopic mucosal resection bleeding of large nonpedunculated colorectal lesions. Am J Gastroenterol. 2022; 117:1080–1088.49. Tanaka S, Kashida H, Saito Y, et al. Japan Gastroenterological Endoscopy Society guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2020; 32:219–239.50. Seo M, Song EM, Cho JW, et al. A risk-scoring model for the prediction of delayed bleeding after colorectal endoscopic submucosal dissection. Gastrointest Endosc. 2019; 89:990–998.51. Chiba H, Ohata K, Tachikawa J, et al. Delayed bleeding after colorectal endoscopic submucosal dissection: when is emergency colonoscopy needed? Dig Dis Sci. 2019; 64:880–887.52. Terasaki M, Tanaka S, Shigita K, et al. Risk factors for delayed bleeding after endoscopic submucosal dissection for colorectal neoplasms. Int J Colorectal Dis. 2014; 29:877–882.53. Suzuki S, Chino A, Kishihara T, et al. Risk factors for bleeding after endoscopic submucosal dissection of colorectal neoplasms. World J Gastroenterol. 2014; 20:1839–1845.54. Akintoye E, Kumar N, Aihara H, et al. Colorectal endoscopic submucosal dissection: a systematic review and meta-analysis. Endosc Int Open. 2016; 4:E1030–E1044.55. Tajika M, Niwa Y, Bhatia V, et al. Comparison of endoscopic submucosal dissection and endoscopic mucosal resection for large colorectal tumors. Eur J Gastroenterol Hepatol. 2011; 23:1042–1049.56. Lim XC, Nistala KRY, Ng CH, et al. Endoscopic submucosal dissection vs endoscopic mucosal resection for colorectal polyps: a meta-analysis and meta-regression with single arm analysis. World J Gastroenterol. 2021; 27:3925–3939.57. Tanaka S, Kashida H, Saito Y, et al. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015; 27:417–434.58. Saito Y, Uraoka T, Yamaguchi Y, et al. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc. 2010; 72:1217–1225.59. Nomura S, Shimura T, Katano T, et al. A multicenter, single-blind randomized controlled trial of endoscopic clipping closure for preventing coagulation syndrome after colorectal endoscopic submucosal dissection. Gastrointest Endosc. 2020; 91:859–867.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Debates on Colorectal Endoscopic Submucosal Dissection - Traction for Effective Dissection: Gravity Is Enough
- Management of Complications of Colorectal Submucosal Dissection
- A Case of Pneumorrhachis and Pneumoscrotum Following Colon Endoscopic Submucosal Dissection
- History and Development of Accessories for Endoscopic Submucosal Dissection
- Endoscopic Treatment of Subepithelial Tumors