Korean J Pain.
2023 Jul;36(3):369-381. 10.3344/kjp.23020.
The effect of graded motor imagery training on pain, functional performance, motor imagery skills, and kinesiophobia after total knee arthroplasty: randomized controlled trial
- Affiliations
-
- 1Physiotherapy and Rehabilitation Department, Faculty of Health Sciences, Inonu University, Malatya, Türkiye
- 2Department of Orthopaedics, Malatya Education and Research Hospital, Malatya, Türkiye
- KMID: 2544248
- DOI: http://doi.org/10.3344/kjp.23020
Abstract
- Background
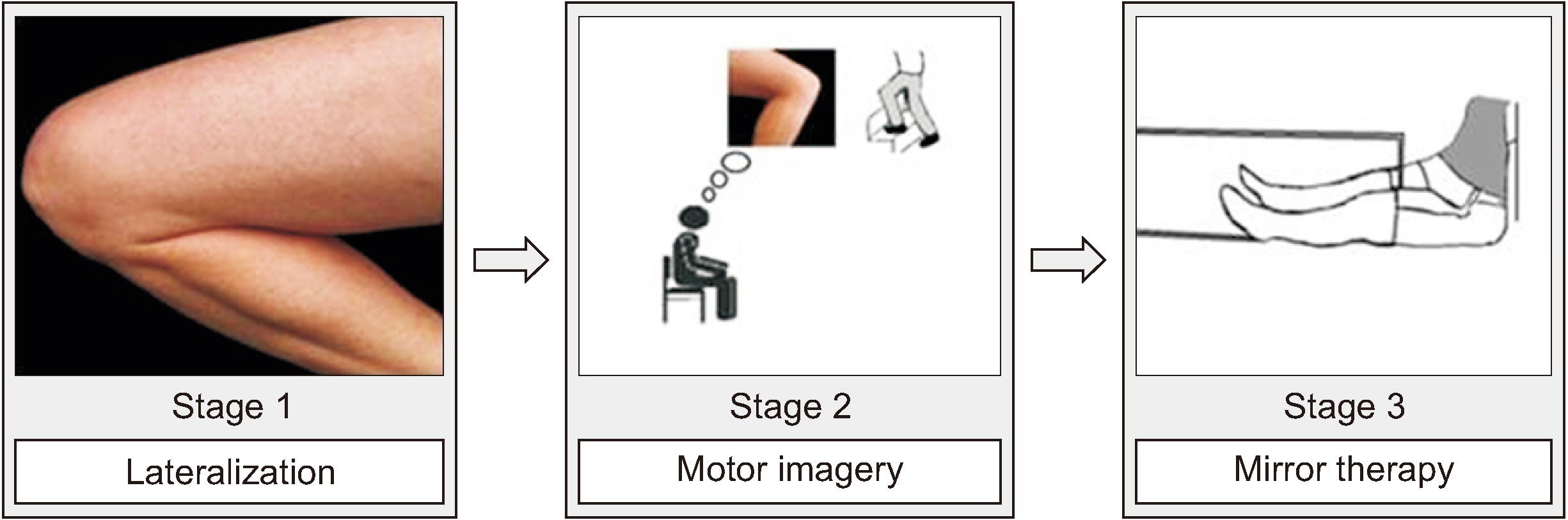
The aim was to investigate the effect of graded motor imagery (GMI) added to rehabilitation on pain, functional performance, motor imagery ability, and kinesiophobia in individuals with total knee arthroplasty (TKA).
Methods
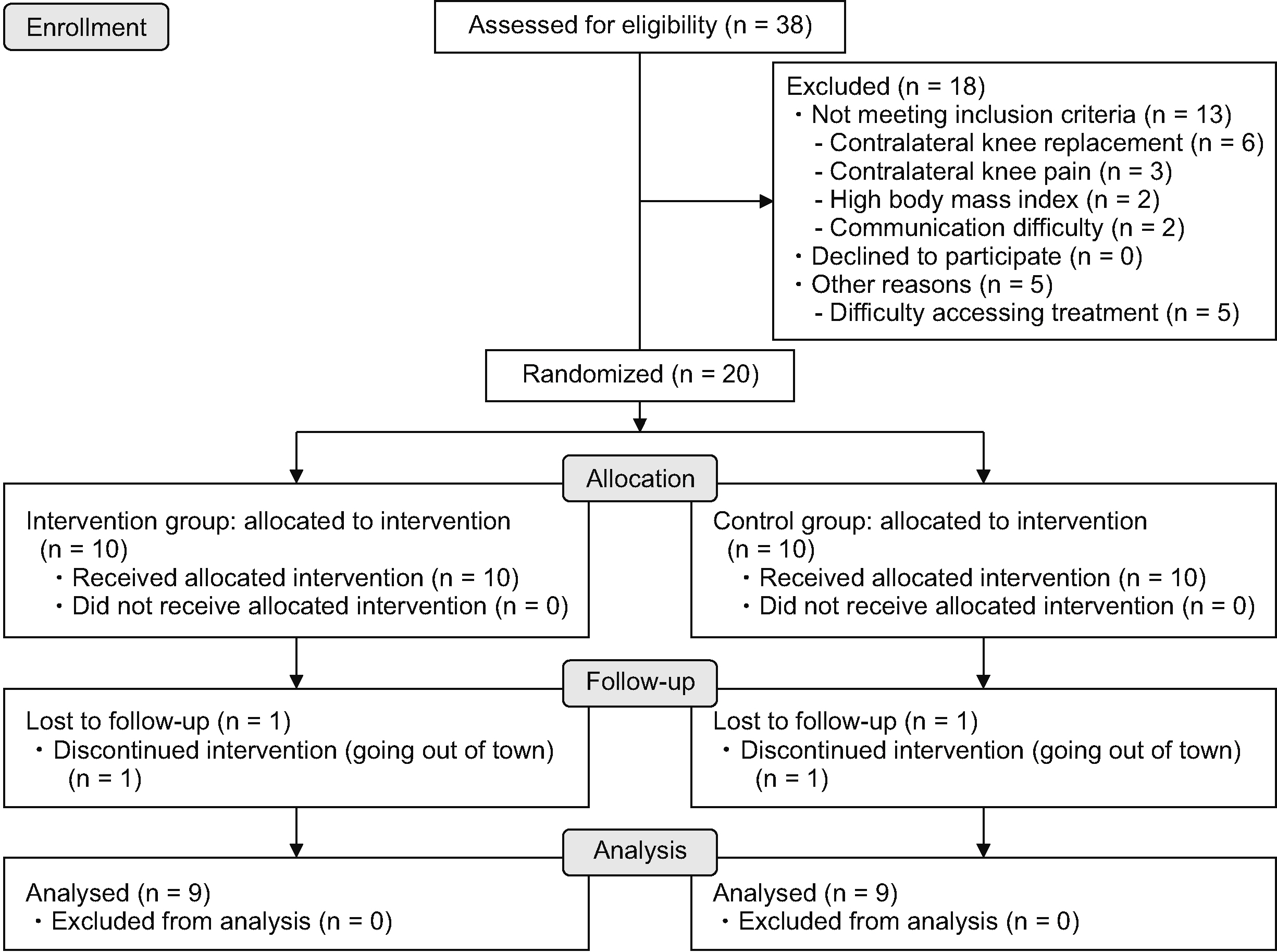
Individuals scheduled for unilateral TKA were randomized to one of two groups: control (traditional rehabilitation, n = 9) and GMI (traditional rehabilitation + GMI, n = 9) groups. The primary outcome measures were the visual analogue scale and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). Secondary outcome measures were knee range of motion, muscle strength, the timed up and go test, mental chronometer, Movement Imagery Questionnaire-3, lateralization performance, Central Sensitization Inventory, Pain Catastrophizing Scale, and Tampa Kinesiophobia Scale. Evaluations were made before and 6 weeks after surgery.
Results
Activity and resting pain were significantly reduced in the GMI group compared to the control group (P < 0.001 and P = 0.004, respectively). Movement Imagery Questionnaire-3 scores and accuracy of lateralization performance also showed significant improvement (P = 0.037 and P = 0.015, respectively). The Pain Catastrophizing Scale and Tampa Kinesiophobia Scale scores were also significantly decreased in the GMI group compared to the control group (P = 0.039 and P = 0.009, respectively). However, GMI did not differ significantly in WOMAC scores, range of motion, muscle strength, timed up and go test and Central Sensitization Inventory scores compared to the control group (P > 0.05).
Conclusions
GMI improved pain, motor imagery ability, pain catastrophizing, and kinesiophobia in the acute period after TKA.
Keyword
Figure
Reference
-
1. Zeni JA Jr, Axe MJ, Snyder-Mackler L. 2010; Clinical predictors of elective total joint replacement in persons with end-stage knee osteoarthritis. BMC Musculoskelet Disord. 11:86. DOI: 10.1186/1471-2474-11-86. PMID: 20459622. PMCID: PMC2877653. PMID: a0aed074d7604a95abe219efe8c816ab.
Article2. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. 2007; Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 89:780–5. DOI: 10.2106/00004623-200704000-00012. PMID: 17403800.
Article3. Parvizi J, Nunley RM, Berend KR, Lombardi AV Jr, Ruh EL, Clohisy JC, et al. 2014; High level of residual symptoms in young patients after total knee arthroplasty. Clin Orthop Relat Res. 472:133–7. DOI: 10.1007/s11999-013-3229-7. PMID: 24061845. PMCID: PMC3889453.
Article4. Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. 2012; What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2:e000435. DOI: 10.1136/bmjopen-2011-000435. PMID: 22357571. PMCID: PMC3289991.
Article5. Kim MS, Kim JJ, Kang KH, Kim MJ, In Y. 2022; Diagnosis of central sensitization and its effects on postoperative outcomes following total knee arthroplasty: a systematic review and meta-analysis. Diagnostics (Basel). 12:1248. DOI: 10.3390/diagnostics12051248. PMID: 35626402. PMCID: PMC9141391. PMID: d399333054cc45bb944e0cf89baa10c9.
Article6. Zapparoli L, Sacheli LM, Seghezzi S, Preti M, Stucovitz E, Negrini F, et al. 2020; Motor imagery training speeds up gait recovery and decreases the risk of falls in patients submitted to total knee arthroplasty. Sci Rep. 10:8917. DOI: 10.1038/s41598-020-65820-5. PMID: 32488010. PMCID: PMC7265300.
Article7. Briones-Cantero M, Fernández-de-Las-Peñas C, Lluch-Girbés E, Osuna-Pérez MC, Navarro-Santana MJ, Plaza-Manzano G, et al. 2020; Effects of adding motor imagery to early physical therapy in patients with knee osteoarthritis who had received total knee arthroplasty: a randomized clinical trial. Pain Med. 21:3548–55. DOI: 10.1093/pm/pnaa103. PMID: 32346743.
Article8. Moukarzel M, Di Rienzo F, Lahoud JC, Hoyek F, Collet C, Guillot A, et al. 2019; The therapeutic role of motor imagery during the acute phase after total knee arthroplasty: a pilot study. Disabil Rehabil. 41:926–33. DOI: 10.1080/09638288.2017.1419289. PMID: 29275638.
Article9. Roy JS, Bouyer LJ, Langevin P, Mercier C. 2017; Beyond the joint: the role of central nervous system reorganizations in chronic musculoskeletal disorders. J Orthop Sports Phys Ther. 47:817–21. DOI: 10.2519/jospt.2017.0608. PMID: 29089002.10. Riquelme-Hernández C, Reyes-Barría JP, Vargas A, Gonzalez-Robaina Y, Zapata-Lamana R, Toloza-Ramirez D, et al. 2022; Effects of the practice of movement representation techniques in people undergoing knee and hip arthroplasty: a systematic review. Sports (Basel). 10:198. DOI: 10.3390/sports10120198. PMID: 36548495. PMCID: PMC9782171. PMID: f42d0ec536814320af6573e6ba3bf5f2.
Article11. Moseley GL, Butler DS, Beames TB, Giles TJ. 2012. The graded motor imagery handbook. Noigroup Publications;DOI: 10.1097/01.jwh.0000438099.62316.15.12. Moseley GL. 2003; A pain neuromatrix approach to patients with chronic pain. Man Ther. 8:130–40. DOI: 10.1016/S1356-689X(03)00051-1. PMID: 12909433.
Article13. Strauss S, Barby S, Härtner J, Pfannmöller JP, Neumann N, Moseley GL, et al. 2021; Graded motor imagery modifies movement pain, cortical excitability and sensorimotor function in complex regional pain syndrome. Brain Commun. 3:fcab216. DOI: 10.1093/braincomms/fcab216. PMID: 34661105. PMCID: PMC8514858.
Article14. Moseley GL. 2005; Is successful rehabilitation of complex regional pain syndrome due to sustained attention to the affected limb? A randomised clinical trial. Pain. 114:54–61. DOI: 10.1016/j.pain.2004.11.024. PMID: 15733631.
Article15. Dilek B, Ayhan C, Yagci G, Yakut Y. 2018; Effectiveness of the graded motor imagery to improve hand function in patients with distal radius fracture: a randomized controlled trial. J Hand Ther. 31:2–9.e1. DOI: 10.1016/j.jht.2017.09.004. PMID: 29122370.
Article16. Moukarzel M, Guillot A, Di Rienzo F, Hoyek N. 2019; The therapeutic role of motor imagery during the chronic phase after total knee arthroplasty: a pilot randomized controlled trial. Eur J Phys Rehabil Med. 55:806–15. DOI: 10.23736/S1973-9087.19.05136-0. PMID: 31615192.
Article17. Louw A, Schmidt SG, Louw C, Puentedura EJ. 2015; Moving without moving: immediate management following lumbar spine surgery using a graded motor imagery approach: a case report. Physiother Theory Pract. 31:509–17. DOI: 10.3109/09593985.2015.1060656. PMID: 26395828.
Article18. Dudhani S, Anwar KAM, Jain PK. 2020; Can brain cure pain and fear? Effect of graded motor imagery on post operative lumbar degenerative diseases - randomized control trial. Indian J Physiother Occup Ther. 14:219–26. DOI: 10.37506/ijpot.v14i3.9698.19. Birinci T, Kaya Mutlu E, Altun S. 2022; The efficacy of graded motor imagery in post-traumatic stiffness of elbow: a randomized controlled trial. J Shoulder Elbow Surg. 31:2147–56. DOI: 10.1016/j.jse.2022.05.031. PMID: 35803550.
Article20. Lee HG, An J, Lee BH. 2021; The effect of progressive dynamic balance training on physical function, the ability to balance and quality of life among elderly women who underwent a total knee arthroplasty: a double-blind randomized control trial. Int J Environ Res Public Health. 18:2513. DOI: 10.3390/ijerph18052513. PMID: 33802559. PMCID: PMC7967306.
Article21. Lagueux E, Charest J, Lefrançois-Caron E, Mauger ME, Mercier E, Savard K, et al. 2012; Modified graded motor imagery for complex regional pain syndrome type 1 of the upper extremity in the acute phase: a patient series. Int J Rehabil Res. 35:138–45. DOI: 10.1097/MRR.0b013e3283527d29. PMID: 22436440.22. Bade MJ, Stevens-Lapsley JE. 2011; Early high-intensity rehabilitation following total knee arthroplasty improves outcomes. J Orthop Sports Phys Ther. 41:932–41. DOI: 10.2519/jospt.2011.3734. PMID: 21979411.23. Carlsson AM. 1983; Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain. 16:87–101. DOI: 10.1016/0304-3959(83)90088-X. PMID: 6602967.
Article24. Bellamy N, Buchanan WW, Goldsmith CH, Bellamy N, Goldsmith CH, Campbell J, et al. 1988; Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcome following total hip or knee arthroplasty in osteoarthritis. J Orthop Rheumatol. 1:95–108.25. Norkin CC, White DJ. 2016. Measurement of joint motion: a guide to goniometry. 5th ed. F.A. Davis Company;DOI: 10.1016/s0031-9406(05)66908-8.26. Daloia LMT, Leonardi-Figueiredo MM, Martinez EZ, Mattiello-Sverzut AC. 2018; Isometric muscle strength in children and adolescents using Handheld dynamometry: reliability and normative data for the Brazilian population. Braz J Phys Ther. 22:474–83. DOI: 10.1016/j.bjpt.2018.04.006. PMID: 29802034. PMCID: PMC6235825.
Article27. Podsiadlo D, Richardson S. 1991; The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 39:142–8. DOI: 10.1111/j.1532-5415.1991.tb01616.x. PMID: 1991946.
Article28. Bek J, Humphries S, Poliakoff E, Brady N. 2022; Mental rotation of hands and objects in ageing and Parkinson's disease: differentiating motor imagery and visuospatial ability. Exp Brain Res. 240:1991–2004. DOI: 10.1007/s00221-022-06389-5. PMID: 35680657. PMCID: PMC9288383.
Article29. Beauchet O, Annweiler C, Assal F, Bridenbaugh S, Herrmann FR, Kressig RW, et al. 2010; Imagined Timed Up & Go test: a new tool to assess higher-level gait and balance disorders in older adults? J Neurol Sci. 294:102–6. DOI: 10.1016/j.jns.2010.03.021. PMID: 20444477.
Article30. Dilek B, Ayhan C, Yakut Y. 2020; Reliability and validity of the Turkish version of the movement imagery questionnaire-3: its cultural adaptation and psychometric properties. Neurol Sci Neurophysiol. 37:221–7. DOI: 10.4103/NSN.NSN_30_20. PMID: b6aee2cd2e244ac4abefcc0cb98c333e.
Article31. Pelletier R, Higgins J, Bourbonnais D. 2018; Laterality recognition of images, motor performance, and aspects related to pain in participants with and without wrist/hand disorders: an observational cross-sectional study. Musculoskelet Sci Pract. 35:18–24. DOI: 10.1016/j.msksp.2018.01.010. PMID: 29427866.
Article32. Sullivan MJ, Bishop SR, Pivik J. 1995; The pain catastrophizing scale: development and validation. Psychol Assess. 7:524–32. DOI: 10.1037/1040-3590.7.4.524.
Article33. Süren M, Okan I, Gökbakan AM, Kaya Z, Erkorkmaz U, Arici S, et al. 2014; Factors associated with the pain catastrophizing scale and validation in a sample of the Turkish population. Turk J Med Sci. 44:104–8. DOI: 10.3906/sag-1206-67. PMID: 25558568.
Article34. Mayer TG, Neblett R, Cohen H, Howard KJ, Choi YH, Williams MJ, et al. 2012; The development and psychometric validation of the central sensitization inventory. Pain Pract. 12:276–85. DOI: 10.1111/j.1533-2500.2011.00493.x. PMID: 21951710. PMCID: PMC3248986.
Article35. Düzce Keleş E, Birtane M, Ekuklu G, Kılınçer C, Çalıyurt O, Taştekin N, et al. 2021; Validity and reliability of the Turkish version of the central sensitization inventory. Arch Rheumatol. 36:518–26. DOI: 10.46497/ArchRheumatol.2022.8665. PMID: 35382371. PMCID: PMC8957757.
Article36. Tunca Yılmaz Ö, Yakut Y, Uygur F, Uluğ N. 2011; Turkish version of the Tampa Scale for Kinesiophobia and its test-retest reliability. Fizyoter Rehabil. 22:44–9. Turkish.37. Fritz CO, Morris PE, Richler JJ. 2012; Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 141:2–18. Erratum in: J Exp Psychol Gen 2012; 141: 30. DOI: 10.1037/a0024338. PMID: 21823805.
Article38. Toms AD, Mandalia V, Haigh R, Hopwood B. 2009; The management of patients with painful total knee replacement. J Bone Joint Surg Br. 91:143–50. DOI: 10.1302/0301-620X.91B2.20995. PMID: 19190044.
Article39. Lewis GN, Parker RS, Sharma S, Rice DA, McNair PJ. 2018; Structural brain alterations before and after total knee arthroplasty: a longitudinal assessment. Pain Med. 19:2166–76. DOI: 10.1093/pm/pny108. PMID: 29917139.
Article40. Paravlic AH, Maffulli N, Kovač S, Pisot R. 2020; Home-based motor imagery intervention improves functional performance following total knee arthroplasty in the short term: a randomized controlled trial. J Orthop Surg Res. 15:451. DOI: 10.1186/s13018-020-01964-4. PMID: 33008432. PMCID: PMC7531130. PMID: 9a5a42e69d864bed88156ce38e842164.
Article41. Gurudut P, Godse AN. 2022; Effectiveness of graded motor imagery in subjects with frozen shoulder: a pilot randomized controlled trial. Korean J Pain. 35:152–9. DOI: 10.3344/kjp.2022.35.2.152. PMID: 35354678. PMCID: PMC8977197.
Article42. Yap BWD, Lim ECW. 2019; The effects of motor imagery on pain and range of motion in musculoskeletal disorders: a systematic review using meta-analysis. Clin J Pain. 35:87–99. DOI: 10.1097/AJP.0000000000000648. PMID: 30222613.
Article43. Skoffer B, Dalgas U, Mechlenburg I, Søballe K, Maribo T. 2015; Functional performance is associated with both knee extensor and flexor muscle strength in patients scheduled for total knee arthroplasty: a cross-sectional study. J Rehabil Med. 47:454–9. DOI: 10.2340/16501977-1940. PMID: 25678417.
Article44. Spruijt S, van der Kamp J, Steenbergen B. 2015; Current insights in the development of children's motor imagery ability. Front Psychol. 6:787. DOI: 10.3389/fpsyg.2015.00787. PMID: 26113832. PMCID: PMC4461854. PMID: 8c6865dec979428fad94c3804c898f5c.
Article45. Paravlic AH, Pisot R, Marusic U. 2019; Specific and general adaptations following motor imagery practice focused on muscle strength in total knee arthroplasty rehabilitation: a randomized controlled trial. PLoS One. 14:e0221089. DOI: 10.1371/journal.pone.0221089. PMID: 31412056. PMCID: PMC6693761. PMID: 7cd5f69c47fc4e6389c41fecc2184220.
Article46. Montuori S, Curcio G, Sorrentino P, Belloni L, Sorrentino G, Foti F, et al. 2018; Functional role of internal and external visual imagery: preliminary evidences from pilates. Neural Plast. 2018:7235872. DOI: 10.1155/2018/7235872. PMID: 29849565. PMCID: PMC5924993. PMID: b372077946eb43db877506347a6b86c2.
Article47. Breckenridge JD, Ginn KA, Wallwork SB, McAuley JH. 2019; Do people with chronic musculoskeletal pain have impaired motor imagery? A meta-analytical systematic review of the left/right judgment task. J Pain. 20:119–32. DOI: 10.1016/j.jpain.2018.07.004. PMID: 30098404.
Article48. Anderson B, Meyster V. 2018; Treatment of a patient with central pain sensitization using graded motor imagery principles: a case report. J Chiropr Med. 17:264–7. DOI: 10.1016/j.jcm.2018.05.004. PMID: 30846919. PMCID: PMC6391225.
Article49. Louw A, Puentedura EJ, Reese D, Parker P, Miller T, Mintken PE. 2017; Immediate effects of mirror therapy in patients with shoulder pain and decreased range of motion. Arch Phys Med Rehabil. 98:1941–7. DOI: 10.1016/j.apmr.2017.03.031. PMID: 28483657.
Article50. Araya-Quintanilla F, Gutiérrez-Espinoza H, Jesús Muñoz-Yanez M, Rubio-Oyarzún D, Cavero-Redondo I, Martínez-Vizcaino V, et al. 2020; The short-term effect of graded motor imagery on the affective components of pain in subjects with chronic shoulder pain syndrome: open-label single-arm prospective study. Pain Med. 21:2496–501. DOI: 10.1093/pm/pnz364. PMID: 32003812.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effectiveness of graded motor imagery in subjects with frozen shoulder: a pilot randomized controlled trial
- Effect of Motor Imagery on the F-Wave Parameters in Hemiparetic Stroke Survivors
- Dose Motor Inhibition Response Training Using Stop-signal Paradigm Influence Execution and Stop Performance?
- Motor Imagery and Action Observation
- A Meta-Analysis of the Effects of Imagery