Child Kidney Dis.
2023 Jun;27(1):46-53. 10.3339/ckd.23.008.
Pleuroperitoneal communication-associated pleuritis as an uncommon cause of fever of unknown origin in a child on peritoneal dialysis: a case report
- Affiliations
-
- 1Department of Pediatrics, Asan Medical Center Children’s Hospital, University of Ulsan College of Medicine, Seoul, Republic of Korea
- KMID: 2544237
- DOI: http://doi.org/10.3339/ckd.23.008
Abstract
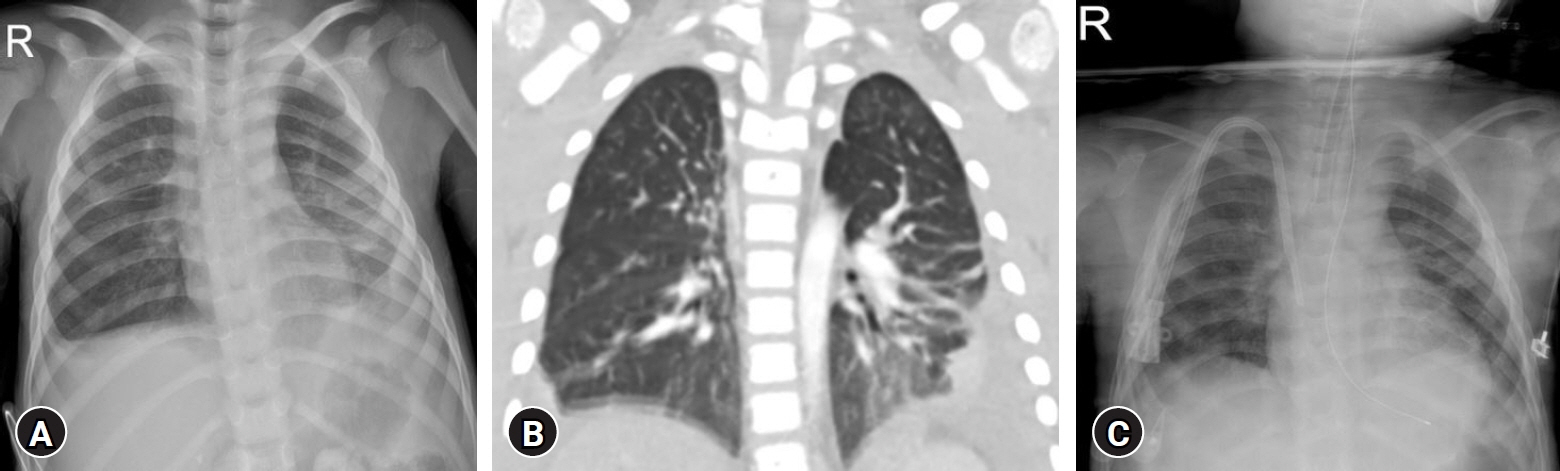
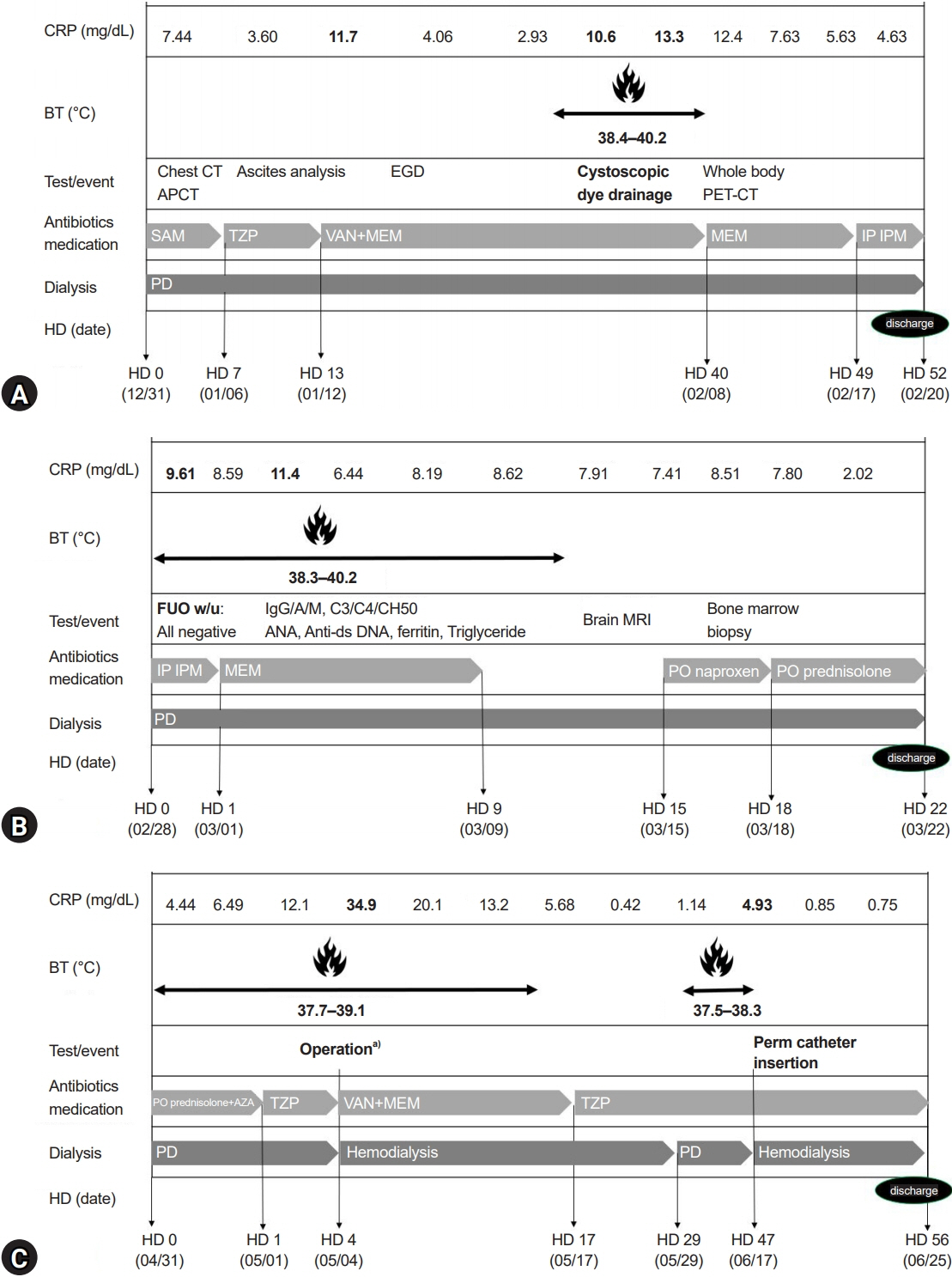
- Pleuroperitoneal communication (PPC) is a rare mechanical complication of peritoneal dialysis (PD), which causes dialysate to move from the peritoneal cavity to the pleural cavity, resulting in pleural effusion. Typically, PPC is discovered through pleural effusion in PD patients who are not in volume overload status. A unique characteristic of the pleural effusion caused by PPC is that it is not resolved by increasing ultrafiltration by dialysis. In this report, we present a 7-year-old girl with PD after birth with the history of various infectious PD-related complications, presenting with fever ongoing for 6 months. PPC-associated pleuritis was suspected as the cause of fever, which eventually developed after long-term PD and induced complicated pleural effusion, lung inflammation, and prolonged fever for 6 months.
Keyword
Figure
Reference
-
References
1. Verrina E, Edefonti A, Gianoglio B, Rinaldi S, Sorino P, Zacchello G, et al. A multicenter experience on patient and technique survival in children on chronic dialysis. Pediatr Nephrol. 2004; 19:82–90.
Article2. Verrina E. Peritoneal dialysis. In : Avner ED, Harmon WE, Niaudet P, Yoshikawa N, editors. Pediatric nephrology. 6th ed. Springer;2009. p. 1785–810.3. Ambarsari CG, Bermanshah EK, Putra MA, Rahman FHF, Pardede SO. Effective management of peritoneal dialysis-associated hydrothorax in a child: a case report. Case Rep Nephrol Dial. 2020; 10:18–25.
Article4. Crabtree JH. Rescue and salvage procedures for mechanical and infectious complications of peritoneal dialysis. Int J Artif Organs. 2006; 29:67–8.
Article5. Kennedy C, McCarthy C, Alken S, McWilliams J, Morgan RK, Denton M, et al. Pleuroperitoneal leak complicating peritoneal dialysis: a case series. Int J Nephrol. 2011; 2011:526753.
Article6. Dufek S, Holtta T, Fischbach M, Ariceta G, Jankauskiene A, Cerkauskiene R, et al. Pleuro-peritoneal or pericardio-peritoneal leak in children on chronic peritoneal dialysis: a survey from the European Paediatric Dialysis Working Group. Pediatr Nephrol. 2015; 30:2021–7.
Article7. Dang MH, Mathew M, Raj R. Pleuroperitoneal leak as an uncommon cause of pleural effusion in peritoneal dialysis: a case report and literature review. Case Rep Nephrol. 2020; 2020:8832080.
Article8. Cho HY, Lee BS, Kang CH, Kim WH, Ha IS, Cheong HI, et al. Hydrothorax in a patient with Denys-Drash syndrome associated with a diaphragmatic defect. Pediatr Nephrol. 2006; 21:1909–12.
Article9. Yaxley J, Twomey K. Peritoneal dialysis complicated by pleuroperitoneal communication and hydrothorax. Ochsner J. 2017; 17:124–7.10. Chow KM, Szeto CC, Li PK. Management options for hydrothorax complicating peritoneal dialysis. Semin Dial. 2003; 16:389–94.11. Bohra N, Sullivan A, Chaudhary H, Demko T. The use of pleural fluid to serum glucose ratio in establishing the diagnosis of a not so sweet PD-related hydrothorax: case report and literature review. Case Rep Nephrol. 2020; 2020:8811288.
Article12. Alhasan KA. Recurrent hydrothorax in a child on peritoneal dialysis: a case report and review of the literature. Clin Case Rep. 2018; 7:149–51.
Article13. Aksoy OY, Gulaldi NCM, Bayrakci US. Hydrothorax in a pediatric patient on peritoneal dialysis: Answers. Pediatr Nephrol. 2020; 35:1421–3.
Article14. Dai BB, Lin BD, Yang LY, Wan JX, Pan YB. Novel conservative treatment for peritoneal dialysis-related hydrothorax: Two case reports. World J Clin Cases. 2020; 8:6437–43.
Article15. Mori T, Fujino A, Takahashi M, Furugane R, Kobayashi T, Kano M, et al. Successful endoscopic surgical treatment of pleuroperitoneal communication in two infant cases. Surg Case Rep. 2021; 7:181.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of hydrothorax in peritoneal dialysis
- A Rare Case of Unilateral Pleural Effusion in a Pediatric Patient on Chronic Peritoneal Dialysis: Is it a Pleuroperitoneal Leakage?
- Aortic dissection presenting as fever of unknown origin
- Non-Infectious Diseases Causing Fever of Unknown Origin
- Two Cases of Hydrothorax Associated with Pleuroperitoneal Communications Proved by CT Peritoneography and Peritoneoscintigraphy