Child Kidney Dis.
2023 Jun;27(1):26-33. 10.3339/ckd.23.005.
Clinical practice pattern on hematuria and proteinuria in children: the report of a survey for the Korean Society of Pediatric Nephrology
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul, Republic of Korea
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Republic of Korea
- 3Kidney Research Institute, Seoul National University College of Medicine, Seoul, Republic of Korea
- KMID: 2544234
- DOI: http://doi.org/10.3339/ckd.23.005
Abstract
- Purpose
Hematuria and proteinuria have various causes and consequential outcomes in children. Immunosuppressants are needed in some children with biopsy-proven glomerulonephropathy but have many adverse effects. Since the clinical practice patterns of Korean pediatric nephrologists are diverse, we surveyed their opinions.
Methods
Using a clinical vignette, the survey was emailed to all Korean Society of Pediatric Nephrology members. The questionnaires included diagnosis, examination, medications, and dietary recommendations for patients with hematuria and proteinuria.
Results
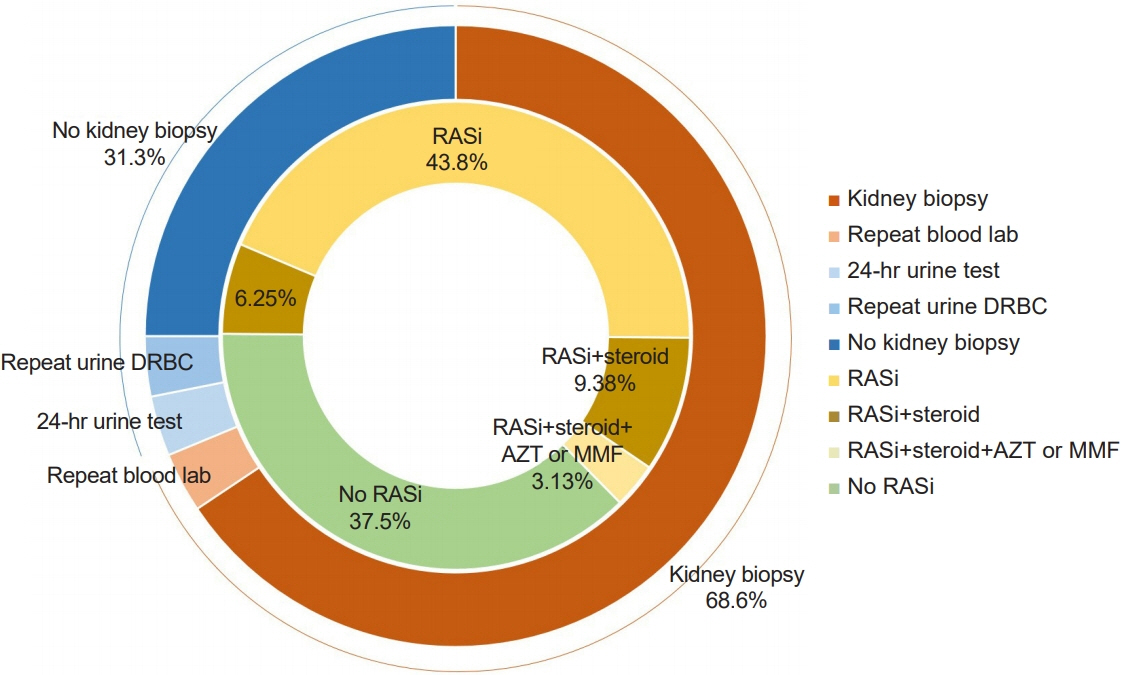
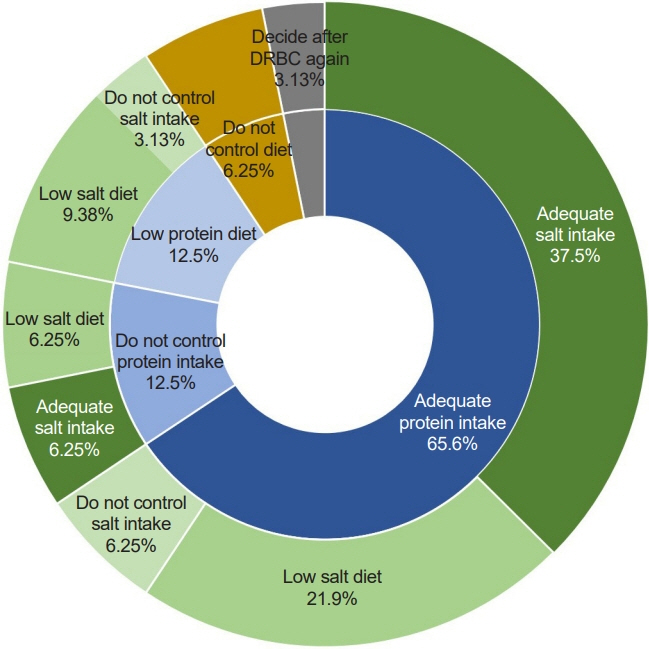
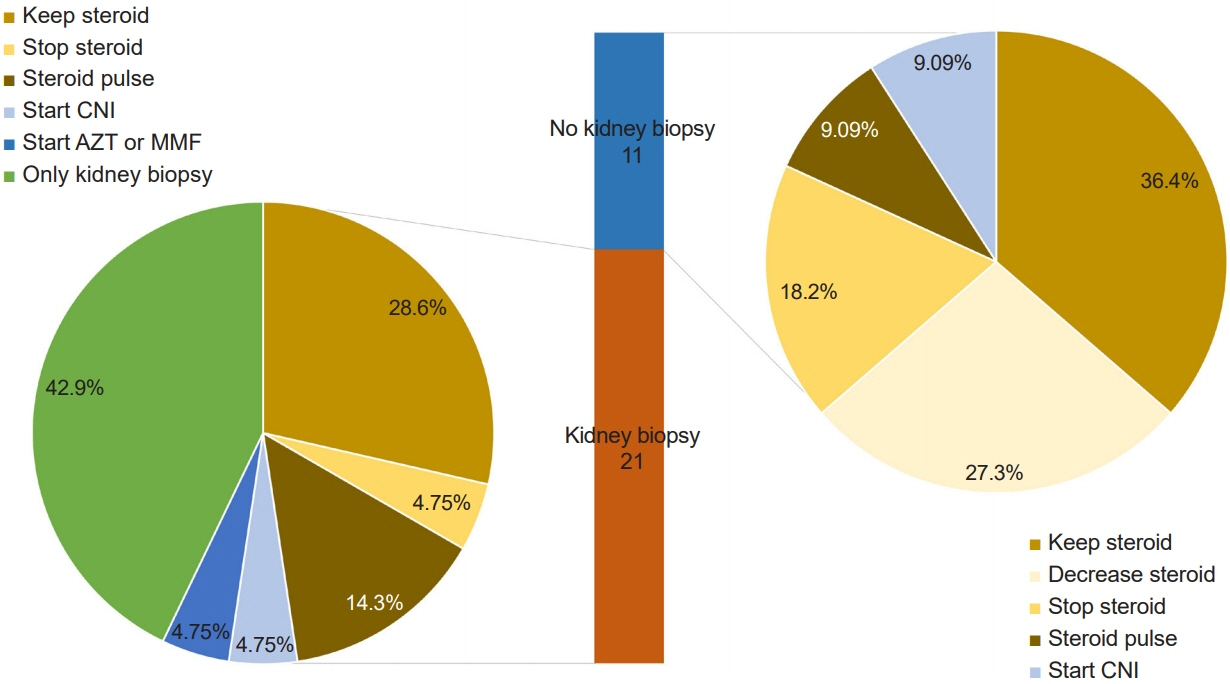
A total of 32 clinicians (5.48%, 22 pediatric certificated nephrologists) responded to the survey. Most responders (87.5%) suspected immunoglobulin A nephropathy, and 68.8% replied that kidney biopsies were a diagnostic tool. Renin-angiotensin system inhibition (62.5%) or steroids (18.8%) were selected as the treatment. Salt and protein intakes were usually encouraged as dietary reference intakes (34.4% and 65.6%, respectively).
Conclusions
Children with abnormal urinalysis have various causes, treatments, and prognoses. As treatments such as immunosuppressants can have many adverse effects, it is necessary to confirm an accurate diagnosis and indications of treatments before starting the treatment. Recommendations for a diet should not hinder growth.
Figure
Reference
-
References
1. Viteri B, Reid-Adam J. Hematuria and proteinuria in children. Pediatr Rev. 2018; 39:573–87.
Article2. Korean Society of Pediatric Nephrology. Korean Society of Pediatric Nephrology 2023 recommendations on diagnosis and management of children with hematuria [Internet]. Korean Society of Pediatric Nephrology. 2023 [cited 2023 Feb 22]. Available from: https://kspn.org/mail/file/m230522.pdf.3. Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group. KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. 2021; 100(4S):S1–276.4. Horie S, Ito S, Okada H, Kikuchi H, Narita I, Nishiyama T, et al. Japanese guidelines of the management of hematuria 2013. Clin Exp Nephrol. 2014; 18:679–89.
Article5. Yap HK, Shenoy M. Approach to the child with hematuria and/or proteinuria. In : Emma F, Goldstein SL, Bagga A, Bates CM, Shroff R, editors. Pediatric nephrology. Springer International Publishing;2022. p. 235–52.6. Murakami M, Yamamoto H, Ueda Y, Murakami K, Yamauchi K. Urinary screening of elementary and junior high-school children over a 13-year period in Tokyo. Pediatr Nephrol. 1991; 5:50–3.
Article7. Cho BS, Hahn WH, Cheong HI, Lim I, Ko CW, Kim SY, et al. A nationwide study of mass urine screening tests on Korean school children and implications for chronic kidney disease management. Clin Exp Nephrol. 2013; 17:205–10.
Article8. Lee YM, Baek SY, Kim JH, Kim DS, Lee JS, Kim PK. Analysis of renal biopsies performed in children with abnormal findings in urinary mass screening. Acta Paediatr. 2006; 95:849–53.
Article9. Yum MS, Yoon HS, Lee JH, Hahn H, Park YS. Follow-up of children with isolated microscopic hematuria detected in a mass school urine screening test. Korean J Pediatr. 2006; 49:82–6.
Article10. Lin CY, Hsieh CC, Chen WP, Yang LY, Wang HH. The underlying diseases and follow-up in Taiwanese children screened by urinalysis. Pediatr Nephrol. 2001; 16:232–7.
Article11. Whittier WL. Complications of the percutaneous kidney biopsy. Adv Chronic Kidney Dis. 2012; 19:179–87.
Article12. Feld LG, Stapleton FB, Duffy L. Renal biopsy in children with asymptomatic hematuria or proteinuria: survey of pediatric nephrologists. Pediatr Nephrol. 1993; 7:441–3.
Article13. HodFeins R, Tobar A, Davidovits M. Yield and complications of kidney biopsy over two decades in a tertiary pediatric center. Pediatr Int. 2017; 59:452–7.
Article14. Scheckner B, Peyser A, Rube J, Tarapore F, Frank R, Vento S, et al. Diagnostic yield of renal biopsies: a retrospective single center review. BMC Nephrol. 2009; 10:11.
Article15. Pilania RK, Venkatesh GV, Nada R, Vignesh P, Jindal AK, Suri D, et al. Renal biopsy in children-effect on treatment decisions: a single-center experience. Indian J Pediatr. 2021; 88:1036–9.
Article16. Spahn JD, Kamada AK. Special considerations in the use of glucocorticoids in children. Pediatr Rev. 1995; 16:266–72.
Article17. Yuzawa Y, Yamamoto R, Takahashi K, Katafuchi R, Tomita M, Fujigaki Y, et al. Evidence-based clinical practice guidelines for IgA nephropathy 2014. Clin Exp Nephrol. 2016; 20:511–35.
Article18. Pozzi C, Bolasco PG, Fogazzi GB, Andrulli S, Altieri P, Ponticelli C, et al. Corticosteroids in IgA nephropathy: a randomised controlled trial. Lancet. 1999; 353:883–7.
Article19. Lv J, Zhang H, Wong MG, Jardine MJ, Hladunewich M, Jha V, et al. Effect of oral methylprednisolone on clinical outcomes in patients with IgA nephropathy: the TESTING Randomized Clinical Trial. JAMA. 2017; 318:432–42.
Article20. Lv J, Zhang H, Chen Y, Li G, Jiang L, Singh AK, et al. Combination therapy of prednisone and ACE inhibitor versus ACE-inhibitor therapy alone in patients with IgA nephropathy: a randomized controlled trial. Am J Kidney Dis. 2009; 53:26–32.
Article21. Manno C, Torres DD, Rossini M, Pesce F, Schena FP. Randomized controlled clinical trial of corticosteroids plus ACE-inhibitors with long-term follow-up in proteinuric IgA nephropathy. Nephrol Dial Transplant. 2009; 24:3694–701.
Article22. Brown DD, Reidy KJ. Approach to the child with hematuria. Pediatr Clin North Am. 2019; 66:15–30.
Article23. Lava SA, Bianchetti MG, Simonetti GD. Salt intake in children and its consequences on blood pressure. Pediatr Nephrol. 2015; 30:1389–96.
Article24. He FJ, Marrero NM, Macgregor GA. Salt and blood pressure in children and adolescents. J Hum Hypertens. 2008; 22:4–11.
Article25. Levin A, Stevens PE, Bilous RW, Coresh J, De Francisco AL, De Jong PE, et al. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013; 3:1–150.26. Chaturvedi S, Jones C. Protein restriction for children with chronic renal failure. Cochrane Database Syst Rev. 2007; (4):CD006863.27. Uauy RD, Hogg RJ, Brewer ED, Reisch JS, Cunningham C, Holliday MA. Dietary protein and growth in infants with chronic renal insufficiency: a report from the Southwest Pediatric Nephrology Study Group and the University of California, San Francisco. Pediatr Nephrol. 1994; 8:45–50.
Article