Child Kidney Dis.
2023 Jun;27(1):19-25. 10.3339/ckd.23.003.
CUBN mutation: a benign genetic cause of proteinuria?
- Affiliations
-
- 1Department of Pediatrics, Kangwon National University Hospital, Chuncheon, Republic of Korea
- KMID: 2544233
- DOI: http://doi.org/10.3339/ckd.23.003
Abstract
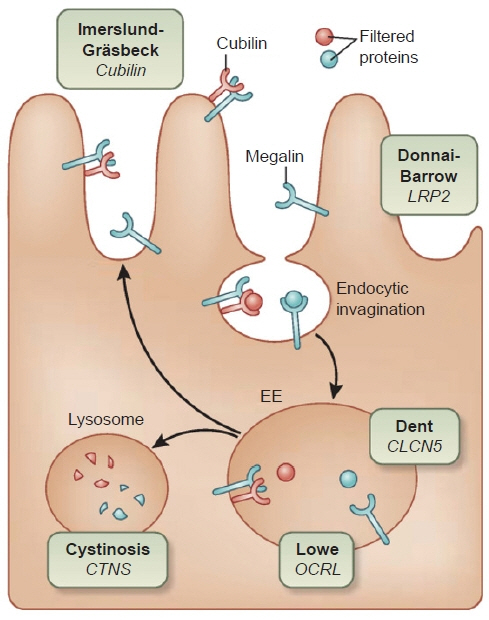
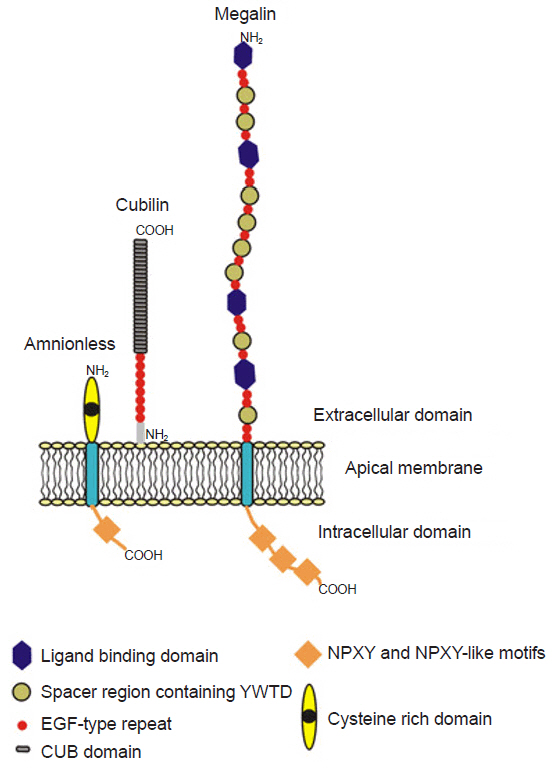
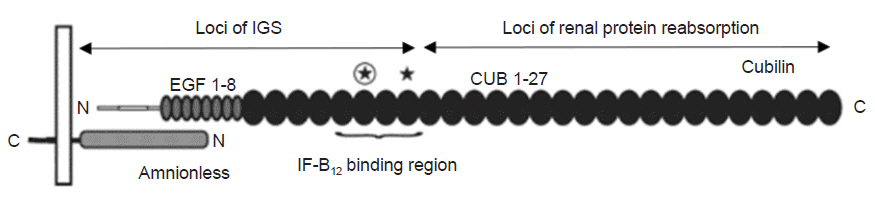
- Proteinuria is an important risk factor for renal and cardiovascular disease. It is associated with a risk for glomerulonephritis, chronic kidney disease, and end-stage renal disease. Therefore, if persistent proteinuria is detected, kidney biopsy is considered to diagnose and treat the underlying disease. Recently, variants in the cubilin gene (CUBN), which is associated with albuminuria, have been reported. This gene encodes cubilin, a membrane glycoprotein receptor expressed in the renal proximal tubules. Cubilin is a component of the megalin and cubilin-amnionless complex that mediates albumin reabsorption into the proximal tubules through endocytosis. A defect in cubilin leads to a reduction in albumin reuptake, resulting in albumin-dominant proteinuria. Although numerous controversies exist, several reports suggest that cubilin defects lead to proteinuria with a high portion of albuminuria but may not impair renal filtration function. If albuminuria due to reduced cubilin function is confirmed as a benign condition, we can consider using genetic studies to detect CUBN mutations in patients with proteinuria and they may not require any treatment or kidney biopsy. Here, we review recent papers on CUBN mutations and discuss the prognosis and management of individuals with this mutation.
Keyword
Figure
Reference
-
References
1. Gburek J, Konopska B, Golab K. Renal handling of albumin-from early findings to current concepts. Int J Mol Sci. 2021; 22:5809.
Article2. Gekle M. Renal tubule albumin transport. Annu Rev Physiol. 2005; 67:573–94.
Article3. Dickson LE, Wagner MC, Sandoval RM, Molitoris BA. The proximal tubule and albuminuria: really! J Am Soc Nephrol. 2014; 25:443–53.4. Figueroa SM, Araos P, Reyes J, Gravez B, Barrera-Chimal J, Amador CA. Oxidized albumin as a mediator of kidney disease. Antioxidants (Basel). 2021; 10:404.
Article5. Nielsen R, Christensen EI, Birn H. Megalin and cubilin in proximal tubule protein reabsorption: from experimental models to human disease. Kidney Int. 2016; 89:58–67.
Article6. Willnow TE. Nanotubes, the fast track to treatment of Dent disease? Kidney Int. 2017; 91:776–8.
Article7. Christensen EI, Willnow TE. Essential role of megalin in renal proximal tubule for vitamin homeostasis. J Am Soc Nephrol. 1999; 10:2224–36.
Article8. Khalifa O, Al-Sahlawi Z, Imtiaz F, Ramzan K, Allam R, Al-Mostafa A, et al. Variable expression pattern in Donnai-Barrow syndrome: report of two novel LRP2 mutations and review of the literature. Eur J Med Genet. 2015; 58:293–9.
Article9. Simons M. The benefits of tubular proteinuria: an evolutionary perspective. J Am Soc Nephrol. 2018; 29:710–2.
Article10. Storm T, Zeitz C, Cases O, Amsellem S, Verroust PJ, Madsen M, et al. Detailed investigations of proximal tubular function in Imerslund-Gräsbeck syndrome. BMC Med Genet. 2013; 14:111.11. Christensen EI, Devuyst O, Dom G, Nielsen R, Van der Smissen P, Verroust P, et al. Loss of chloride channel ClC-5 impairs endocytosis by defective trafficking of megalin and cubilin in kidney proximal tubules. Proc Natl Acad Sci U S A. 2003; 100:8472–7.
Article12. Birn H, Fyfe JC, Jacobsen C, Mounier F, Verroust PJ, Orskov H, et al. Cubilin is an albumin binding protein important for renal tubular albumin reabsorption. J Clin Invest. 2000; 105:1353–61.
Article13. Aminoff M, Carter JE, Chadwick RB, Johnson C, Grasbeck R, Abdelaal MA, et al. Mutations in CUBN, encoding the intrinsic factor-vitamin B12 receptor, cubilin, cause hereditary megaloblastic anaemia 1. Nat Genet. 1999; 21:309–13.
Article14. Grasbeck R. Imerslund-Gräsbeck syndrome (selective vitamin B(12) malabsorption with proteinuria). Orphanet J Rare Dis. 2006; 1:17.
Article15. Storm T, Emma F, Verroust PJ, Hertz JM, Nielsen R, Christensen EI. A patient with cubilin deficiency. N Engl J Med. 2011; 364:89–91.
Article16. Ovunc B, Otto EA, Vega-Warner V, Saisawat P, Ashraf S, Ramaswami G, et al. Exome sequencing reveals cubilin mutation as a single-gene cause of proteinuria. J Am Soc Nephrol. 2011; 22:1815–20.
Article17. Boger CA, Chen MH, Tin A, Olden M, Kottgen A, de Boer IH, et al. CUBN is a gene locus for albuminuria. J Am Soc Nephrol. 2011; 22:555–70.18. Sadowski CE, Lovric S, Ashraf S, Pabst WL, Gee HY, Kohl S, et al. A single-gene cause in 29.5% of cases of steroid-resistant nephrotic syndrome. J Am Soc Nephrol. 2015; 26:1279–89.
Article19. Schapiro D, Daga A, Lawson JA, Majmundar AJ, Lovric S, Tan W, et al. Panel sequencing distinguishes monogenic forms of nephritis from nephrosis in children. Nephrol Dial Transplant. 2019; 34:474–85.
Article20. Nagano C, Yamamura T, Horinouchi T, Aoto Y, Ishiko S, Sakakibara N, et al. Comprehensive genetic diagnosis of Japanese patients with severe proteinuria. Sci Rep. 2020; 10:270.
Article21. Bedin M, Boyer O, Servais A, Li Y, Villoing-Gaude L, Tete MJ, et al. Human C-terminal CUBN variants associate with chronic proteinuria and normal renal function. J Clin Invest. 2020; 130:335–44.
Article22. Domingo-Gallego A, Pybus M, Madariaga L, Pinero-Fernandez JA, Gonzalez-Pastor S, Lopez-Gonzalez M, et al. Clinical and genetic characterization of a cohort of proteinuric patients with biallelic CUBN variants. Nephrol Dial Transplant. 2022; 37:1906–15.23. Cicek N, Alpay H, Guven S, Alavanda C, Turkkan ON, Pul S, et al. Clinical and genetic characterization of children with cubilin variants. Pediatr Nephrol. 2023; 38:1381–5.
Article24. Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016; 536:285–91.
Article25. Yang J, Xu Y, Deng L, Zhou L, Qiu L, Zhang Y, et al. CUBN gene mutations may cause focal segmental glomerulosclerosis (FSGS) in children. BMC Nephrol. 2022; 23:15.
Article26. Jayasinghe K, White SM, Kerr PG, MacGregor D, Stark Z, Wilkins E, et al. Isolated proteinuria due to CUBN homozygous mutation: challenging the investigative paradigm. BMC Nephrol. 2019; 20:330.27. Gan C, Zhou X, Chen D, Chi H, Qiu J, You H, et al. Novel pathogenic variants in CUBN uncouple proteinuria from renal function. J Transl Med. 2022; 20:480.
Article28. Prabakaran T, Christensen EI, Nielsen R, Verroust PJ. Cubilin is expressed in rat and human glomerular podocytes. Nephrol Dial Transplant. 2012; 27:3156–9.
Article29. Gianesello L, Priante G, Ceol M, Radu CM, Saleem MA, Simioni P, et al. Albumin uptake in human podocytes: a possible role for the cubilin-amnionless (CUBAM) complex. Sci Rep. 2017; 7:13705.30. Christensen EI, Birn H, Storm T, Weyer K, Nielsen R. Endocytic receptors in the renal proximal tubule. Physiology (Bethesda). 2012; 27:223–36.
Article31. Santer R, Calado J. Familial renal glucosuria and SGLT2: from a mendelian trait to a therapeutic target. Clin J Am Soc Nephrol. 2010; 5:133–41.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Genetic analysis using whole-exome sequencing in pediatric chronic kidney disease: a single center's experience
- Clinical Approach to Children with Proteinuria
- A Case of Nutcracker Syndrome Presenting with Orthostatic Proteinuria
- Two Cases of Oculocerebrorenal Syndrome in Two Brothers Diagnosed after Congenital Cataract Surgery
- Clinical Features of Genetic Creutzfeldt-Jakob Disease with E200K Mutation