J Korean Med Sci.
2023 Jun;38(24):e197. 10.3346/jkms.2023.38.e197.
Current Status of Q Fever and the Challenge of Outbreak Preparedness in Korea: One Health Approach to Zoonoses
- Affiliations
-
- 1Laboratory of Parasitic and Honeybee Diseases, Bacterial Disease Division, Department of Animal and Plant Health Research, Animal and Plant Quarantine Agency, Gimcheon, Korea
- 2Department of Preventive Medicine, College of Medicine, Dongguk University, Gyeongju, Korea
- 3Research Planning Division, Department of Animal and Plant Health Research, Animal and Plant Quarantine Agency, Gimcheon, Korea
- 4World Organization for Animal Health (WOAH) Reference Laboratory for Brucellosis, Bacterial Disease Division, Department of Animal and Plant Health Research, Animal and Plant Quarantine Agency, Gimcheon, Korea
- 5Chungcheongbuk-do Institute of Veterinary Service and Research, Cheongju, Korea
- 6Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea
- 7Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Korea
- 8Division of Infectious Diseases, Department of Internal Medicine, Chosun University College of Medicine, Gwangju, Korea
- 9Division of Infectious Diseases, Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Cheonan, Korea
- 10College of Veterinary Medicine & Institute of Veterinary Science, Kangwon National University, Chuncheon, Gangwon, Korea
- 11Division of Veterinary Parasitology, College of Veterinary Medicine, Kyungpook National University, Daegu, Korea
- 12Department of Infectious Diseases, College of Veterinary Medicine, Seoul National University, Seoul, Korea
- 13Division of Zoonotic and Vector Borne Disease Control, Bureau of Infectious Disease Policy, Korea Disease Control and Prevention Agency, Cheongju, Korea
- 14Department of Infectious Diseases, Ajou University School of Medicine, Suwon, Korea
- KMID: 2543977
- DOI: http://doi.org/10.3346/jkms.2023.38.e197
Abstract
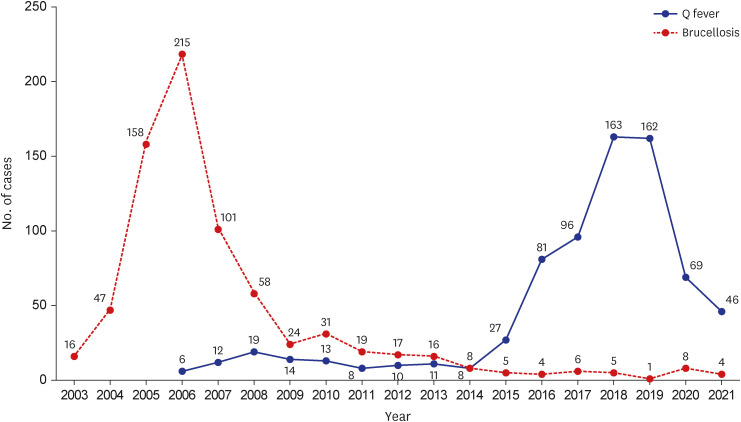
- Human Q fever, a zoonosis caused by Coxiella burnetii, presents with diverse clinical manifestations ranging from mild self-limited febrile illnesses to life-threatening complications such as endocarditis or vascular infection. Although acute Q fever is a benign illness with a low mortality rate, a large-scale outbreak of Q fever in the Netherlands led to concerns about the possibility of blood transfusion-related transmission or obstetric complications in pregnant women. Furthermore, a small minority (< 5%) of patients with asymptomatic or symptomatic infection progress to chronic Q fever. Chronic Q fever is fatal in 5–50% of patients if left untreated. In South Korea, Q fever in humans was designated as a notifiable infectious disease in 2006, and the number of Q fever cases has increased sharply since 2015. Nonetheless, it is still considered a neglected and under-recognized infectious disease. In this review, recent trends of human and animal Q fever in South Korea, and public health concerns regarding Q fever outbreaks are reviewed, and we consider how a One Health approach could be applied as a preventive measure to prepare for zoonotic Q fever outbreaks.
Keyword
Figure
Reference
-
1. Stein A, Raoult D. Pigeon pneumonia in provence: a bird-borne Q fever outbreak. Clin Infect Dis. 1999; 29(3):617–620. PMID: 10530457.2. Buhariwalla F, Cann B, Marrie TJ. A dog-related outbreak of Q fever. Clin Infect Dis. 1996; 23(4):753–755. PMID: 8909839.3. Beaman MH, Hung J. Pericarditis associated with tick-borne Q fever. Aust N Z J Med. 1989; 19(3):254–256. PMID: 2775046.4. Langley JM, Marrie TJ, Covert A, Waag DM, Williams JC. Poker players’ pneumonia. An urban outbreak of Q fever following exposure to a parturient cat. N Engl J Med. 1988; 319(6):354–356. PMID: 3393197.5. Marrie TJ, Schlech WF 3rd, Williams JC, Yates L. Q fever pneumonia associated with exposure to wild rabbits. Lancet. 1986; 327(8478):427–429.6. van der Hoek W, Dijkstra F, Schimmer B, Schneeberger PM, Vellema P, Wijkmans C, et al. Q fever in the Netherlands: an update on the epidemiology and control measures. Euro Surveill. 2010; 15(12):19520. PMID: 20350500.7. Schimmer B, Ter Schegget R, Wegdam M, Züchner L, de Bruin A, Schneeberger PM, et al. The use of a geographic information system to identify a dairy goat farm as the most likely source of an urban Q-fever outbreak. BMC Infect Dis. 2010; 10(1):69. PMID: 20230650.8. Racult D, Stein A. Q fever during pregnancy--a risk for women, fetuses, and obstetricians. N Engl J Med. 1994; 330(5):371.9. Kanfer E, Farrag N, Price C, MacDonald D, Coleman J, Barrett AJ. Q fever following bone marrow transplantation. Bone Marrow Transplant. 1988; 3(2):165–166. PMID: 3048481.10. Bamberg WM, Pape WJ, Beebe JL, Nevin-Woods C, Ray W, Maguire H, et al. Outbreak of Q fever associated with a horse-boarding ranch, Colorado, 2005. Vector Borne Zoonotic Dis. 2007; 7(3):394–402. PMID: 17896873.11. Maurin M, Raoult D. Q fever. Clin Microbiol Rev. 1999; 12(4):518–553. PMID: 10515901.12. Fenollar F, Fournier PE, Carrieri MP, Habib G, Messana T, Raoult D. Risks factors and prevention of Q fever endocarditis. Clin Infect Dis. 2001; 33(3):312–316. PMID: 11438895.13. Eldin C, Mélenotte C, Mediannikov O, Ghigo E, Million M, Edouard S, et al. From Q fever to Coxiella burnetii infection: a paradigm change. Clin Microbiol Rev. 2017; 30(1):115–190. PMID: 27856520.14. World Organisation for Animal Health. Q fever. OIE terrestrial manual. Updated 2018. Accessed February 9, 2023. https://www.woah.org/fileadmin/Home/eng/Health_standards/tahm/3.01.16_Q_FEVER.pdf .15. Korea Disease Control and Prevention Agency. Statistics for infectious disease, 2006-2023, group III: Q fever. Updated 2023. Accessed February 9, 2023. https://www.kdca.go.kr/npt/biz/npp/ist/bass/bassDissStatsMain.do .16. Kim YC, Jeong HW, Kim DM, Huh K, Choi SH, Lee HY, et al. Epidemiological investigation and physician awareness regarding the diagnosis and management of Q fever in South Korea, 2011 to 2017. PLoS Negl Trop Dis. 2021; 15(6):e0009467. PMID: 34077423.17. Heo JY, Lee HY, Jeong HW, Choi YH, Kim DM, Choi SH, et al. A comprehensive analysis of clinical and epidemiological characteristics in Korean Q fever patients for better management. Report No. RP00004303. Updated 2019. Accessed February 9, 2023. https://library.nih.go.kr/ncmiklib/archive/rom/reportView.do?upd_yn=Y&rep_id=RP00004303 .18. Acharya D, Park JH, Chun JH, Kim MY, Yoo SJ, Lewin A, et al. Seroepidemiologic evidence of Q fever and associated factors among workers in veterinary service laboratory in South Korea. PLoS Negl Trop Dis. 2022; 16(2):e0010054. PMID: 35108271.19. Park JH, Lee K, Yoo SJ, Jeong EY. Epidemiological ans serological studies on Q fever and brucellosis in the high-risk population, 2019. Report No. RP00011917. Updated 2019. Accessed February 9, 2023. https://library.nih.go.kr/ncmiklib/archive/rom/reportView.do?upd_yn=Y&rep_id=RP00011917 .20. Kim M, Yi H, Chun JH, Hwang KJ. Survey of sero-prevalence to coxiellosis among high risk groups of Q-fever in South Korea, 2007-2019. Public Health Wkly Rep. 2020; 13(33):2467–2477.21. Song J, Lee HS, Lee JY, Shin S, Kwon GY, Kim M, et al. Seroprevalence of Q fever in goat farm workers in the Republic of Korea, 2020. Public Health Wkly Rep. 2021; 14(44):3111–3119.22. Korea Animal Health Integrated System. Statistics for livestock communicable diseases. Updated 2023. Accessed February 9, 2023. https://home.kahis.go.kr/home/lkntscrinfo/selectLkntsOccrrnc.do .23. Na HM, Bae SY, Koh BR, Park JS, Seo YJ, Jeong H, et al. Prevalence of antibody titers for Coxiella burnetii in cattle in Gwangju area, Korea. Korean J Vet Serv. 2016; 39(2):125–129.24. Gang SJ, Jeong JM, Kim HK, Lee JW, Shon K, Park TW. Prevalence of Coxiella burnetii in native Korean goat in Jeonbuk province. Korean J Vet Serv. 2016; 39(4):239–246.25. Kim SG, Cho JC, Lee MG, Kim SS, Lee SH, Kwak DM. Seroprevalence of Coxiella burnetii in native Korean goats (Capra hircus coreanae) in Gyeongbuk province, Korea. Korean J Vet Serv. 2014; 37(4):241–246.26. Ouh IO, Seo MG, Do JC, Kim IK, Cho MH, Kwak DM. Seroprevalence of Coxiella burnetii in bulk-tank milk and dairy cattle in Gyeongbuk province, Korea. Korean J Vet Serv. 2013; 36(4):243–248.27. Anderson A, Bijlmer H, Fournier PE, Graves S, Hartzell J, Kersh GJ, et al. Diagnosis and management of Q fever--United States, 2013: recommendations from CDC and the Q Fever Working Group. MMWR Recomm Rep. 2013; 62:1–30.28. van Loenhout JA, Paget WJ, Vercoulen JH, Wijkmans CJ, Hautvast JL, van der Velden K. Assessing the long-term health impact of Q-fever in the Netherlands: a prospective cohort study started in 2007 on the largest documented Q-fever outbreak to date. BMC Infect Dis. 2012; 12(1):280. PMID: 23110336.29. Roest HI, Tilburg JJ, van der Hoek W, Vellema P, van Zijderveld FG, Klaassen CH, et al. The Q fever epidemic in The Netherlands: history, onset, response and reflection. Epidemiol Infect. 2011; 139(1):1–12. PMID: 20920383.30. Koopmans C, Tempelman C, Prins J. Economic consequences of the Q fever outbreak. Updated 2011. Accessed February 9, 2023. https://www.seo.nl/en/publications/economic-consequences-of-the-q-fever-outbreak/#:~:text=The%20total%20damage%20is%20estimated,some%2067%2D145%20million%20euros .31. van der Hoek W, Hogema BM, Dijkstra F, Rietveld A, Wijkmans CJ, Schneeberger PM, et al. Relation between Q fever notifications and Coxiella burnetii infections during the 2009 outbreak in The Netherlands. Euro Surveill. 2012; 17(3):20058. PMID: 22297100.32. Oei W, Kretzschmar ME, Zaaijer HL, Coutinho R, van der Poel CL, Janssen MP. Estimating the transfusion transmission risk of Q fever. Transfusion. 2014; 54(7):1705–1711. PMID: 24456030.33. Kampschreur LM, Delsing CE, Groenwold RH, Wegdam-Blans MC, Bleeker-Rovers CP, de Jager-Leclercq MG, et al. Chronic Q fever in the Netherlands 5 years after the start of the Q fever epidemic: results from the Dutch chronic Q fever database. J Clin Microbiol. 2014; 52(5):1637–1643. PMID: 24599987.34. Million M, Thuny F, Richet H, Raoult D. Long-term outcome of Q fever endocarditis: a 26-year personal survey. Lancet Infect Dis. 2010; 10(8):527–535. PMID: 20637694.35. Botelho-Nevers E, Fournier PE, Richet H, Fenollar F, Lepidi H, Foucault C, et al. Coxiella burnetii infection of aortic aneurysms or vascular grafts: report of 30 new cases and evaluation of outcome. Eur J Clin Microbiol Infect Dis. 2007; 26(9):635–640. PMID: 17629755.36. Million M, Roblot F, Carles D, D’Amato F, Protopopescu C, Carrieri MP, et al. Reevaluation of the risk of fetal death and malformation after Q Fever. Clin Infect Dis. 2014; 59(2):256–260. PMID: 24748522.37. Munster JM, Leenders AC, Hamilton CJ, Meekelenkamp JC, Schneeberger PM, van der Hoek W, et al. Routine screening for Coxiella burnetii infection during pregnancy: a clustered randomised controlled trial during an outbreak, the Netherlands, 2010. Euro Surveill. 2013; 18(24):20504. PMID: 23787163.38. Quijada SG, Terán BM, Murias PS, Anitua AA, Cermeño JL, Frías AB. Q fever and spontaneous abortion. Clin Microbiol Infect. 2012; 18(6):533–538. PMID: 22471505.39. Carcopino X, Raoult D, Bretelle F, Boubli L, Stein A. Managing Q fever during pregnancy: the benefits of long-term cotrimoxazole therapy. Clin Infect Dis. 2007; 45(5):548–555. PMID: 17682987.40. Park MY, Lee CS, Choi YS, Park SJ, Lee JS, Lee HB. A sporadic outbreak of human brucellosis in Korea. J Korean Med Sci. 2005; 20(6):941–946. PMID: 16361801.41. Lim JS, Min KD, Ryu S, Hwang SS, Cho SI. Spatial analysis to assess the relationship between human and bovine brucellosis in South Korea, 2005-2010. Sci Rep. 2019; 9(1):6657. PMID: 31040303.42. Lee BY, Higgins IM, Moon OK, Clegg TA, McGrath G, Collins DM, et al. Surveillance and control of bovine brucellosis in the Republic of Korea during 2000-2006. Prev Vet Med. 2009; 90(1-2):66–79. PMID: 19361875.43. Yoon H, Moon OK, Her M, Carpenter TE, Kim YJ, Jung S, et al. Impact of bovine brucellosis eradication programs in the Republic of Korea. Prev Vet Med. 2010; 95(3-4):288–291. PMID: 20493568.44. Ryu S, Soares Magalhães RJ, Chun BC. The impact of expanded brucellosis surveillance in beef cattle on human brucellosis in Korea: an interrupted time-series analysis. BMC Infect Dis. 2019; 19(1):201. PMID: 30819243.45. Animal and Plant Quarantine Agency (KR). Control measures for animal Q fever. Updated 2017. Accessed February 9, 2023. https://www.qia.go.kr/viewwebQiaCom.do?id=41348&type=2_3fyxx .46. Byeon HS, Han MN, Han ST, Chae MH, Kang SS, Jang RH, et al. Massive human Q fever outbreak from a goat farm in Korea. J Biomed Transl Res. 2020; 21(4):200–206.47. Kersh GJ, Wolfe TM, Fitzpatrick KA, Candee AJ, Oliver LD, Patterson NE, et al. Presence of Coxiella burnetii DNA in the environment of the United States, 2006 to 2008. Appl Environ Microbiol. 2010; 76(13):4469–4475. PMID: 20472727.48. Angelakis E, Raoult D. Q fever. Vet Microbiol. 2010; 140(3-4):297–309. PMID: 19875249.49. Enright JB, Sadler WW, Thomas RC. Pasteurization of milk containing the organism of Q fever. Am J Public Health Nations Health. 1957; 47(6):695–700. PMID: 13424814.50. Stephen S, Rao KN. Coxiellosis in reptiles of South Kanara district, Karnataka. Indian J Med Res. 1979; 70:937–941. PMID: 541017.51. Centers for Disease Control and Prevention (CDC). Bioterrorism agents/diseases. Updated 2018. Accessed February 9, 2023. https://emergency.cdc.gov/agent/agentlist-category.asp .52. McDermott J, Grace D, Zinsstag J. Economics of brucellosis impact and control in low-income countries. Rev Sci Tech. 2013; 32(1):249–261. PMID: 23837382.53. International Livestock Research Institute. Mapping of poverty and likely zoonoses hotspots. Zoonoses Project 4. Report to Department for International Development, UK. Updated 2012. Accessed February 9, 2023. https://assets.publishing.service.gov.uk/media/57a08a63ed915d622c0006fd/ZooMapDFIDreport18June2012FINALsm.pdf .54. de Cremoux R, Rousset E, Touratier A, Audusseau G, Nicollet P, Ribaud D, et al. Coxiella burnetii vaginal shedding and antibody responses in dairy goat herds in a context of clinical Q fever outbreaks. FEMS Immunol Med Microbiol. 2012; 64(1):120–122. PMID: 22066517.55. Guatteo R, Beaudeau F, Joly A, Seegers H. Coxiella burnetii shedding by dairy cows. Vet Res. 2007; 38(6):849–860. PMID: 17903418.56. Rousset E, Berri M, Durand B, Dufour P, Prigent M, Delcroix T, et al. Coxiella burnetii shedding routes and antibody response after outbreaks of Q fever-induced abortion in dairy goat herds. Appl Environ Microbiol. 2009; 75(2):428–433. PMID: 19011054.57. Schimmer B, Dijkstra F, Vellema P, Schneeberger PM, Hackert V, ter Schegget R, et al. Sustained intensive transmission of Q fever in the south of the Netherlands, 2009. Euro Surveill. 2009; 14(19):19210. PMID: 19442401.58. Van den Brom R, Vellema P. Q fever outbreaks in small ruminants and people in the Netherlands. Small Rumin Res. 2009; 86(1-3):74–79.59. Anderson A, Boyer T, Garvey A, Marshall K, Menzies P, Murphy J, et al. Prevention and control of Coxiella burnetii infection among humans and animals: guidance for a coordinated public health and animal health response, 2013. Updated 2013. Accessed February 9, 2023. http://www.nasphv.org/Documents/Q_Fever_2013.pdf .60. Bond KA, Vincent G, Wilks CR, Franklin L, Sutton B, Stenos J, et al. One Health approach to controlling a Q fever outbreak on an Australian goat farm. Epidemiol Infect. 2016; 144(6):1129–1141. PMID: 26493615.61. Van den Brom R, van Engelen E, Roest HI, van der Hoek W, Vellema P. Coxiella burnetii infections in sheep or goats: an opinionated review. Vet Microbiol. 2015; 181(1-2):119–129. PMID: 26315774.62. Heo JY, Choi YW, Kim EJ, Lee SH, Lim SK, Hwang SD, et al. Clinical characteristics of acute Q fever patients in South Korea and time from symptom onset to serologic diagnosis. BMC Infect Dis. 2019; 19(1):903. PMID: 31660875.63. Fournier PE, Marrie TJ, Raoult D. Diagnosis of Q fever. J Clin Microbiol. 1998; 36(7):1823–1834. PMID: 9650920.64. Fournier PE, Raoult D. Comparison of PCR and serology assays for early diagnosis of acute Q fever. J Clin Microbiol. 2003; 41(11):5094–5098. PMID: 14605144.65. Schneeberger PM, Hermans MH, van Hannen EJ, Schellekens JJ, Leenders AC, Wever PC. Real-time PCR with serum samples is indispensable for early diagnosis of acute Q fever. Clin Vaccine Immunol. 2010; 17(2):286–290. PMID: 20032219.66. European Medicines Agency. Coevac: inactivated coxiella burnetii vaccine. Updated 2020. Accessed February 9, 2023. https://www.ema.europa.eu/en/medicines/veterinary/EPAR/coxevac .67. Arricau-Bouvery N, Souriau A, Bodier C, Dufour P, Rousset E, Rodolakis A. Effect of vaccination with phase I and phase II Coxiella burnetii vaccines in pregnant goats. Vaccine. 2005; 23(35):4392–4402. PMID: 16005747.68. Hogerwerf L, van den Brom R, Roest HI, Bouma A, Vellema P, Pieterse M, et al. Reduction of Coxiella burnetii prevalence by vaccination of goats and sheep, The Netherlands. Emerg Infect Dis. 2011; 17(3):379–386. PMID: 21392427.69. Lepidi H, Houpikian P, Liang Z, Raoult D. Cardiac valves in patients with Q fever endocarditis: microbiological, molecular, and histologic studies. J Infect Dis. 2003; 187(7):1097–1106. PMID: 12660924.70. Fournier PE, Thuny F, Richet H, Lepidi H, Casalta JP, Arzouni JP, et al. Comprehensive diagnostic strategy for blood culture-negative endocarditis: a prospective study of 819 new cases. Clin Infect Dis. 2010; 51(2):131–140. PMID: 20540619.71. Kampschreur LM, Oosterheert JJ, Koop AM, Wegdam-Blans MC, Delsing CE, Bleeker-Rovers CP, et al. Microbiological challenges in the diagnosis of chronic Q fever. Clin Vaccine Immunol. 2012; 19(5):787–790. PMID: 22441385.72. Kampschreur LM, Wegdam-Blans MC, Wever PC, Renders NH, Delsing CE, Sprong T, et al. Chronic Q fever diagnosis—consensus guideline versus expert opinion. Emerg Infect Dis. 2015; 21(7):1183–1188. PMID: 26277798.73. Wielders CC, van Loenhout JA, Morroy G, Rietveld A, Notermans DW, Wever PC, et al. Long-term serological follow-up of acute Q-fever patients after a large epidemic. PLoS One. 2015; 10(7):e0131848. PMID: 26161658.74. Korea Center for Disease Control and Prevention Agency. Seroprevalence survey and development of preventive guideline of Q fever among high risk groups. Updated 2022. Accessed February 9, 2023. https://www.prism.go.kr/homepage/entire/researchDetail.do?researchId=1790387-202100132&menuNo=I0000002 .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Healthcare reform after MERS outbreak: progress to date and next steps
- Current Status and Issues in Zoonoses Control
- What do we really fear? The epidemiological characteristics of Ebola and our preparedness
- A Case Report of Human Brucellosis Found by Zoonoses Surveillance System Based on One Health
- Awareness of Zoonoses among Cattle Slaughterhouse Workers in Korea