J Korean Med Sci.
2023 Jun;38(24):e182. 10.3346/jkms.2023.38.e182.
Ethical Issues Referred to Clinical Ethics Support at a University Hospital in Korea: Three-Year Experience After Enforcement of LifeSustaining Treatment Decisions Act
- Affiliations
-
- 1Center for Palliative Care and Clinical Ethics, Seoul National University Hospital, Seoul, Korea
- 2Public Healthcare Center, Seoul National University Hospital, Seoul, Korea
- 3Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Psychiatry, Seoul National University College of Medicine, Seoul, Korea
- 5Division of Hematology and Medical Oncology, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 6Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2543973
- DOI: http://doi.org/10.3346/jkms.2023.38.e182
Abstract
- Background
Clinical ethics support is a form of preventive ethics aimed at mediating ethicsrelated conflicts and managing ethical issues arising in the healthcare setting. However, limited evidence exists regarding the specific ethical issues in clinical practice. This study aimed to explore the diverse ethical issues of cases referred to clinical ethics support after the new legislation on hospice palliative care and end-of-life decision-making was implemented in Korea in 2018.
Methods
A retrospective study of cases referred to clinical ethics support at a university hospital in Korea from February 2018 to February 2021 was conducted. The ethical issues at the time of referral were analyzed via qualitative content analysis of the ethics consultationrelated documents.
Results
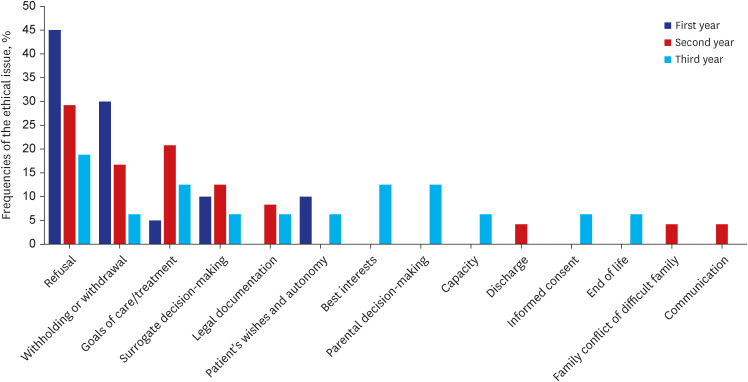
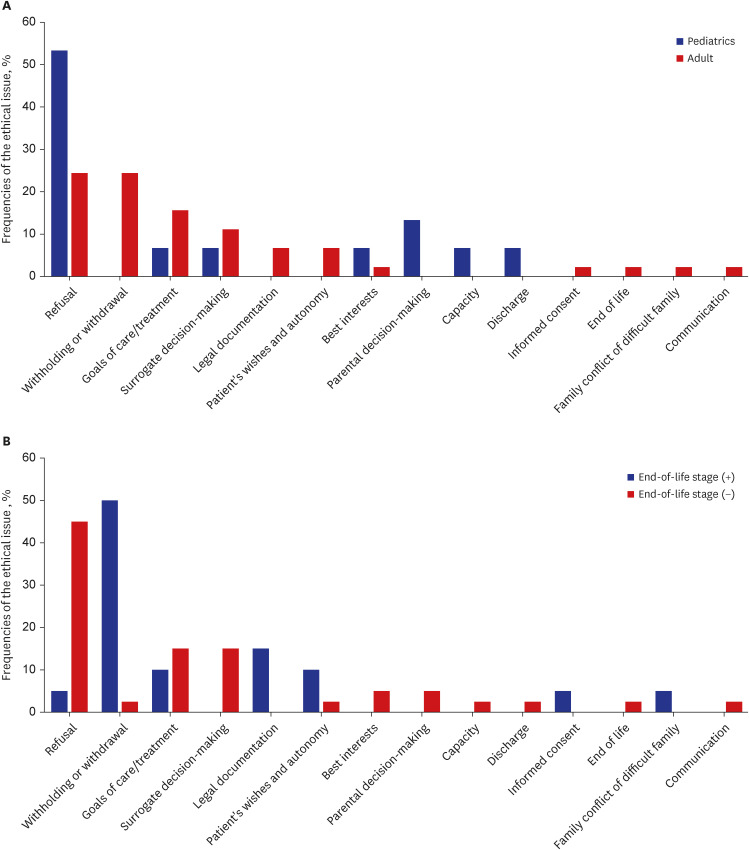
A total of 60 cases of 57 patients were included in the study, of whom 52.6% were men and 56.1% were older than 60 years of age. The majority of cases (80%) comprised patients from the intensive care unit. One-third of the patients were judged as being at the end-of-life stage. The most frequent ethical categories were identified as goals of care/ treatment (78.3%), decision-making (75%), relationship (41.7%), and end-of-life issues (31.7%). More specifically, best interests (71.7%), benefits and burdens/harms (61.7%), refusal (53.3%), and surrogate decision-making (33.3%), followed by withholding or withdrawal (28.3%) were the most frequent ethical issues reported, which became diversified by year. In addition, the ethical issues appeared to differ by age group and judgment of the end-of-life stage.
Conclusion
The findings of this study expand the current understanding of the diverse ethical issues including decision-making and goals of care/treatment that have been referred to clinical ethics support since the enforcement of the new legislation in Korea. This study suggests a need for further research on the longitudinal exploration of ethical issues and implementation of clinical ethics support in multiple healthcare centers.
Keyword
Figure
Reference
-
1. Fuscaldo G, Cadwell M, Wallis K, Fry L, Rogers M. Developing clinical ethics support for an Australian Health Service: a survey of clinician’s experiences and views. AJOB Empir Bioeth. 2019; 10(1):44–54. PMID: 30908109.2. Jansky M, Marx G, Nauck F, Alt-Epping B. Physicians’ and nurses’ expectations and objections toward a clinical ethics committee. Nurs Ethics. 2013; 20(7):771–783. PMID: 23715555.3. Fox E, Myers S, Pearlman RA. Ethics consultation in United States hospitals: a national survey. Am J Bioeth. 2007; 7(2):13–25.4. Slowther A, Bunch C, Woolnough B, Hope T. Clinical ethics support services in the UK: an investigation of the current provision of ethics support to health professionals in the UK. J Med Ethics. 2001; 27:Suppl 1. (Suppl 1):i2–i8. PMID: 11314606.5. Rasoal D, Skovdahl K, Gifford M, Kihlgren A. Clinical ethics support for healthcare personnel: an integrative literature review. HEC Forum. 2017; 29(4):313–346. PMID: 28600658.6. Wasson K, Anderson E, Hagstrom E, McCarthy M, Parsi K, Kuczewski M. What ethical issues really arise in practice at an academic medical center? A quantitative and qualitative analysis of clinical ethics consultations from 2008 to 2013. HEC Forum. 2016; 28(3):217–228. PMID: 26423767.7. Ministry of Health and Welfare. Act on Hospice and Palliative Care and Decisions on Life-sustaining Treatment for Patients at the End of Life. Updated 2022. Accessed August 22, 2022. https://www.law.go.kr/%EB%B2%95%EB%A0%B9/%ED%98%B8%EC%8A%A4%ED%94%BC%EC%8A%A4%E3%86%8D%EC%99%84%ED%99%94%EC%9D%98%EB%A3%8C%EB%B0%8F%EC%9E%84%EC%A2%85%EA%B3%BC%EC%A0%95%EC%97%90%EC%9E%88%EB%8A%94%ED%99%98%EC%9E%90%EC%9D%98%EC%97%B0%EB%AA%85%EC%9D%98%EB%A3%8C%EA%B2%B0%EC%A0%95%EC%97%90%EA%B4%80%ED%95%9C%EB%B2%95%EB%A5%A0 .8. Lee I. Perspective on patient end-of-life decision act and clinical ethics service. J Korean Bioethics Assoc. 2017; 18(1):35–45.9. Choi K. Clinical ethics consultation and hospital ethics committees. Korean J Med Ethics. 2017; 20(4):359–375.10. Park SH, Koh Y. Attitudes toward medical ethics among resident physicians in one Korean university hospital. Korean J Med Ethics. 2007; 10(2):109–116.11. Kim MS, Kim CH, Hong J, An AR, Choi EK, Keam B, et al. A survey of the ethical problems faced by healthcare professionals and the need for clinical ethics consultation services in university hospitals in South Korea. Korean J Med Ethics. 2017; 20(3):376–385.12. Yoo SH, Choi W, Kim Y, Kim MS, Park HY, Keam B, et al. Difficulties doctors experience during life-sustaining treatment discussion after enactment of the Life-Sustaining Treatment Decisions Act: a cross-sectional study. Cancer Res Treat. 2021; 53(2):584–592. PMID: 33211941.13. Heo DS, Park HY, Hong J, Lee J, Keam B. The roles of hospital ethics committee and clinical ethics consultation teams. Korean J Med Ethics. 2017; 20(4):353–358.14. Milliken A, Courtwright A, Grace P, Eagan-Bengston E, Visser M, Jurchak M. Ethics consultations at a major academic medical center: a retrospective, longitudinal analysis. AJOB Empir Bioeth. 2020; 11(4):275–286. PMID: 32940565.15. Thomas SM, Ford PJ, Weise KL, Worley S, Kodish E. Not just little adults: a review of 102 paediatric ethics consultations. Acta Paediatr. 2015; 104(5):529–534. PMID: 25611088.16. Toh HJ, Low JA, Lim ZY, Lim Y, Siddiqui S, Tan L. Jonsen’s four topics approach as a framework for clinical ethics consultation. Asian Bioeth Rev. 2018; 10(1):37–51. PMID: 33717274.17. Jonsen AR, Siegler M, Winslade WJ. Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine. 9th ed. New York, NY, USA: McGraw-Hill Education;2015.18. Lo B. Resolving Ethical Dilemmas: A Guide for Clinicians. 6th ed. Philadelphia, PA, USA: Lippincott Williams & Wilkins;2019.19. Gorka C, Craig JM, Spielman BJ. Growing an ethics consultation service: a longitudinal study examining two decades of practice. AJOB Empir Bioeth. 2017; 8(2):116–127. PMID: 28949846.20. Davies B, Sehring SA, Partridge JC, Cooper BA, Hughes A, Philp JC, et al. Barriers to palliative care for children: perceptions of pediatric health care providers. Pediatrics. 2008; 121(2):282–288. PMID: 18245419.21. Coventry PA, Grande GE, Richards DA, Todd CJ. Prediction of appropriate timing of palliative care for older adults with non-malignant life-threatening disease: a systematic review. Age Ageing. 2005; 34(3):218–227. PMID: 15863407.22. Choi K. Issues and tasks in the Hospice, Palliative Care, and Life-sustaining Treatment Decision-making Act. Korean J Med Ethics. 2016; 19(2):121–140.23. Jeong GH, Nam SH, Jung EJ, Lee JH, Lee YK, Kim JS, et al. Policy Implications of Changes in Family Structure: Focused on the Increase of Single Person Households in Korea. Sejong, Korea: Korea Institute for Health and Social Affairs;2012.24. Kim B, Kim M. Developing policy for life sustaining treatment decision for patient without surrogate. Korean J Med Ethics. 2018; 21(2):114–128.25. Kim B, Kim M. Using a health care proxy to overcome limitations of the Act on Decisions on Life-sustaining Treatment. Korean J Med Ethics. 2018; 21(2):95–113.26. Kim K, Huh J. Problems with the decision to end life of unrepresented persons and the tasks of the ethics committee. Korean Journal of Medicine and Law. 2020; 28(1):7–34.27. Kayser JB, Kaplan LJ. Conflict management in the ICU. Crit Care Med. 2020; 48(9):1349–1357. PMID: 32618689.28. Nicoli F, Cummins P, Raho JA, Porz R, Minoja G, Picozzi M. “If an acute event occurs, what should we do?” Diverse ethical approaches to decision-making in the ICU. Med Health Care Philos. 2019; 22(3):475–486. PMID: 30671733.29. Au SS, Couillard P, Roze des Ordons A, Fiest KM, Lorenzetti DL, Jette N. Outcomes of ethics consultations in adult ICUs: a systematic review and meta-analysis. Crit Care Med. 2018; 46(5):799–808. PMID: 29394183.30. Picozzi M, Gasparetto A. Clinical ethics consultation in the intensive care unit. Minerva Anestesiol. 2020; 86(6):670–677. PMID: 32000471.31. Fukuyama M, Asai A, Itai K, Bito S. A report on small team clinical ethics consultation programmes in Japan. J Med Ethics. 2008; 34(12):858–862. PMID: 19043109.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Life-sustaining treatment and palliative care in patients with liver cirrhosis - legal, ethical, and practical issues
- Experiences of Ethical Issues and Needs for Ethics Education in Clinical Nurses
- Regulatory Trends and Ethical Issues in Advanced Regenerative Medicine
- The Differences of Nurses' Perception of the Code of Ethics, Degree of Application of Nursing Ethics and Biomedical Ethical Consciousness according to Nursing Students' Clinical Practice Experience, Ethical Values and Biomedical Ethics Education
- A Review of Codes of Ethics in the United States and Ethical Dilemmas Surrounding the Native American Graves Protection and Repatriation Act (NAGPRA)