Anesth Pain Med.
2023 Apr;18(2):169-176. 10.17085/apm.22169.
Transient decrease in B-type natriuretic peptide level after liver transplantation does not ensure favorable post-transplant 30-day outcomes
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Laboratory for Cardiovascular Dynamics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2543658
- DOI: http://doi.org/10.17085/apm.22169
Abstract
- Background
High B-type natriuretic peptide (BNP) levels within the first 3 postoperative days (postBNPPOD3) after liver transplantation (LT) are greatly predictive of the 30-day mortality. We evaluated clinical impact of transient decrease in postBNPPOD3 compared to pretransplant BNP (preBNP) level on mortality and major adverse cardiac event (MACE) within 30 days after LT.
Methods
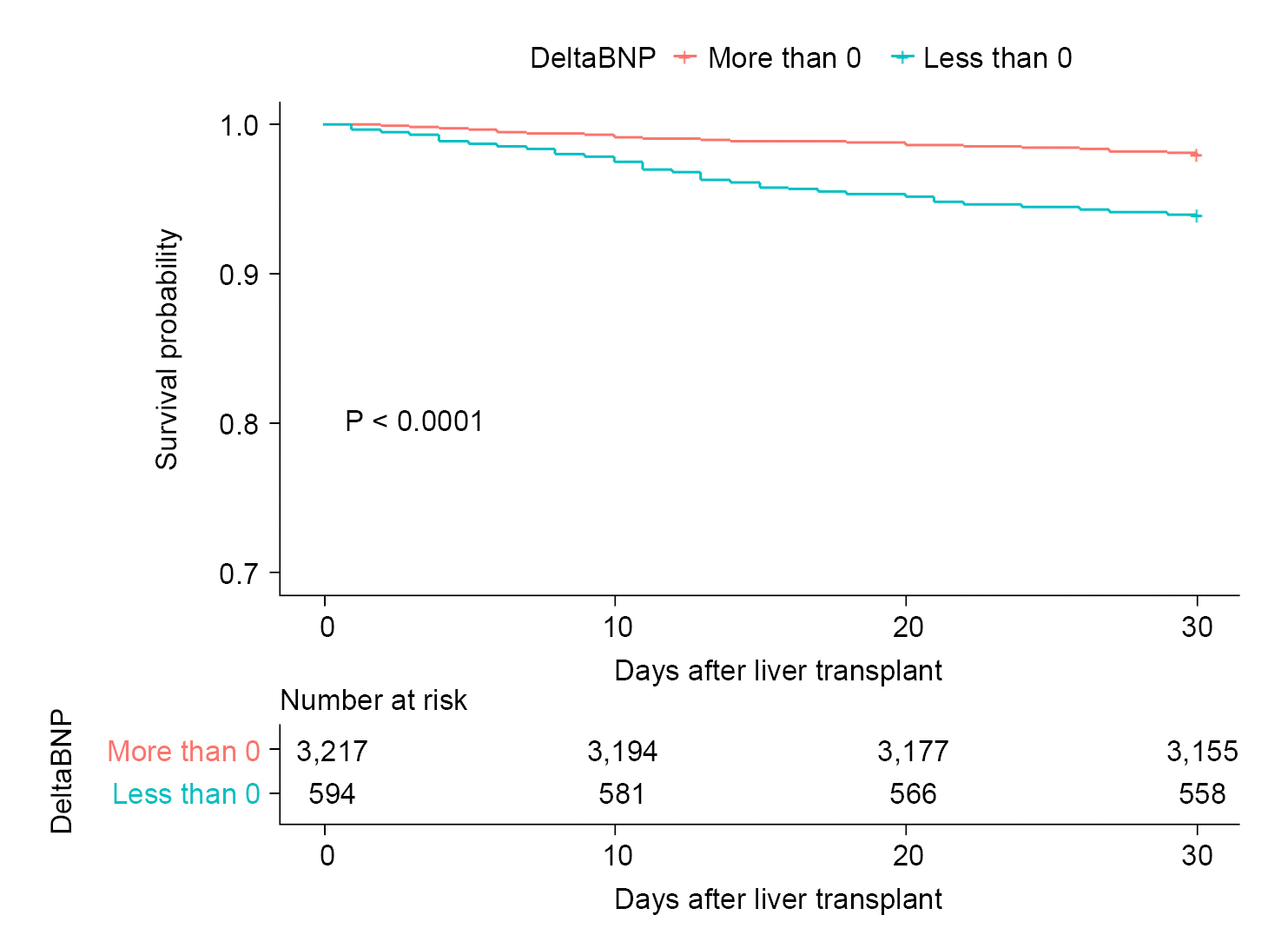
We retrospectively evaluated 3,811 LT patients who measured delta BNP (deltaBNP), defined by serial postBNPPOD3 minus preBNP. Thirty-day all-cause mortality and MACE were estimated in patients with deltaBNP < 0 (n = 594, 15.6%) and > 0 (n = 3,217, 84.4%), respectively. Kaplan-Meier survival and multivariable Cox regression analysis were used.
Results
Within 30 days, 100 (2.6%) of all patients died. Unexpectedly, 30-day mortality rate (6.1% [95% CI: 4.2–8.4%] vs. 2.0% [95% CI: 1.5–2.5%], P < 0.001) and MACE (24.2% [95% CI: 20.4–28.5%] vs. 15.3% [95% CI: 14.0–16.7%], P < 0.001) were higher in patients with deltaBNP < 0 compared to those with deltaBNP > 0, respectively. Patients with deltaBNP < 0 had higher preBNP level (median [interquartile range], 251 [118, 586] vs. 43 [21, 92] pg/ml, P < 0.001) and model for end-stage liver disease score (26 [14, 37] vs. 14 [9, 23], P < 0.001) and more transfused intraoperatively. DeltaBNP < 0 remained significant after adjustments for potential confounders in multivariable analysis of 30-day mortality and MACE.
Conclusions
DeltaBNP < 0 within the first 3 postoperative days is mainly attributed to pre-LT severe liver and cardiac disease status, therefore, transient decrease in BNP level after LT does not ensure favorable post-LT 30-day outcomes.
Figure
Reference
-
1. Izzy M, VanWagner LB, Lee SS, Altieri M, Angirekula M, Watt KD. Understanding and managing cardiovascular outcomes in liver transplant recipients. Curr Opin Organ Transplant. 2019; 24:148–55.
Article2. Kwon HM, Hwang GS. Cardiovascular dysfunction and liver transplantation. Korean J Anesthesiol. 2018; 71:85–91.
Article3. VanWagner LB, Lapin B, Levitsky J, Wilkins JT, Abecassis MM, Skaro AI, et al. High early cardiovascular mortality after liver transplantation. Liver Transpl. 2014; 20:1306–16.
Article4. Kwon HM, Moon YJ, Kim KS, Shin WJ, Huh IY, Jun IG, et al. Prognostic value of B-type natriuretic peptide in liver transplant patients: implication in posttransplant mortality. Hepatology. 2021; 74:336–50.
Article5. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016; 18:891–975.
Article6. Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2014; 130:2215–45.
Article7. Moon KW. R statistics and graphs for medical papers. Seoul: Hannarae;2015.8. Moon KW. Survival analysis with R for medical personnel. Seoul: Hannarae;2022.9. Kassambara A, Kosinski M, Biecek P. survminer: survival analysis and visualization. ggsurvplot: drawing survival curves [Internet]. 2021. [2022 Jan 3]. Available from https://rpkgs.datanovia.com/survminer/.10. Therneau T. A package for survival analysis in R. Version 3.2-13 [Internet]. 2021. [updated 2022 Jan 9; 2023 Jan 3]. Available from https://cran.r-project.org/web/packages/survival/index.html.11. Kim YK, Shin WJ, Song JG, Kim Y, Kim WJ, Kim SH, et al. Evaluation of intraoperative brain natriuretic peptide as a predictor of 1-year mortality after liver transplantation. Transplant Proc. 2011; 43:1684–90.
Article12. Rodseth RN, Biccard BM, Le Manach Y, Sessler DI, Lurati Buse GA, Thabane L, et al. The prognostic value of pre-operative and post-operative B-type natriuretic peptides in patients undergoing noncardiac surgery: B-type natriuretic peptide and N-terminal fragment of pro-B-type natriuretic peptide: a systematic review and individual patient data meta-analysis. J Am Coll Cardiol. 2014; 63:170–80.13. Saner FH, Neumann T, Canbay A, Treckmann JW, Hartmann M, Goerlinger K, et al. High brain-natriuretic peptide level predicts cirrhotic cardiomyopathy in liver transplant patients. Transpl Int. 2011; 24:425–32.
Article14. Rodseth RN, Biccard BM, Chu R, Lurati Buse GA, Thabane L, Bakhai A, et al. Postoperative B-type natriuretic peptide for prediction of major cardiac events in patients undergoing noncardiac surgery: systematic review and individual patient meta-analysis. Anesthesiology. 2013; 119:270–83.15. Vernooij LM, van Klei WA, Moons KG, Takada T, van Waes J, Damen JA. The comparative and added prognostic value of biomarkers to the Revised Cardiac Risk Index for preoperative prediction of major adverse cardiac events and all-cause mortality in patients who undergo noncardiac surgery. Cochrane Database Syst Rev. 2021; 12:CD013139.
Article16. Ryding AD, Kumar S, Worthington AM, Burgess D. Prognostic value of brain natriuretic peptide in noncardiac surgery: a meta-analysis. Anesthesiology. 2009; 111:311–9.17. Møller S, Bendtsen F. Cirrhotic multiorgan syndrome. Dig Dis Sci. 2015; 60:3209–25.
Article18. Møller S, Danielsen KV, Wiese S, Hove JD, Bendtsen F. An update on cirrhotic cardiomyopathy. Expert Rev Gastroenterol Hepatol. 2019; 13:497–505.
Article19. Møller S, Henriksen JH. Cirrhotic cardiomyopathy. J Hepatol. 2010; 53:179–90.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric Liver Transplantation
- B-type natriuretic peptide in anesthesia practice to predict adverse cardiovascular outcomes
- Biomarkers in Heart Failure: Focus on B-type Natriuretic Peptide
- B-type natriuretic peptide may have a role in the management of patent ductus arteriosus
- High Plasma Levels of the B-type Natriuretic Peptide in Patients Without Heart Failure: Is There Clinical Significance?