Acute Crit Care.
2023 May;38(2):182-189. 10.4266/acc.2022.00206.
The role of ROX index–based intubation in COVID-19 pneumonia: a cross-sectional comparison and retrospective survival analysis
- Affiliations
-
- 1Department of Anaesthesiology and Critical Care, MOSC Medical College, Kerala, India
- 2Department of Surgery, MOSC Medical College, Kerala, India
- 3North Cumbria Integrated Care NHS Trust, Whitehaven, UK
- KMID: 2543637
- DOI: http://doi.org/10.4266/acc.2022.00206
Abstract
- Background
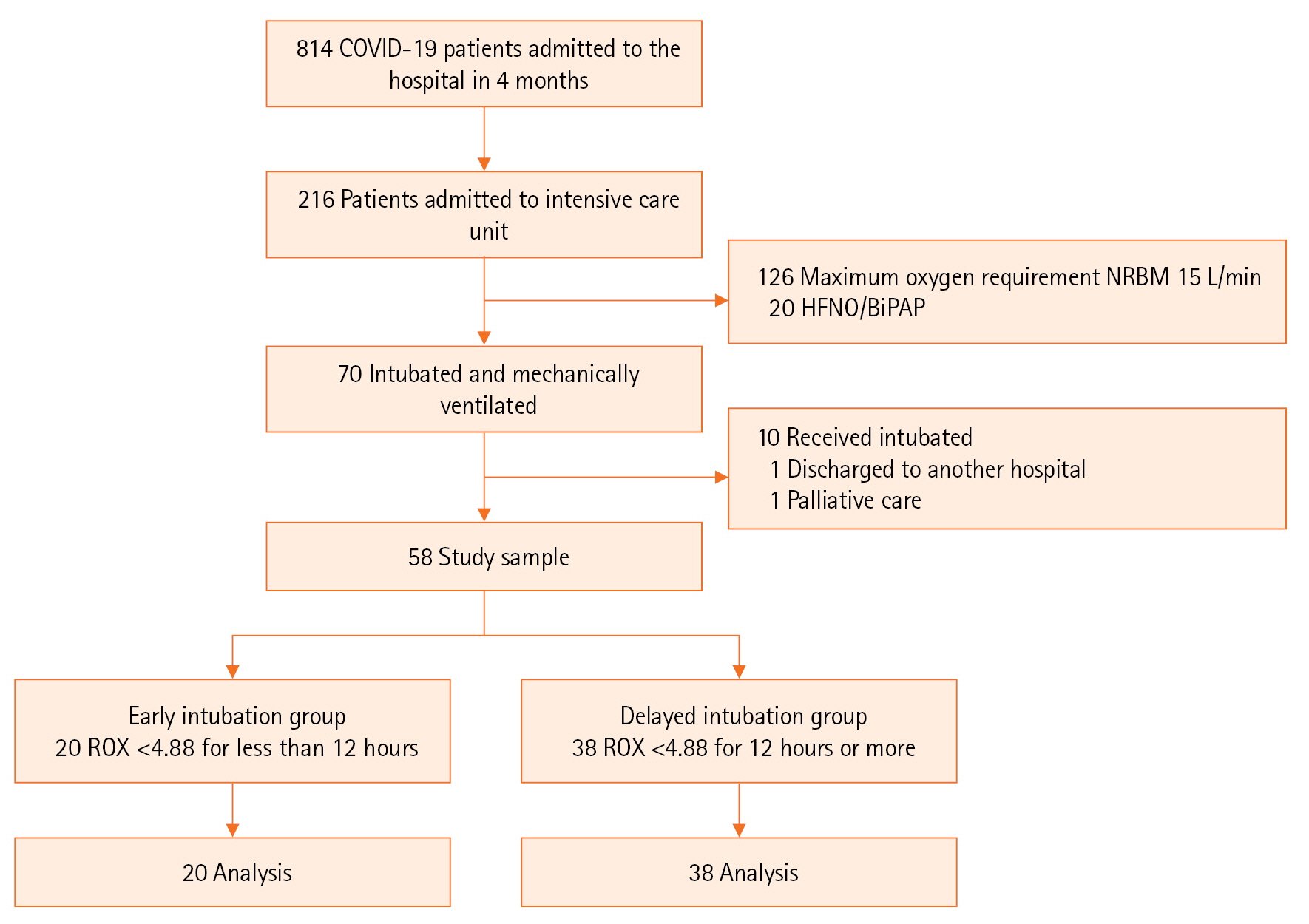
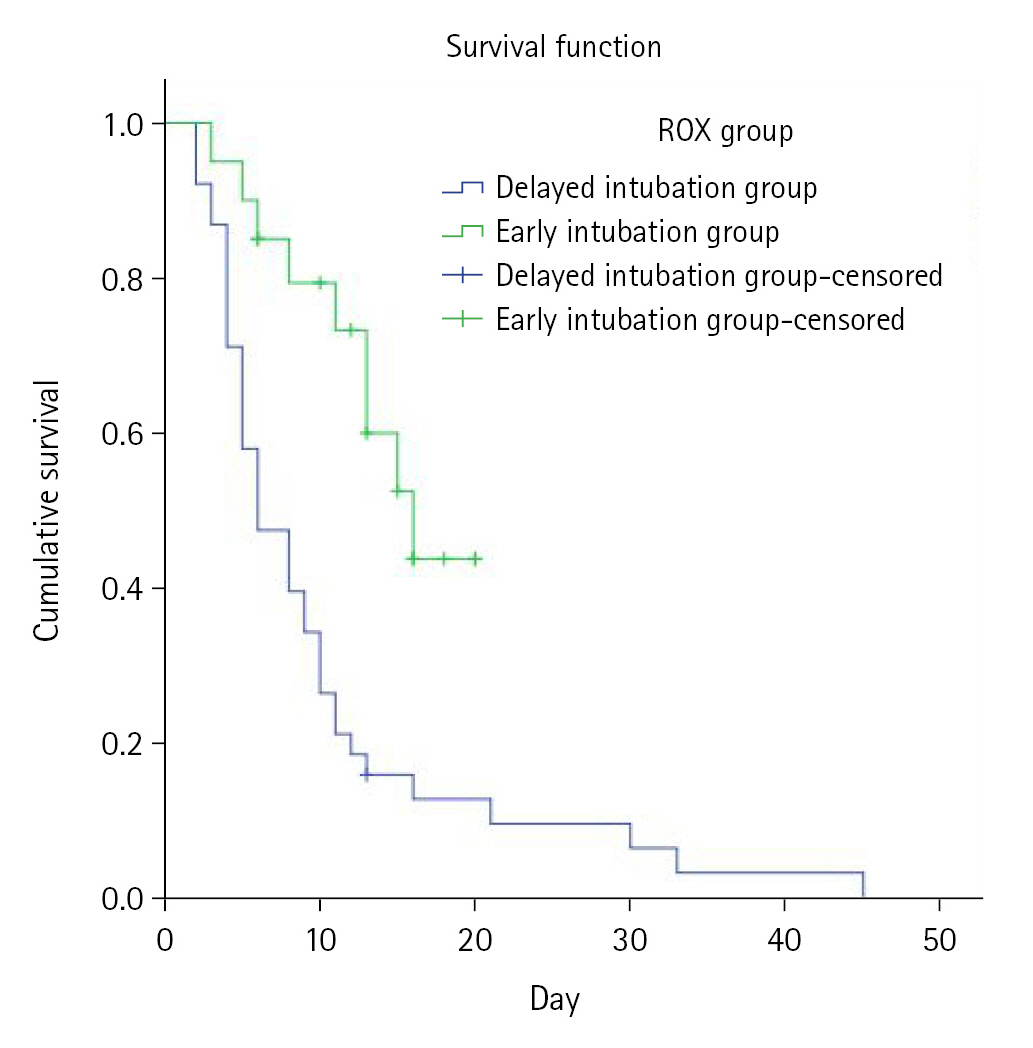
Coronavirus disease 2019 (COVID-19) patients with acute respiratory failure who experience delayed initiation of invasive mechanical ventilation have poor outcomes. The lack of objective measures to define the timing of intubation is an area of concern. We investigated the effect of timing of intubation based on respiratory rate-oxygenation (ROX) index on the outcomes of COVID-19 pneumonia. Methods: This was a retrospective cross-sectional study performed in a tertiary care teaching hospital in Kerala, India. Patients with COVID-19 pneumonia who were intubated were grouped into early intubation (within 12 hours of ROX index <4.88) or delayed intubation (12 hours or more hours after ROX <4.88). Results: A total of 58 patients was included in the study after exclusions. Among them, 20 patients were intubated early, and 38 patients were intubated 12 hours after ROX index <4.88. The mean age of the study population was 57±14 years, and 55.0% of the patients were male; diabetes mellitus (48.3%) and hypertension (50.0%) were the most common comorbidities. The early intubation group had 88.2% successful extubation, while only 11.8% of the delayed group had successful extubation (P<0.001). Survival was also significantly more frequent in the early intubation group. Conclusions: Early intubation within 12 hours of ROX index <4.88 was associated with improved extubation and survival in patients with COVID-19 pneumonia.
Keyword
Figure
Reference
-
1. Varikasuvu SR, Varshney S, Dutt N, Munikumar M, Asfahan S, Kulkarni PP, et al. D-dimer, disease severity, and deaths (3D-study) in patients with COVID-19: a systematic review and meta-analysis of 100 studies. Sci Rep. 2021; 11:21888.
Article2. Meng L, Qiu H, Wan L, Ai Y, Xue Z, Guo Q, et al. Intubation and ventilation amid the COVID-19 outbreak: Wuhan's experience. Anesthesiology. 2020; 132:1317–32.3. Tobin MJ, Laghi F, Jubran A. Caution about early intubation and mechanical ventilation in COVID-19. Ann Intensive Care. 2020; 10:78.
Article4. Kang BJ, Koh Y, Lim CM, Huh JW, Baek S, Han M, et al. Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med. 2015; 41:623–32.
Article5. Roca O, Caralt B, Messika J, Samper M, Sztrymf B, Hernández G, et al. An index combining respiratory rate and oxygenation to predict outcome of nasal high-flow therapy. Am J Respir Crit Care Med. 2019; 199:1368–76.
Article6. Patel BK, Wolfe KS, Pohlman AS, Hall JB, Kress JP. Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2016; 315:2435–41.
Article7. Suliman LA, Abdelgawad TT, Farrag NS, Abdelwahab HW. Validity of ROX index in prediction of risk of intubation in patients with COVID-19 pneumonia. Adv Respir Med. 2021; 89:1–7.
Article8. Kim JH, Baek AR, Lee SI, Kim WY, Na YS, Lee BY, et al. ROX index and SpO2/FiO2 ratio for predicting high-flow nasal cannula failure in hypoxemic COVID-19 patients: a multicenter retrospective study. PLoS One. 2022; 17:e0268431.9. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008; 61:344–9.
Article10. Zirpe KG, Tiwari AM, Gurav SK, Deshmukh AM, Suryawanshi PB, Wankhede PP, et al. Timing of invasive mechanical ventilation and mortality among patients with severe COVID-19-associated acute respiratory distress syndrome. Indian J Crit Care Med. 2021; 25:493–8.
Article11. Wunsch H. Mechanical ventilation in COVID-19: interpreting the current epidemiology. Am J Respir Crit Care Med. 2020; 202:1–4.
Article12. Wang Y, Lu X, Li Y, Chen H, Chen T, Su N, et al. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med. 2020; 201:1430–4.
Article13. Pfortmueller CA, Spinetti T, Urman RD, Luedi MM, Schefold JC. COVID-19-associated acute respiratory distress syndrome (CARDS): current knowledge on pathophysiology and ICU treatment. A narrative review. Best Pract Res Clin Anaesthesiol. 2021; 35:351–68.14. Wang Z, Deng H, Ou C, Liang J, Wang Y, Jiang M, et al. Clinical symptoms, comorbidities and complications in severe and non-severe patients with COVID-19: a systematic review and meta-analysis without cases duplication. Medicine (Baltimore). 2020; 99:e23327.15. Song SE, Lee SH, Jo EJ, Eom JS, Mok JH, Kim MH, et al. The prognostic value of the Charlson's comorbidity index in patients with prolonged acute mechanical ventilation: a single center experience. Tuberc Respir Dis (Seoul). 2016; 79:289–94.
Article16. Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001; 286:1754–8.
Article17. Fuchs PA, Czech IJ, Krzych ŁJ. Mortality prediction using SOFA score in critically ill surgical and non-surgical patients: which parameter is the most valuable? Medicina (Kaunas). 2020; 56:273.
Article18. Raschke RA, Agarwal S, Rangan P, Heise CW, Curry SC. Discriminant accuracy of the SOFA score for determining the probable mortality of patients with COVID-19 pneumonia requiring mechanical ventilation. JAMA. 2021; 325:1469–70.
Article19. Gianstefani A, Farina G, Salvatore V, Alvau F, Artesiani ML, Bonfatti S, et al. Role of ROX index in the first assessment of COVID-19 patients in the emergency department. Intern Emerg Med. 2021; 16:1959–65.
Article20. Patel M, Chowdhury J, Mills N, Marron R, Gangemi A, Dorey-Stein Z, et al. Utility of the ROX index in predicting intubation for patients with COVID-19-related hypoxemic respiratory failure receiving high-flow nasal therapy: retrospective cohort study. JMIRx Med. 2021; 2:e29062.
Article21. Hyman JB, Leibner ES, Tandon P, Egorova NN, Bassily-Marcus A, Kohli-Seth R, et al. Timing of intubation and in-hospital mortality in patients with coronavirus disease 2019. Crit Care Explor. 2020; 2:e0254.
Article22. Papoutsi E, Giannakoulis VG, Xourgia E, Routsi C, Kotanidou A, Siempos II. Effect of timing of intubation on clinical outcomes of critically ill patients with COVID-19: a systematic review and meta-analysis of non-randomized cohort studies. Crit Care. 2021; 25:121.
Article23. Weaver L, Das A, Saffaran S, Yehya N, Scott TE, Chikhani M, et al. High risk of patient self-inflicted lung injury in COVID-19 with frequently encountered spontaneous breathing patterns: a computational modelling study. Ann Intensive Care. 2021; 11:109.
Article24. Chaddha U, Kaul V, Agrawal A. What is the true mortality in the critically ill patients with COVID-19? Indian J Crit Care Med. 2020; 24:383–4.
Article25. Nath R, Gupta NK, Jaswal A, Gupta S, Kaur N, Kohli S, et al. Mortality among adult hospitalized patients during the first wave and second wave of COVID-19 pandemic at a tertiary care center in India. Monaldi Arch Chest Dis. 2021; 92.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of Early Warning Scores, ROX index, and CURB-65 in the prognostic evaluation of patients with COVID-19
- Evaluating the use of the respiratory-rate oxygenation index as a predictor of high-flow nasal cannula oxygen failure in COVID-19
- The Comparison of Dysphagia between COVID-19 Pneumonia and Aspiration Pneumonia
- A Comparison of Changes in Health Behavior, Obesity, and Mental Health of Korean Adolescents Before and During the COVID-19 Pandemic: Online Cross-Sectional Study
- Clinical and Radiologic Findings of COVID-19 Pneumonia: South Korean Experience from Three Cases