Acute Crit Care.
2023 Feb;38(1):31-40. 10.4266/acc.2022.01081.
Evaluating the use of the respiratory-rate oxygenation index as a predictor of high-flow nasal cannula oxygen failure in COVID-19
- Affiliations
-
- 1Department of Critical Care Medicine, King’s College Hospital NHS Foundation Trust, London, UK
- KMID: 2540312
- DOI: http://doi.org/10.4266/acc.2022.01081
Abstract
- Background
It can be challenging for clinicians to predict which patients with respiratory failure secondary to coronavirus disease 2019 (COVID-19) will fail on high-flow nasal cannula (HFNC) oxygen and require escalation of therapy. This study set out to evaluate the association between the respiratory rate-oxygenation index (ROX) and HFNC failure in such patients and to assess whether ROX trajectory correlates with treatment failure.
Methods
This was a single-centre, retrospective, observational study of patients with COVID-19 requiring HFNC, conducted over a 3-month period. ROX was calculated as “pulse-oximetry oxygen saturation (SpO2) over the fractional inspired oxygen concentration (FiO2)/respiratory rate” for each patient at 2, 4, and 12 hours from starting HFNC. HFNC failure was defined as escalation to continuous positive airway pressure ventilation or invasive mechanical ventilation (IMV). Time-to-event analyses were performed to account for the longitudinal data set and time-dependent variables.
Results
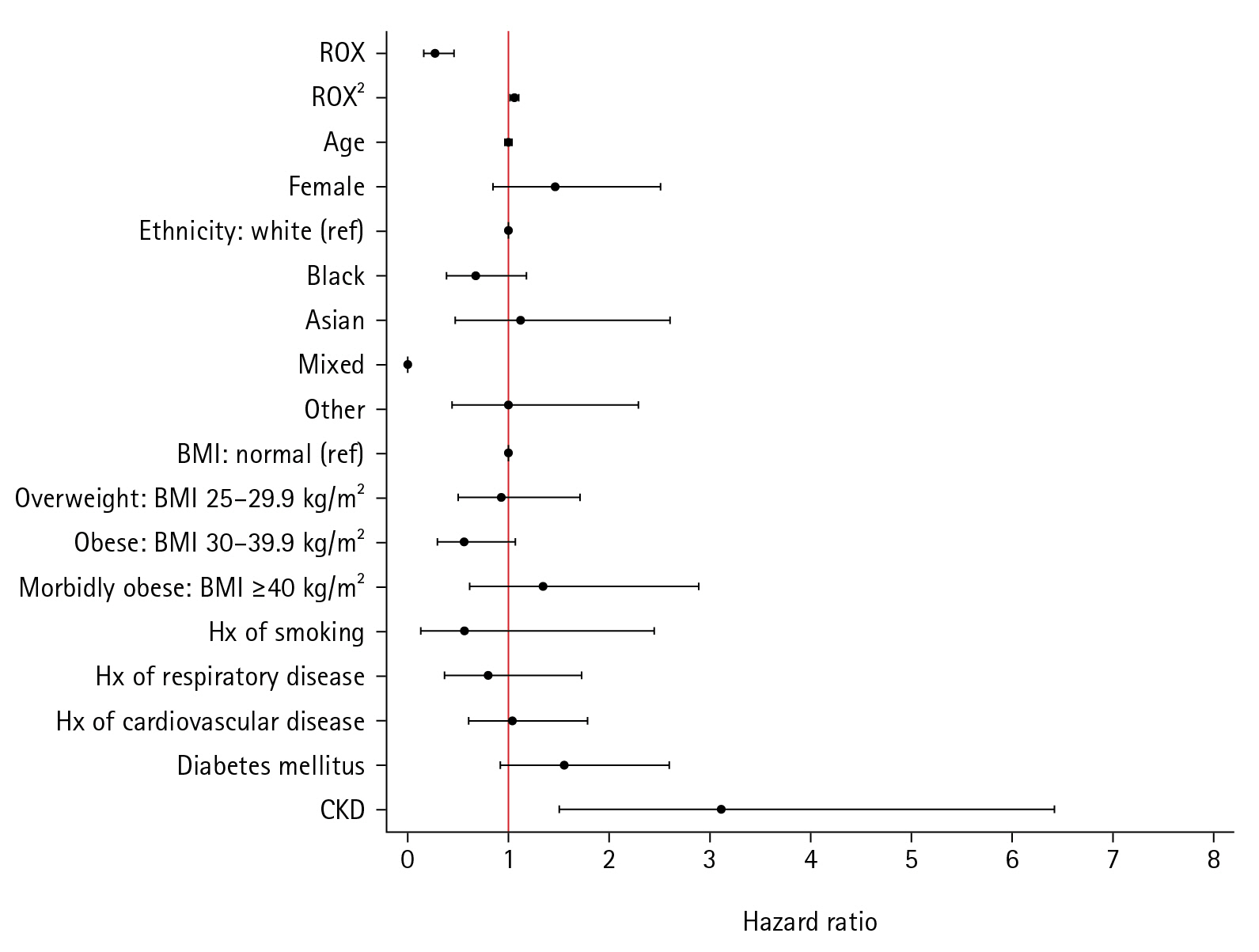
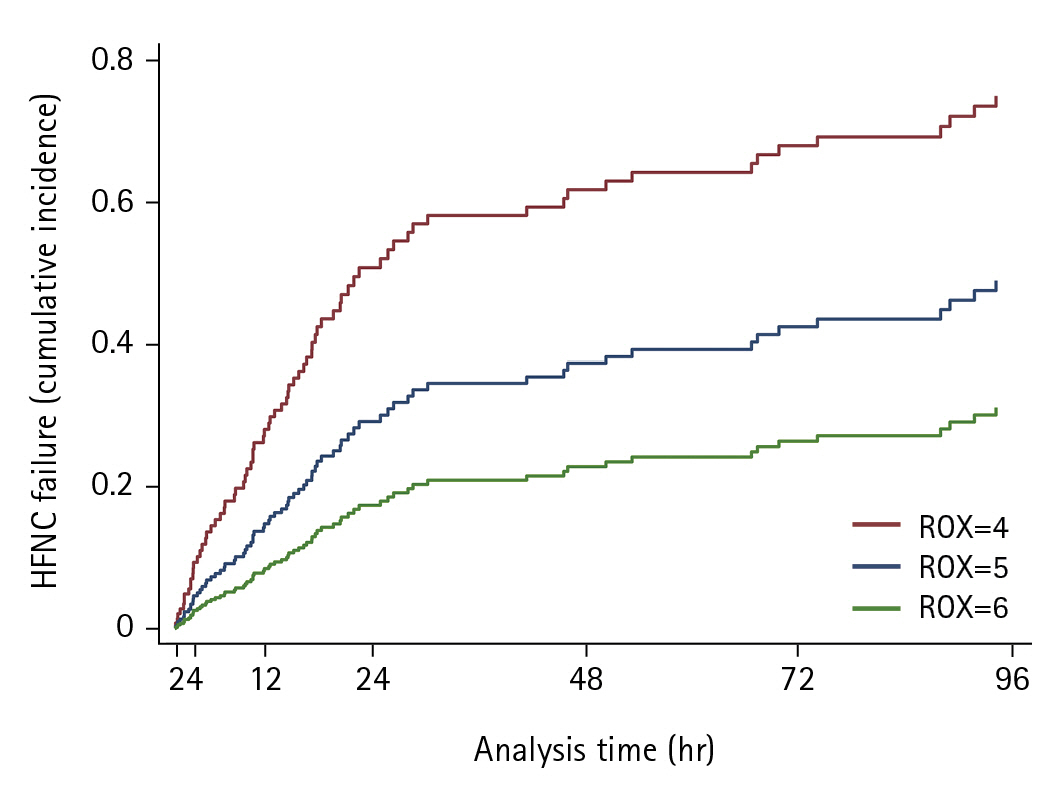
We included 146 patients. Ninety-three (63.7%) experienced HFNC failure, with 53 (36.3%) requiring IMV. Higher ROX values were associated with a lower subhazard of HFNC failure on time-to-HFNC failure analysis (subhazard ratio, 0.29; 95% confidence interval [CI], 0.18–0.46; P<0.001). This remained true after controlling for informative censoring. Median ROX values changed differentially over time, increasing in the HFNC success group (0.06 per hour; 95% CI, 0.05–0.08; P<0.001) but not in the HFNC failure group (0.004 per hour; 95% CI, –0.05 to 0.08; P=0.890).
Conclusions
A higher ROX is associated with a lower risk of HFNC failure. Monitoring ROX trajectory over time may help identify patients at risk of treatment failure. This has potential clinical applications; however, future prospective studies are required.
Figure
Reference
-
1. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020; 323:1574–81.2. Tzotzos SJ, Fischer B, Fischer H, Zeitlinger M. Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey. Crit Care. 2020; 24:1–4.3. Marini JJ, Gattinoni L. Management of COVID-19 respiratory distress. JAMA. 2020; 323:2329.4. Costa WN da S, Miguel JP, Prado F dos S, Lula LHS de M, Amarante GAJ, Righetti RF, et al. Noninvasive ventilation and high-flow nasal cannula in patients with acute hypoxemic respiratory failure by covid-19: a retrospective study of the feasibility, safety and outcomes. Respir Physiol Neurobiol. 2022; 298:103842.5. Duan J, Chen B, Liu X, Shu W, Zhao W, Li J, et al. Use of high-flow nasal cannula and noninvasive ventilation in patients with COVID-19: a multicenter observational study. Am J Emerg Med. 2021; 46:276–81.6. Rochwerg B, Granton D, Wang DX, Helviz Y, Einav S, Frat JP, et al. High flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: a systematic review and meta-analysis. Intensive Care Med. 2019; 45:563–72.7. Drake MG. High-flow nasal cannula oxygen in adults: an evidence-based assessment. Ann Am Thorac Soc. 2018; 15:145–55.8. Patel M, Gangemi A, Marron R, Chowdhury J, Yousef I, Zheng M, et al. Retrospective analysis of high flow nasal therapy in COVID-19-related moderate-to-severe hypoxaemic respiratory failure. BMJ Open Respir Res. 2020; 7:1–11.9. Shoukri AM. High flow nasal cannula oxygen and non-invasive mechanical ventilation in management of COVID-19 patients with acute respiratory failure: a retrospective observational study. Egypt J Bronchol. 2021; 15:17.10. Demoule A, Baron AV, Darmon M, Beurton A, Géri G, Voiriot G, et al. High-flow nasal cannula in critically Ill patients with severe COVID-19. Am J Respir Crit Care Med. 2020; 202:1039–42.11. Calligaro GL, Lalla U, Audley G, Gina P, Miller MG, Mendelson M, et al. The utility of high-flow nasal oxygen for severe COVID-19 pneumonia in a resource-constrained setting: a multi-centre prospective observational study. EClinicalMedicine. 2020; 28:100570.12. Kang BJ, Koh Y, Lim CM, Huh JW, Baek S, Han M, et al. Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med. 2015; 41:623–32.13. Roca O, Messika J, Caralt B, García-de-Acilu M, Sztrymf B, Ricard JD, et al. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: the utility of the ROX index. J Crit Care. 2016; 35:200–5.14. Roca O, Caralt B, Messika J, Samper M, Sztrymf B, Hernández G, et al. A novel risk-stratification models of the high-flow nasal cannula therapy in COVID-19 patients with hypoxemic respiratory failure. Am J Respir Crit Care Med. 2019; 199:1368–76.15. Xu J, Yang X, Huang C, Zou X, Zhou T, Pan S, et al. A Novel Risk-Stratification Models of the High-Flow Nasal Cannula Therapy in COVID-19 Patients With Hypoxemic Respiratory Failure. Front Med. 2020; 7:1–9.16. Hu M, Zhou Q, Zheng R, Li X, Ling J, Chen Y, et al. Application of high-flow nasal cannula in hypoxemic patients with COVID-19: a retrospective cohort study. BMC Pulm Med. 2020; 20:1–7.17. Chandel A, Patolia S, Brown AW, Collins AC, Sahjwani D, Khangoora V, et al. High-flow nasal cannula therapy in COVID-19: using the ROX index to predict success. Respir Care. 2021; 66:909–19.18. Panadero C, Abad-Fernández A, Rio-Ramirez MT, Acosta Gutierrez CM, Calderon-Alcala M, Lopez-Riolobos C, et al. High-flow nasal cannula for acute respiratory distress syndrome (ARDS) due to COVID-19. Multidiscip Respir Med. 2020; 15:693.19. Blez D, Soulier A, Bonnet F, Gayat E, Garnier M. Monitoring of high-flow nasal cannula for SARS-CoV-2 severe pneumonia: less is more, better look at respiratory rate. Intensive Care Med. 2020; 46:2094–5.20. Vega ML, Dongilli R, Olaizola G, Colaianni N, Sayat MC, Pisani L, et al. COVID-19 pneumonia and ROX index: time to set a new threshold for patients admitted outside the ICU. Pulmonology. 2022; 28:13–7.21. Zucman N, Mullaert J, Roux D, Roca O, Ricard JD, Longrois D, et al. Prediction of outcome of nasal high flow use during COVID-19-related acute hypoxemic respiratory failure. Intensive Care Med. 2020; 46:1924–6.22. Myers LC, Mark D, Ley B, Guarnieri M, Hofmeister M, Paulson S, et al. Validation of respiratory rate-oxygenation index in patients with COVID-19-related respiratory failure. Crit Care Med. 2022; 50:e638–42.23. Ferrer S, Sancho J, Bocigas I, Bures E, Mora H, Monclou E, et al. ROX index as predictor of high flow nasal cannula therapy success in acute respiratory failure due to SARS-CoV-2. Respir Med. 2021; 189:106638.24. Prakash J, Bhattacharya PK, Yadav AK, Kumar A, Tudu LC, Prasad K. ROX index as a good predictor of high flow nasal cannula failure in COVID-19 patients with acute hypoxemic respiratory failure: a systematic review and meta-analysis. J Crit Care. 2021; 66:102–8.25. Leszek A, Wozniak H, Giudicelli‐bailly A, Suh N, Boroli F, Pugin J, et al. measurement of ROX index in intermediary care unit is associated with mortality in intubated COVID-19 patients: a retrospective study. J Clin Med. 2022; 11:365.26. Alshaqaq HM, Aseri ZA Al, Alshahrani MS. High ‑ Flow Nasal Cannula for Patients with COVID ‑ 19 Acute Hypoxemic Respiratory Failure. Saudi Crit Care J. 2020; 4(5 Suppl):6–9.27. Rice TW, Wheeler AP, Bernard GR, Hayden DL, Schoenfeld DA, Ware LB. SpO2/FIO2 ratio and the PaO2/FIO2 ratio in patients with acute lung injury or ARDS. Chest. 2007; 132:410–7.28. Babu S, Abhilash KP, Kandasamy S, Gowri M. Association between spo2/fio2 ratio and pao2/fio2 ratio in different modes of oxygen supplementation. Indian J Crit Care Med. 2021; 25:1001–5.29. Knight SR, Ho A, Pius R, Buchan I, Carson G, Drake TM, et al. Risk stratification of patients admitted to hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ. 2020; 370:m3339.30. Fine JP, Gray RJ. Proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999; 94:496–509.31. Crowther MJ, Abrams KR, Lambert PC. Joint modeling of longitudinal and survival data. Stata J. 2013; 13:165–84.32. Andersson TML, Crowther MJ, Czene K, Hall P, Humphreys K. Mammographic density reduction as a prognostic marker for postmenopausal breast cancer: results using a joint longitudinal-survival modeling approach. Am J Epidemiol. 2017; 186:1065–73.33. Glenardi G, Chriestya F, Oetoro BJ, Mangkuliguna G, Natalia N. Comparison of high-flow nasal oxygen therapy and noninvasive ventilation in COVID-19 patients: a systematic review and meta-analysis. Acute Crit Care. 2022; 37:71–83.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High-flow nasal cannula for respiratory failure in adult patients
- Combining reservoir mask oxygenation with high-flow nasal cannula in the treatment of hypoxemic respiratory failure among patients with COVID-19 pneumonia: a retrospective cohort study
- Factors about Failure after High Flow Oxygen through Nasal Cannula Therapy in Hypoxic Respiratory Failure Patients at Emergency Department Presentation
- Treatment of acute respiratory failure: high-flow nasal cannula
- Study on the Changes of SaO2, According to the Different Type of Oxygen Suppliers