Korean J healthc assoc Infect Control Prev.
2023 Jun;28(1):155-166. 10.14192/kjicp.2023.28.1.155.
Characteristics and Affecting Factors of Hand Hygiene Adherence of Healthcare Workers at Operating Room Using Self- administered and Direct-observational Method
- Affiliations
-
- 1Operating Room, Dankook University Hospital, Cheonan, Korea
- 2Department of Clinical Nursing, University of Ulsan Graduate School of Industry, Seoul, Korea
- 3College of Nursing, Chodang University, Muan, Korea
- KMID: 2543146
- DOI: http://doi.org/10.14192/kjicp.2023.28.1.155
Abstract
- Background
Hand hygiene (HH) is needed for healthcare workers (HCWs) at the operating room (OR) to prevent their hands from becoming reservoirs for pathogenic. This study was carried out to investigate the level of knowledge and perception and the barriers to HH and to identify the factors that affect HH.
Methods
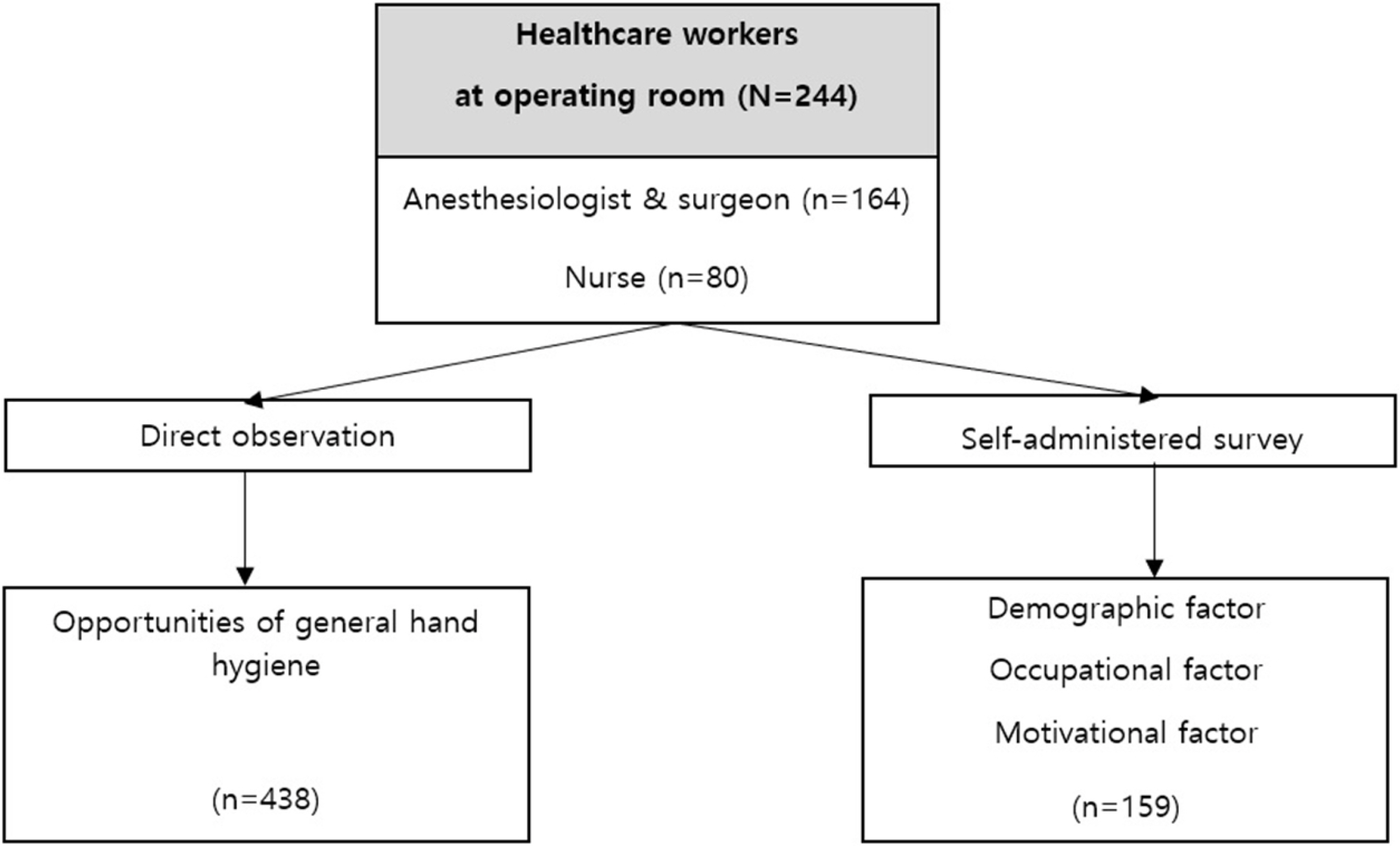
This was a cross-sectional study. The participants were those who worked at an OR at a teaching hospital. A total of 244 HCWs were enrolled, among whom we distributed a selfadministered survey regarding the knowledge, perception, and barriers and adherence of to HH. Finally, 159 survey sheets were retrieved, and a concurrent direct-observation of HH was conducted.
Results
HH adherence was differed from the method using self-administration or direct observation. HH adherence accounted for 83.4% of the survey respondents and 68.5% with direct observation, with statistical significance (P<.001). This presented confirmative results in doctors (85.4% vs. 52.5%). The HH of HCWs in surgery (85.8%) was significantly higher than that of HCWs in anesthesia (76.0%). A multivariate hierarchical linear regression model was constructed by three-layer models consisting of demographic, occupational, and motivational factors. It revealed that perception, barrier, type of duty (surgery vs. anesthesia), and years of career experience were affecting factors of HH adherence.
Conclusion
The HH adherence of HCWs in anesthesia was lower than of those in surgery, presenting a wide gap between self-administration and direct observation. The HH perception increased with self-administered HH, but barriers acted reversely. Therefore, improvement on perception and decrease of the barriers is necessary to raise the HH adherence of HCWs in the OR.
Keyword
Figure
Reference
-
1. WHO. 2009. WHO guidelines on hand hygiene in health care: a summary. WHO;Geneva: p. 270.2. KCDC. 2017. Standard precaution guidelines for healthcare associated infecion. Korean Society for Healthcare-associated Infection Control;Seoul: p. 63–71.3. Zandiyeh M, Borzo SR. 2012; [The level of hand hygiene compliance by operating room personnel of Educational Hospitals in Hamadan University of Medical Science]. J Holist Nurs Midwifery. 22:23–9. Persian.4. Loftus RW, Dexter F, Robinson ADM. 2018; High-risk Staphylococcus aureus transmission in the operating room: a call for widespread improvements in perioperative hand hygiene and patient decolonization practices. Am J Infect Control. 46:1134–41. DOI: 10.1016/j.ajic.2018.04.211. PMID: 29907449.
Article5. Fukada T, Iwakiri H, Ozaki M. 2008; Anaesthetists' role in computer keyboard contamination in an operating room. J Hosp Infect. 70:148–53. DOI: 10.1016/j.jhin.2008.05.023. PMID: 18701192.
Article6. Loftus RW, Koff MD, Birnbach DJ. 2015; The dynamics and implications of bacterial transmission events arising from the anesthesia work area. Anesth Analg. 120:853–60. DOI: 10.1213/ANE.0000000000000505. PMID: 25790210.
Article7. Ezzat A, Safdar MM, Ahmed I. 2014; Are we following the WHO recommendations for surgical scrubbing? Scott Med J. 59:214–9. DOI: 10.1177/0036933014554885. PMID: 25311006.
Article8. Biddle C, Shah J. 2012; Quantification of anesthesia providers' hand hygiene in a busy metropolitan operating room: what would Semmelweis think? Am J Infect Control. 40:756–9. DOI: 10.1016/j.ajic.2011.10.008. PMID: 22325482.
Article9. Megeus V, Nilsson K, Karlsson J, Eriksson BI, Andersson AE. 2015; Hand hygiene and aseptic techniques during routine anesthetic care - observations in the operating room. Antimicrob Resist Infect Control. 4:5. DOI: 10.1186/s13756-015-0042-y. PMID: 25685334. PMCID: PMC4328079.
Article10. Krediet AC, Kalkman CJ, Bonten MJ, Gigengack AC, Barach P. 2011; Hand-hygiene practices in the operating theatre: an observational study. Br J Anaesth. 107:553–8. DOI: 10.1093/bja/aer162. PMID: 21665900.
Article11. Paul ET, Kuszajewski M, Davenport A, Thompson JA, Morgan B. 2019; Sleep safe in clean hands: improving hand hygiene compliance in the operating room through education and increased access to hand hygiene products. Am J Infect Control. 47:504–8. DOI: 10.1016/j.ajic.2018.10.021. PMID: 30553542.
Article12. Plemmons MM, Marcenaro J, Oermann MH, Thompson J, Vacchiano CA. 2019; Improving infection control practices of nurse anesthetists in the anesthesia workspace. Am J Infect Control. 47:551–7. DOI: 10.1016/j.ajic.2018.12.009. PMID: 30665777.
Article13. Lee Y, Shin H. 2017; A feasibility study of hand hygiene status in Korea hospitals. J Korea Inst Healthc Archit. 23:9–17.14. Zhou Q, Lai X, Wan Z, Zhang X, Tan L. 2021; Impact of burnout, secondary traumatic stress and compassion satisfaction on hand hygiene of healthcare workers during the COVID-19 pandemic. Nurs Open. 8:2551–7. DOI: 10.1002/nop2.786. PMCID: PMC8014518. PMID: 33605557.
Article15. Sax H, Uçkay I, Richet H, Allegranzi B, Pittet D. 2007; Determinants of good adherence to hand hygiene among healthcare workers who have extensive exposure to hand hygiene campaigns. Infect Control Hosp Epidemiol. 28:1267–74. DOI: 10.1086/521663. PMID: 17926278.
Article16. Park JA, Yang NY. 2018; Knowledge and compliance on hand hygiene moments of nursing care workers in geriatric hospitals. J Korean Acad Soc Home Health Care Nurs. 25:165–74.17. Kim HJ, Kim NC. 2005; A study of handwashing by intensive care unit nurses according to the content of nursing faculty practice. J Korean Acad Fundam Nurs. 12:121–30.18. Cha KS, Ko JW, Han SH, Jung KH. 2018; A survey of nurses' hand hygiene knowledge, perception and hand hygiene performance rate. J Korean Crit Care Nurs. 11:101–9.19. Pedersen L, Elgin K, Peace B, Masroor N, Doll M, Sanogo K, et al. 2017; Barriers, perceptions, and adherence: hand hygiene in the operating room and endoscopy suite. Am J Infect Control. 45:695–7. DOI: 10.1016/j.ajic.2017.01.003. PMID: 28189412.
Article20. Santosaningsih D, Erikawati D, Santoso S, Noorhamdani N, Ratridewi I, Candradikusuma D, et al. 2017; Intervening with healthcare workers' hand hygiene compliance, knowledge, and perception in a limited-resource hospital in Indonesia: a randomized controlled trial study. Antimicrob Resist Infect Control. 6:23. DOI: 10.1186/s13756-017-0179-y. PMID: 28239452. PMCID: PMC5312519.
Article21. Lee SS, Park SJ, Chung MJ, Lee JH, Kang HJ, Lee JA, et al. 2014; Improved hand hygiene compliance is associated with the change of perception toward hand hygiene among medical personnel. Infect Chemother. 46:165–71. DOI: 10.3947/ic.2014.46.3.165. PMID: 25298905. PMCID: PMC4189144.
Article22. Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. 2004; Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med. 141:1–8. DOI: 10.7326/0003-4819-141-1-200407060-00008. PMID: 15238364.
Article23. van Dijk MD, Waltmans-den Breejen CM, Vermeeren JMJJ, van den Berg S, van Beeck EF, Vos MC. 2023; Compliance with a novel hand hygiene protocol tailored to non-sterile healthcare workers in the operating theatre. J Hosp Infect. 131:173–80. DOI: 10.1016/j.jhin.2022.10.009. PMID: 36328310.
Article24. Park JH, Kim HS. 2012; The effect of the hand hygiene education program on hand hygiene knowledge, hand hygiene perception, nasal staphylococcus aureus colonization and hand hygiene adherence in nursing students. J Korean Biol Nurs Sci. 14:156–65. DOI: 10.7586/jkbns.2012.14.3.156.
Article25. WHO. Hand hygiene monitoring tools. https://www.who.int/teams/integrated-health-services/infection-prevention-control/hand-hygiene/monitoring-tools. (Updated on 17 January 2021).26. Polit DF, Beck CT. 2006; The content validity index: are you sure you know what's being reported? Critique and recommendations. Res Nurs Health. 29:489–97. DOI: 10.1002/nur.20147. PMID: 16977646.
Article27. George D, Mallery P. 2011. SPSS for Windows step by step: a simple guide and reference, 17.0 update. 10th ed. Allyn & Bacon;Boston: p. 112–120.28. Alshammari M, Reynolds KA, Verhougstraete M, O'Rourke MK. 2018; Comparison of perceived and observed hand hygiene compliance in healthcare workers in MERS-CoV endemic regions. Healthcare (Basel). 6:122. DOI: 10.3390/healthcare6040122. PMID: 30301272. PMCID: PMC6315729.
Article29. Moret L, Tequi B, Lombrail P. 2004; Should self-assessment methods be used to measure compliance with handwashing recommendations? A study carried out in a French university hospital. Am J Infect Control. 32:384–90. DOI: 10.1016/j.ajic.2004.02.004. PMID: 15525912.
Article30. Kim JH, Jeong JS, Kim MN, Park JY, Choi HR. 2014; The Hawthorne effect between covert and overt observations in the monitoring of hand hygiene adherence among healthcare personnel at coronary care unit and cardiac surgery intensive care unit. Korean J Nosocomial Infect Control. 19:20–8. DOI: 10.14192/kjnic.2014.19.1.20.
Article31. Hosseini P, Mundis GM Jr, Eastlack R, Nourian A, Pawelek J, Nguyen S, et al. 2016; Do longer surgical procedures result in greater contamination of surgeons' hands? Clin Orthop Relat Res. 474:1707–13. DOI: 10.1007/s11999-016-4832-1. PMID: 27090260. PMCID: PMC4887375.
Article32. Pittet D. 2000; Improving compliance with hand hygiene in hospitals. Infect Control Hosp Epidemiol. 21:381–6. DOI: 10.1086/501777. PMID: 10879568.
Article33. Oh HS. 2019; Knowledge, perception, performance, and attitude regarding hand hygiene and related factors among infection control nurses in South Korea: a cross-sectional study. Am J Infect Control. 47:258–63. DOI: 10.1016/j.ajic.2018.09.006. PMID: 30415804. PMCID: PMC7124298.
Article34. Schneider J, Moromisato D, Zemetra B, Rizzi-Wagner L, Rivero N, Mason W, et al. 2009; Hand hygiene adherence is influenced by the behavior of role models. Pediatr Crit Care Med. 10:360–3. DOI: 10.1097/PCC.0b013e3181a32f16. PMID: 19325501.
Article35. Munoz-Price LS, Riley B, Banks S, Eber S, Arheart K, Lubarsky DA, et al. 2014; Frequency of interactions and hand disinfections among anesthesiologists while providing anesthesia care in the operating room: induction versus maintenance. Infect Control Hosp Epidemiol. 35:1056–9. DOI: 10.1086/677154. PMID: 25026624.
Article36. Rose L, Rogel K, Redl L, Cade JF. 2009; Implementation of a multimodal infection control program during an Acinetobacter outbreak. Intensive Crit Care Nurs. 25:57–63. DOI: 10.1016/j.iccn.2008.09.002. PMID: 18952433.
Article37. Erasmus V, Daha TJ, Brug H, Richardus JH, Behrendt MD, Vos MC, et al. 2010; Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 31:283–94. DOI: 10.1086/650451. PMID: 20088678.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Hawthorne Effect on the Adherence to Hand Hygiene
- Healthcare Workers’ Knowledge and Attitudes Regarding the World Health Organization’s “My 5 Moments for Hand Hygiene”: Evidence From a Vietnamese Central General Hospital
- Survey for Hygiene Behavior on Healthcare Personnel by Hygiene Inventory 23
- Factors Influencing Care workers’ Intention of Implementing Hand Hygiene in Long-term Care Hospitals
- The Hawthorne Effect between Covert and Overt Observations in the Monitoring of Hand Hygiene Adherence among Healthcare Personnel at Coronary Care Unit and Cardiac Surgery Intensive Care Unit