J Korean Med Sci.
2023 May;38(21):e168. 10.3346/jkms.2023.38.e168.
Developing and Establishing a Wound Dressing Team: Experience and Recommendations
- Affiliations
-
- 1Department of Plastic Surgery, Korea University College of Medicine, Seoul, Korea
- 2Diabetic Wound Center, Korea University Guro Hospital, Seoul, Korea
- 3Department of Nursing Service, Korea University Guro Hospital, Seoul, Korea
- KMID: 2542603
- DOI: http://doi.org/10.3346/jkms.2023.38.e168
Abstract
- Background
The existing literature has comprehensively examined the benefits of specialized wound-care services and multidisciplinary team care. However, information on the development and integration of wound-dressing teams for patients who do not require specialized wound care is scarce. Therefore, the present study aimed to elucidate the benefits of a wound-dressing team by reporting our experiences with the establishment of a wounddressing team.
Methods
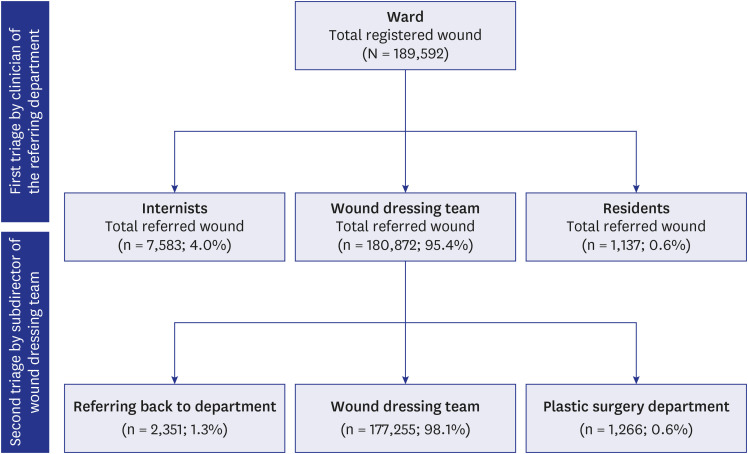
The wound-dressing team was established at Korea University Guro Hospital. Between July 2018 and June 2022, 180,872 cases were managed for wounds at the wounddressing team. The data were analyzed to assess the types of wounds and their outcomes. In addition, questionnaires assessing the satisfaction with the service were administered to patients, ward nurses, residents/internists, and team members.
Results
Regarding the wound type, 80,297 (45.3%) were catheter-related, while 48,036 (27.1%), 26,056 (14.7%), and 20,739 (11.7%) were pressure ulcers, dirty wounds, and simple wounds, respectively. In the satisfaction survey, the scores of the patient, ward nurse, dressing team nurse, and physician groups were 8.9, 8.1, 8.2, and 9.1, respectively. Additionally, 136 dressing-related complications (0.08%) were reported.
Conclusion
The wound dressing team can enhance satisfaction among patients and healthcare providers with low complications. Our findings may provide a potential framework for establishing similar service models.
Figure
Reference
-
1. Nowossadeck E, Prütz F, Teti A. Population change and the burden of hospitalization in Germany 2000-2040: decomposition analysis and projection. PLoS One. 2020; 15(12):e0243322. PMID: 33306705.2. Lee JK, Kwak BO, Choi JH, Choi EH, Kim JH, Kim DH. Financial burden of hospitalization of children with coronavirus disease 2019 under the national health insurance service in Korea. J Korean Med Sci. 2020; 35(24):e224. PMID: 32567260.3. Namgoong S, Han SK. Status of wound management in Korea. Wound Repair Regen. 2018; 26(Suppl 1):S3–S8. PMID: 28857399.4. Hughes R. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD, USA: Agency for Healthcare Research and Quality;2008.5. Posnett J, Gottrup F, Lundgren H, Saal G. The resource impact of wounds on health-care providers in Europe. J Wound Care. 2009; 18(4):154–161. PMID: 19349935.6. Lee JH. Socioeconomic effects of pressure ulcer. J Korean Med Assoc. 2021; 64(1):11–15.7. Järbrink K, Ni G, Sönnergren H, Schmidtchen A, Pang C, Bajpai R, et al. Prevalence and incidence of chronic wounds and related complications: a protocol for a systematic review. Syst Rev. 2016; 5(1):152. PMID: 27609108.8. Kim JY, Pak CS, Park JH, Jeong JH, Heo CY. Effects of polydeoxyribonucleotide in the treatment of pressure ulcers. J Korean Med Sci. 2014; 29(Suppl 3):Suppl 3. S222–S227. PMID: 25473213.9. Olsson M, Järbrink K, Divakar U, Bajpai R, Upton Z, Schmidtchen A, et al. The humanistic and economic burden of chronic wounds: a systematic review. Wound Repair Regen. 2019; 27(1):114–125. PMID: 30362646.10. Eom YH, Kim GY, Jung SS, Lee KY, Kang SB, Bae JS, et al. Present condition analysis of physician assistant in Korea. J Korean Med Sci. 2012; 27(9):981–986. PMID: 22969241.11. You HJ, Han SK. Cell therapy for wound healing. J Korean Med Sci. 2014; 29(3):311–319. PMID: 24616577.12. Jung SY, Lee MJ, Lee SY, Lee SY. The current status of bacterial identification by wound culture for diabetic foot lesions in a single tertiary hospital in South Korea. J Korean Foot Ankle Soc. 2021; 25(2):100–107.13. Son ST, Han SK, Lee TY, Namgoong S, Dhong ES. The microbiology of diabetic foot infections in Korea. J Wound Manag Res. 2017; 13(1):8–12.14. Son JW, Han SK, Namgoong S, Jeong SH, Dhong ES. Bioelectric dressing on skin graft donor sites: a pilot clinical trial. J Wound Manag Res. 2022; 18(2):92–97.15. Ahn J, Park HY, Shetty AA, Hwang W. Use of injectable acellular dermal matrix combined with negative pressure wound therapy in open diabetic foot amputation. J Wound Care. 2022; 31(4):310–320. PMID: 35404696.16. Smith G, Greenwood M, Searle R. Ward nurses’ use of wound dressings before and after a bespoke education programme. J Wound Care. 2010; 19(9):396–402. PMID: 20852568.17. Sood A, Granick MS, Tomaselli NL. Wound dressings and comparative effectiveness data. Adv Wound Care (New Rochelle). 2014; 3(8):511–529. PMID: 25126472.18. Cowman S, Gethin G, Clarke E, Moore Z, Craig G, Jordan-O’Brien J, et al. An international eDelphi study identifying the research and education priorities in wound management and tissue repair. J Clin Nurs. 2012; 21(3-4):344–353. PMID: 22151150.19. Kim H. Wound dressing materials: the essentials. J Wound Manag Res. 2018; 14(2):141–142.20. Han SK. Innovations and Advances in Wound Healing. Berlin, Germany: Springer;2015.21. Sohn S, Seo Y, Jeong Y, Lee S, Lee J, Lee KJ. Changes in the working conditions and learning environment of medical residents after the enactment of the Medical Resident Act in Korea in 2015: a national 4-year longitudinal study. J Educ Eval Health Prof. 2021; 18:7. PMID: 33873263.22. Oh SH, Kim JS. Changes in the training conditions of residents by enforcement of Medical Residents Act. J Digit Converg. 2019; 17(12):427–434.23. Oh SH, Kim JS, Lee PS. A survey on training and working conditions of residents in 2015. J Korean Med Assoc. 2015; 58(12):1179–1189.24. Jones V, Grey JE, Harding KG. Wound dressings. BMJ. 2006; 332(7544):777–780. PMID: 16575081.25. Tan BK, Tan EW, Chong SJ, Chang YY, Colin S, Lee VJ. An economic evaluation of chronic wound management in a tertiary hospital. Wound Pract Res. 2016; 24(3):130–136.26. Wu SC, Marston W, Armstrong DG. Wound care: the role of advanced wound-healing technologies. J Am Podiatr Med Assoc. 2010; 100(5):385–394. PMID: 20847352.27. Boateng J, Catanzano O. Advanced therapeutic dressings for effective wound healing - a review. J Pharm Sci. 2015; 104(11):3653–3680. PMID: 26308473.28. Namgoong S, Jung SY, Han SK, Kim AR, Dhong ES. Clinical experience with surgical debridement and simultaneous meshed skin grafts in treating biofilm-associated infection: an exploratory retrospective pilot study. J Plast Surg Hand Surg. 2020; 54(1):47–54. PMID: 31575315.29. Namgoong S, Yang JP, Yoo KH, Han SK, Rha SW, Lee YN. Comparison of perfusion values after percutaneous transluminal angioplasty according to the severity of ischaemia in the diabetic foot. Int Wound J. 2019; 16(1):176–182. PMID: 30311727.30. Bolton L, McNees P, van Rijswijk L, de Leon J, Lyder C, Kobza L, et al. Wound-healing outcomes using standardized assessment and care in clinical practice. J Wound Ostomy Continence Nurs. 2004; 31(2):65–71. PMID: 15209428.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Selection of dressing materials in chronic wound management
- The Effectiveness of a Dressing Method using Nanocrystalline Silver for Chronic Wounds
- Bioelectric Dressing on Skin Graft Donor Sites: A Pilot Clinical Trial
- Effective Dressing Considering Adhesion and Absorptance in Treatment of Second Degree Facial Burn
- Role of the Surgical Glove in Modified Vacuum-Assisted Wound Healing