Ann Hepatobiliary Pancreat Surg.
2023 May;27(2):180-188. 10.14701/ahbps.22-111.
Radical surgery for stage IV gallbladder cancers: Treatment strategies in patients with limited metastatic burden
- Affiliations
-
- 1Gastrointestinal and Hepato-Pancreato-Biliary Service, Department of Surgical Oncology, Tata Memorial Centre, Homi Bhabha National Institute, Mumbai, India
- 2Gastrointestinal and Hepato-Pancreato-Biliary Service, Department of Surgical Oncology, Homi Bhabha Cancer Hospital, Varanasi, India
- KMID: 2542582
- DOI: http://doi.org/10.14701/ahbps.22-111
Abstract
- Backgrounds/Aims
The present study looked at the role of radical surgery in gallbladder cancers (GBC) with limited metastatic disease.
Methods
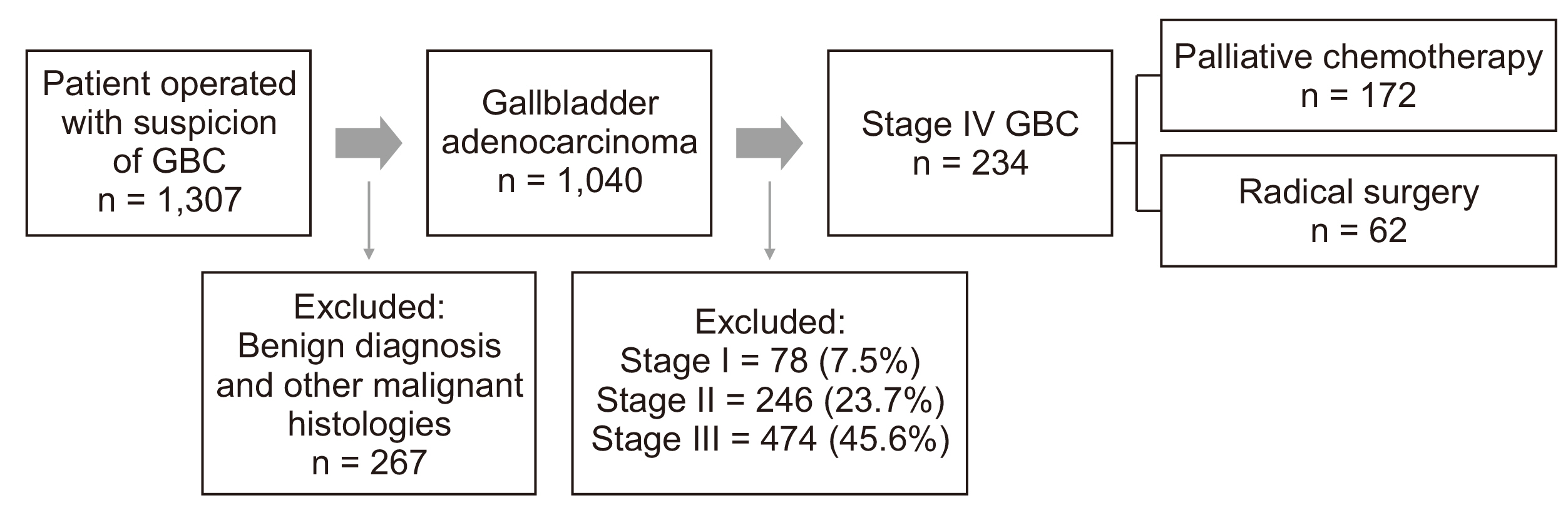
The retrospective observational study was conducted to screen the database from 1st January 2010 to 31st December 2019. Patients of GBC found to have low-volume metastatic disease upon surgical exploration were included.
Results
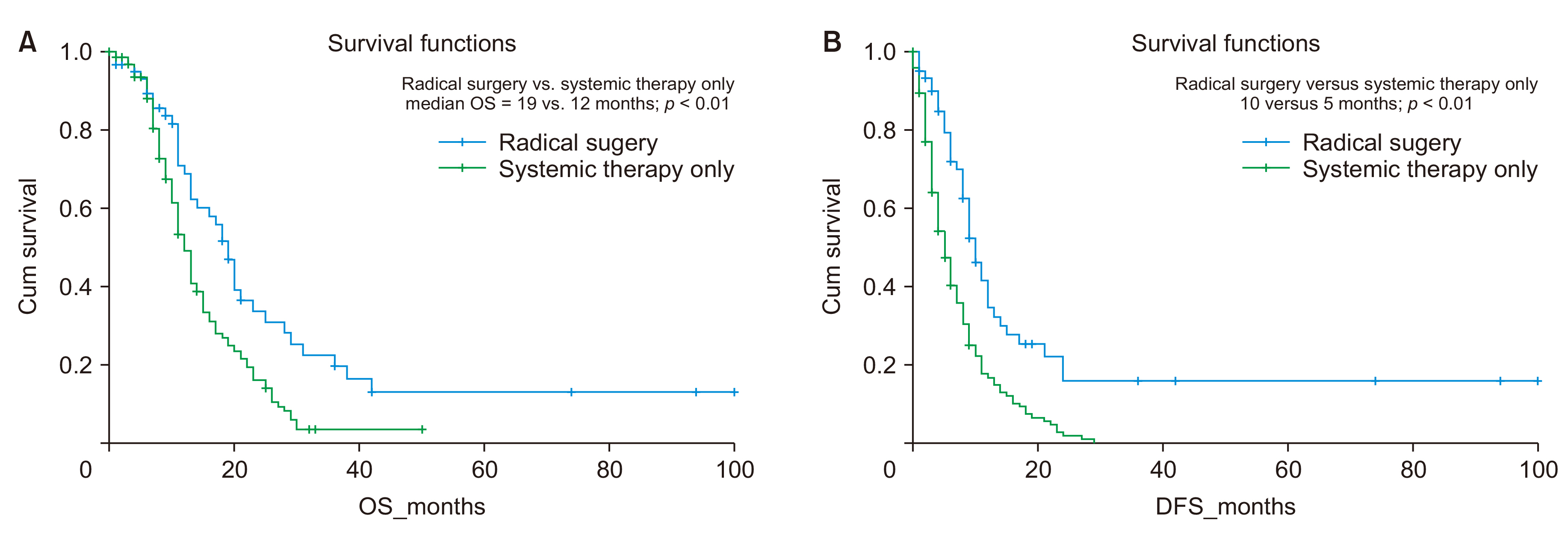
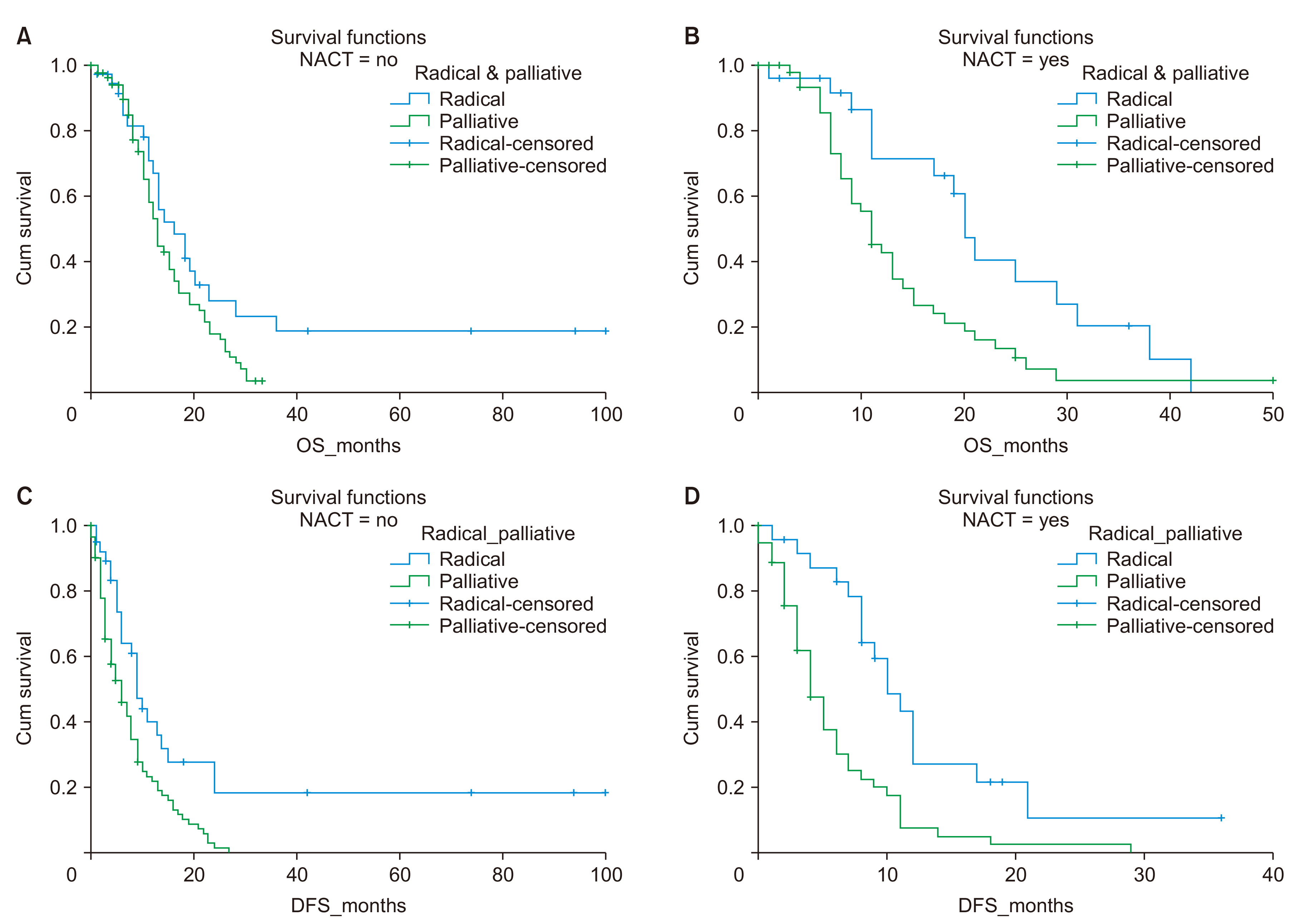
Of the 1,040 patients operated for GBC, 234 patients had low-volume metastatic disease (microscopic disease in station 16b1 node or N2 disease isolated port-site metastases, or low burden peritoneal disease with deposits less than 1 cm, in adjacent omentum or adjacent diaphragm or Morrison’s pouch or a solitary discontinuous liver metastasis in adjacent liver parenchyma) detected intraoperative. Of these, 62 patients underwent radical surgery for R-0 metastatic disease followed by systemic therapy, while the remaining 172 patients did not undergo radical surgery and were given palliative systemic chemotherapy. Patients who underwent radical surgery had significantly superior overall survival (19 months versus 12 months, p < 0.01) and superior progression-free survival (10 months versus 5 months, p < 0.01) when compared to the rest. This difference in survival was more significant amongst patients when operated on after neoadjuvant chemotherapy. Regression analysis showed that a sub-group of patients with incidental GBC with limited metastases showed more favorable outcomes with radical surgery.
Conclusions
Authors suggest a possible role for radical treatment of advanced GBC with a limited metastatic burden. Neoadjuvant chemotherapy can be used for preferentially selecting patients of favorable disease biology for curative treatment.
Keyword
Figure
Reference
-
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–249. DOI: 10.3322/caac.21660. PMID: 33538338.
Article2. Yang Y, Tu Z, Ye C, Cai H, Yang S, Chen X, et al. 2021; Site-specific metastases of gallbladder adenocarcinoma and their prognostic value for survival: a SEER-based study. BMC Surg. 21:59. DOI: 10.1186/s12893-021-01068-8. PMID: 33485332. PMCID: PMC7825172.
Article3. Lee AJ, Chiang YJ, Lee JE, Conrad C, Chun YS, Aloia TA, et al. 2018; Validation of American Joint Committee on Cancer eighth staging system for gallbladder cancer and its lymphadenectomy guidelines. J Surg Res. 230:148–154. DOI: 10.1016/j.jss.2018.04.067. PMID: 30100032.
Article4. Casabianca AS, Tsagkalidis V, Burchard PR, Chacon A, Melucci A, Reitz A, et al. 2022; Surgery in combination with systemic chemotherapy is associated with improved survival in stage IV gallbladder cancer. Eur J Surg Oncol. 48:2448–2454. DOI: 10.1016/j.ejso.2022.06.029. PMID: 35773092.
Article5. Patel S, Patkar S, Goel M. 2022; Radical treatment for stage IV gallbladder cancers: is surgery a worthwhile exercise in advanced cancers? Eur J Surg Oncol. 48:2572–2573. DOI: 10.1016/j.ejso.2022.08.019. PMID: 36064633.
Article6. Carlson RV, Boyd KM, Webb DJ. 2004; The revision of the Declaration of Helsinki: past, present and future. Br J Clin Pharmacol. 57:695–713. DOI: 10.1111/j.1365-2125.2004.02103.x. PMID: 15151515. PMCID: PMC1884510.
Article7. Chaudhari VA, Ostwal V, Patkar S, Sahu A, Toshniwal A, Ramaswamy A, et al. 2018; Outcome of neoadjuvant chemotherapy in "locally advanced/borderline resectable" gallbladder cancer: the need to define indications. HPB (Oxford). 20:841–847. DOI: 10.1016/j.hpb.2018.03.008. PMID: 29706425.
Article8. Goel M, Tamhankar A, Rangarajan V, Patkar S, Ramadwar M, Shrikhande SV. 2016; Role of PET CT scan in redefining treatment of incidental gall bladder carcinoma. J Surg Oncol. 113:652–658. DOI: 10.1002/jso.24198. PMID: 26847023.
Article9. Patkar S, Patel S, Gupta A, Ramaswamy A, Ostwal V, Goel M. 2021; Revision surgery for incidental gallbladder cancer-challenging the dogma: ideal timing and real-world applicability. Ann Surg Oncol. 28:6758–6766. DOI: 10.1245/s10434-021-09687-4. PMID: 33625635.
Article10. Patkar S, Patil V, Acharya MR, Kurunkar S, Goel M. 2019; Achieving margin negative resection-doing less is justified: oncological outcomes of wedge excision of liver in gallbladder cancer (GBC) surgery. Chin Clin Oncol. 8:38. DOI: 10.21037/cco.2019.07.07. PMID: 31431034.
Article11. Pandey D. 2012; Technical description of a regional lymphadenectomy in radical surgery for gallbladder cancer. HPB (Oxford). 14:216–219. DOI: 10.1111/j.1477-2574.2011.00430.x. PMID: 22321041. PMCID: PMC3371205.
Article12. Kurahara H, Maemura K, Mataki Y, Sakoda M, Iino S, Kawasaki Y, et al. 2018; Indication of extrahepatic bile duct resection for gallbladder cancer. Langenbecks Arch Surg. 403:45–51. DOI: 10.1007/s00423-017-1620-7. PMID: 28875312.
Article13. Shukla PJ, Barreto SG. 2010; Systematic review: should routine resection of the extra-hepatic bile duct be performed in gallbladder cancer? Saudi J Gastroenterol. 16:161–167. DOI: 10.4103/1319-3767.65184. PMID: 20616410. PMCID: PMC3003211.
Article14. Ethun CG, Postlewait LM, Le N, Pawlik TM, Poultsides G, Tran T, et al. 2017; Routine port-site excision in incidentally discovered gallbladder cancer is not associated with improved survival: a multi-institution analysis from the US Extrahepatic Biliary Malignancy Consortium. J Surg Oncol. 115:805–811. DOI: 10.1002/jso.24591. PMID: 28230242. PMCID: PMC5800745.
Article15. Amin MB, Edge SB, Greene FL, Byrd DR, Brookland RK, Washington MK, et al. AJCC cancer staging manual. 8th ed. Springer;2017.16. Ostwal V, Swami R, Patkar S, Majumdar S, Goel M, Mehta S, et al. 2018; Gemcitabine-cisplatin (GC) as adjuvant chemotherapy in resected stage II and stage III gallbladder cancers (GBC): a potential way forward. Med Oncol. 35:57. DOI: 10.1007/s12032-018-1115-6. PMID: 29564657.
Article17. Edge S, Byrd D, Compton C, Fritz A, Greene F, Trotti A. 2010. AJCC cancer staging handbook. 7th ed. Springer-Verlag;p. 97–100.18. Shirai Y, Sakata J, Wakai T, Ohashi T, Ajioka Y, Hatakeyama K. 2012; Assessment of lymph node status in gallbladder cancer: location, number, or ratio of positive nodes. World J Surg Oncol. 10:87. DOI: 10.1186/1477-7819-10-87. PMID: 22594526. PMCID: PMC3532237.
Article19. Wi Y, Woo H, Won YJ, Jang JY, Shin A. 2018; Trends in gallbladder cancer incidence and survival in Korea. Cancer Res Treat. 50:1444–1451. DOI: 10.4143/crt.2017.279. PMID: 29370591. PMCID: PMC6192934.
Article20. Ishihara S, Horiguchi A, Miyakawa S, Endo I, Miyazaki M, Takada T. Biliary tract cancer registry in Japan from 2008 to 2013. J Hepatobiliary Pancreat Sci. 2016; 23:149–157. DOI: 10.1002/jhbp.314. PMID: 26699688.
Article21. Singh A, Ghosh NK, Rahul R, Kapoor VK, Saxena R. 2021; Retroperitoneal lymph node metastasis in gallbladder cancer: as bad as distant metastasis. Ann Hepatobiliary Pancreat Surg. 25(Suppl 1):S324. DOI: 10.14701/ahbps.EP-126.
Article22. Maker AV, Butte JM, Oxenberg J, Kuk D, Gonen M, Fong Y, et al. 2012; Is port site resection necessary in the surgical management of gallbladder cancer? Ann Surg Oncol. 19:409–417. DOI: 10.1245/s10434-011-1850-9. PMID: 21698501.
Article23. Hellman S, Weichselbaum RR. 1995; Oligometastases. J Clin Oncol. 13:8–10. DOI: 10.1200/JCO.1995.13.1.8. PMID: 7799047.
Article24. Weichselbaum RR, Hellman S. 2011; Oligometastases revisited. Nat Rev Clin Oncol. 8:378–382. DOI: 10.1038/nrclinonc.2011.44. PMID: 21423255.
Article25. Kuipers H, de Savornin Lohman EAJ, van Dooren M, Braat AE, Daams F, van Dam R, et al. 2021; Extended resections for advanced gallbladder cancer: results from a Nationwide Cohort Study. Ann Surg Oncol. 28:835–843. DOI: 10.1245/s10434-020-08858-z. PMID: 32696306. PMCID: PMC7801314.
Article26. Goel M, Gupta AM, Patkar S, Parray AM, Shetty N, Ramaswamy A, et al. 2021; Towards standardization of management of gallbladder carcinoma with obstructive jaundice: analysis of 113 cases over 10 years at a single institution. J Surg Oncol. 124:572–580. DOI: 10.1002/jso.26564. PMID: 34106475.
Article27. De Lorenzo S, Garajova I, Stefanini B, Tovoli F. 2021; Targeted therapies for gallbladder cancer: an overview of agents in preclinical and clinical development. Expert Opin Investig Drugs. 30:759–772. DOI: 10.1080/13543784.2021.1928636. PMID: 33966562.
Article28. Ahn S, Lee JC, Shin DW, Kim J, Hwang JH. 2020; High PD-L1 expression is associated with therapeutic response to pembrolizumab in patients with advanced biliary tract cancer. Sci Rep. 10:12348. Erratum in: Sci Rep 2020;10:21552. DOI: 10.1038/s41598-020-69366-4. PMID: 32704067. PMCID: PMC7378166.
Article29. Das CK, Patel A, Raj A, Gupta VG, Mehta P, Bhethanabhotla S, et al. 2020; Anti-Her2neu directed therapy in advanced gall bladder cancer: a prospective, multicenter experience from India. J Clin Oncol. 38(15 Suppl):e16682. DOI: 10.1200/JCO.2020.38.15_suppl.e16682.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radical Surgery for Carcinoma of the Gallbladder
- Surgical Outcomes and Prognostic Factors of Primary Gallbladder Carcinoma
- Analysis of Clinical Outcome and Prognostic Factors in Patients with Gallbladder Cancer
- Metastatic Gallbladder Cancer Treated with Curative Surgery after Cyclic Chemotherapy and Biliary Drainage
- A Case of Metastatic Malignant Melanoma of the Gallbladder