Arch Hand Microsurg.
2023 Jun;28(2):119-124. 10.12790/ahm.21.0145.
An ancient schwannoma misdiagnosed as a dermoid cyst on ultrasound examination: a case report
- Affiliations
-
- 1Department of Orthopaedic Surgery, CHA Gumi Medical Center, CHA University School of Medicine, Gumi, Korea
- 2Department of Orthopaedic Surgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- KMID: 2542564
- DOI: http://doi.org/10.12790/ahm.21.0145
Abstract
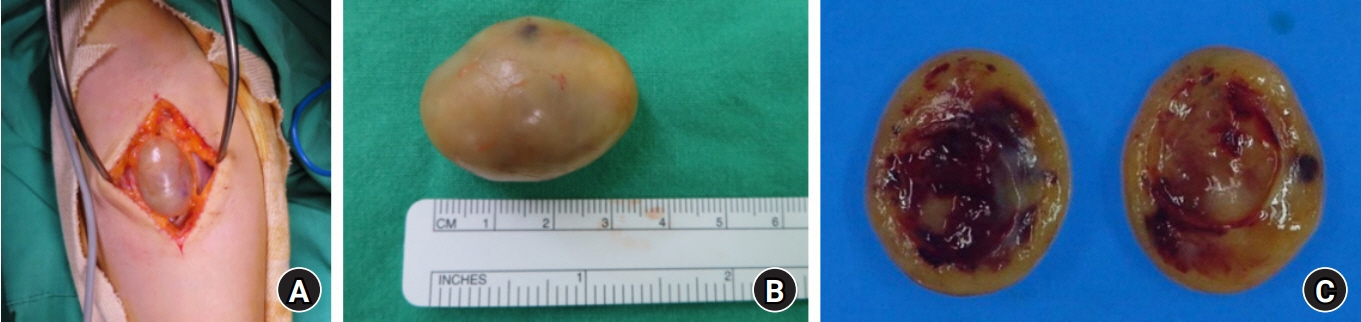
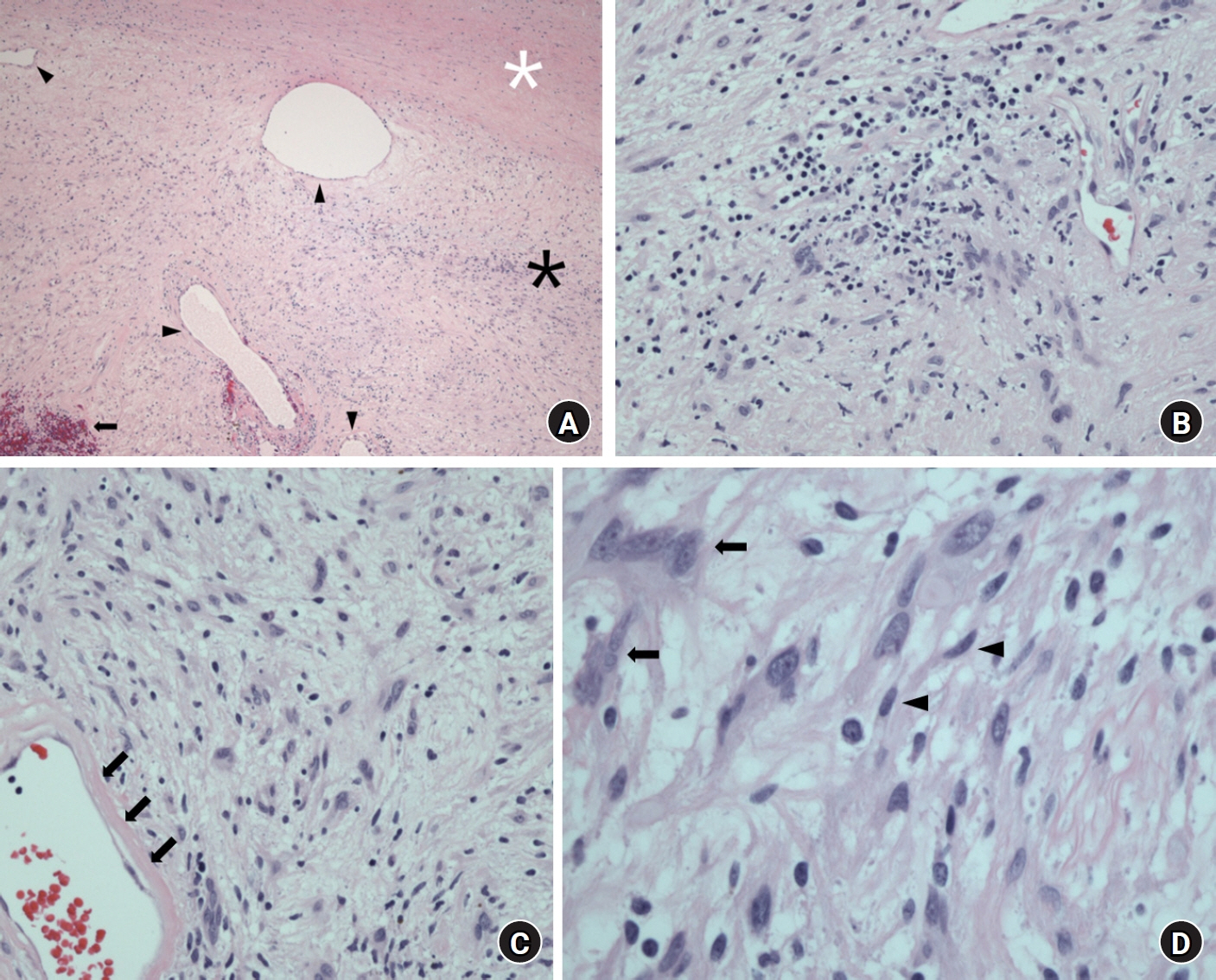
- Ancient schwannomas are benign, long-standing schwannomas of the neural sheaths. This schwannoma subtype is characterized by cystic and hemorrhagic changes. These degenerative changes are thought to result from the tumor’s long-term progression and have the potential to be misdiagnosed as other soft tissue tumors or sarcomas. A 37-year-old female patient presented to our department with discomfort caused by a mass on the anterior side of her forearm. Approximately 2 weeks prior to her visit, an excisional biopsy was attempted under local anesthesia, but the patient experienced severe tingling sensations up to the wrist during surgery, preventing successful removal of the mass. Ultrasonography and magnetic resonance imaging (MRI) were performed for further differential diagnosis. An excisional biopsy was performed under general anesthesia, and histologic analysis revealed typical degenerative features of ancient schwannoma. A thorough examination, including MRI, is necessary to identify these tumors, prevent potential misdiagnosis, and ensure appropriate treatment.
Figure
Reference
-
References
1. Weiss SW GJ, Enzinger FM. Enzinger and Weiss’s soft tissue tumours. 4th ed. St. Louis: Mosby;2001. p. 1111–208.2. MacCollin M, Chiocca EA, Evans DG, et al. Diagnostic criteria for schwannomatosis. Neurology. 2005; 64:1838–45.
Article3. Knight DM, Birch R, Pringle J. Benign solitary schwannomas: a review of 234 cases. J Bone Joint Surg Br. 2007; 89:382–7.4. Hide IG, Baudouin CJ, Murray SA, Malcolm AJ. Giant ancient schwannoma of the pelvis. Skeletal Radiol. 2000; 29:538–42.
Article5. Schultz E, Sapan MR, McHeffey-Atkinson B, Naidich JB, Arlen M. Case report 872. “Ancient” schwannoma (degenerated neurilemoma). Skeletal Radiol. 1994; 23:593–5.6. Yasumatsu R, Nakashima T, Miyazaki R, Segawa Y, Komune S. Diagnosis and management of extracranial head and neck schwannomas: a review of 27 cases. Int J Otolaryngol. 2013; 2013:973045.
Article7. Koga H, Matsumoto S, Manabe J, Tanizawa T, Kawaguchi N. Definition of the target sign and its use for the diagnosis of schwannomas. Clin Orthop Relat Res. 2007; 464:224–9.
Article8. Vilanova JR, Burgos-Bretones JJ, Alvarez JA, Rivera-Pomar JM. Benign schwannomas: a histopathological and morphometric study. J Pathol. 1982; 137:281–6.
Article9. Ackerman LV, Taylor FH. Neurogenous tumors within the thorax: a clinicopathological evaluation of forty-eight cases. Cancer. 1951; 4:669–91.
Article10. Rockwell GM, Thoma A, Salama S. Schwannoma of the hand and wrist. Plast Reconstr Surg. 2003; 111:1227–32.
Article