Arch Hand Microsurg.
2023 Jun;28(2):106-109. 10.12790/ahm.23.0010.
Reconstruction of a soft tissue defect in the toe using a serratus anterior fascia free flap: a case report
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2542561
- DOI: http://doi.org/10.12790/ahm.23.0010
Abstract
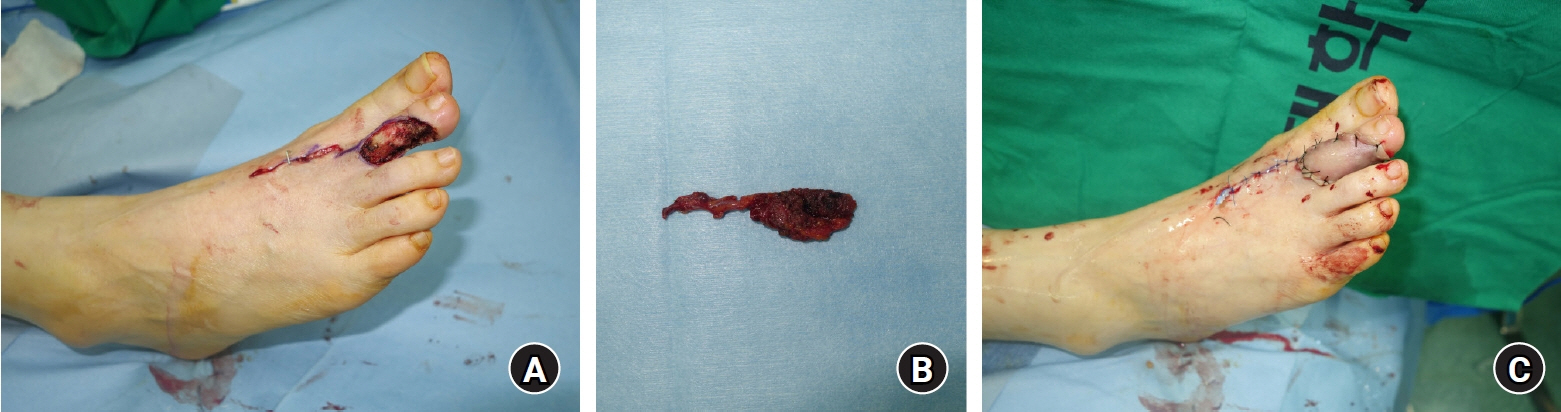
- Toe injuries frequently occur as traumatic or oncologic defects. Compared with finger reconstruction, toe reconstruction has been rarely reported in the literature, because of the difficulty of toes’ relatively thin soft tissue envelope, their requirement for relatively challenging surgical techniques, and the slight improvements in gait. Therefore, toe reconstruction can be challenging for plastic surgeons, especially in cases with exposure of a tendon, bone, or joint. Herein, we present a case study of a 54-year-old woman with squamous cell carcinoma in situ (Bowen disease) that subsequently resulted in a defect on her second toe. A serratus anterior fascia free flap could be a good option for toe reconstruction due to its large caliber, lengthy pedicle, relatively easy dissection, and thin muscle bulk. We present our unique experience using the serratus anterior fascia free flap for the reconstruction of an oncologic toe defect.
Figure
Reference
-
References
1. Kwon SH, Lao W, Yen CI, Lin YT, Wu KP, Chang TN. Aesthetic multiple-toe reconstruction with combined iliac bone graft and wraparound free anterolateral thigh flap-a case report and literature review. Ann Plast Surg. 2017; 78(3 Suppl 2):S37–40.
Article2. Cheng LF, Lee JT, Wu MS. Lateral toe pulp flap used in reconstruction of distal dorsal toe defect: case report and review of the literature. Ann Plast Surg. 2019; 82(1S Suppl 1):S136–9.3. Karir A, Stein MJ, Shiga S, Zhang J. Reconstruction of lower extremity defects using the serratus anterior free flap: a systematic review and retrospective case series. J Reconstr Microsurg. 2020; 36:116–26.
Article4. Covello GS, Martins DV, Padilha GC, Cavalheiro CS, Vieira LA, Caetano EB. Serratus anterior muscle flap for reconstruction of extremity injuries. Acta Ortop Bras. 2022; 30(spe1):e250673.
Article5. Kim YH, Kim KH, Sung KY, Kim JT, Kim SW. Toe resurfacing with a thin thoracodorsal artery perforator flap. Microsurgery. 2017; 37:312–8.
Article6. Lee KT, Park BY, Kim EJ, et al. Superthin SCIP flap for reconstruction of subungual melanoma: aesthetic functional surgery. Plast Reconstr Surg. 2017; 140:1278–89.
Article7. Glass GE, Staruch RM, Sivakumar B, Stotland MA. Thin and superthin free flaps: an innovative approach to pediatric extremity reconstruction. J Plast Reconstr Aesthet Surg. 2022; 75:3970–8.
Article8. Moris V, Cristofari S, Stivala A, et al. Fluorescent indocyanine green angiography: preliminary results in microsurgery monitoring. J Stomatol Oral Maxillofac Surg. 2019; 120:297–300.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of soft tissue defects using free serratus anterior muscle and adifofascial flap
- Reconstruction of various sized soft tissue or compound tissue defect using free serratus anterior muscle or composite flap
- Reconstruction of the Hand Using Fabricated Great Toe Pulp and Anterolateral Thigh Chimeric Free Flap
- Usefullness of Chimeric Flaps Based on the Subscapular Vascular System
- Reconstruction of a skull base defect with cutaneous nasocranial communication using a combination of an anterolateral thigh free flap and galeal flap division: a case report