Clin Endosc.
2023 May;56(3):340-352. 10.5946/ce.2022.166.
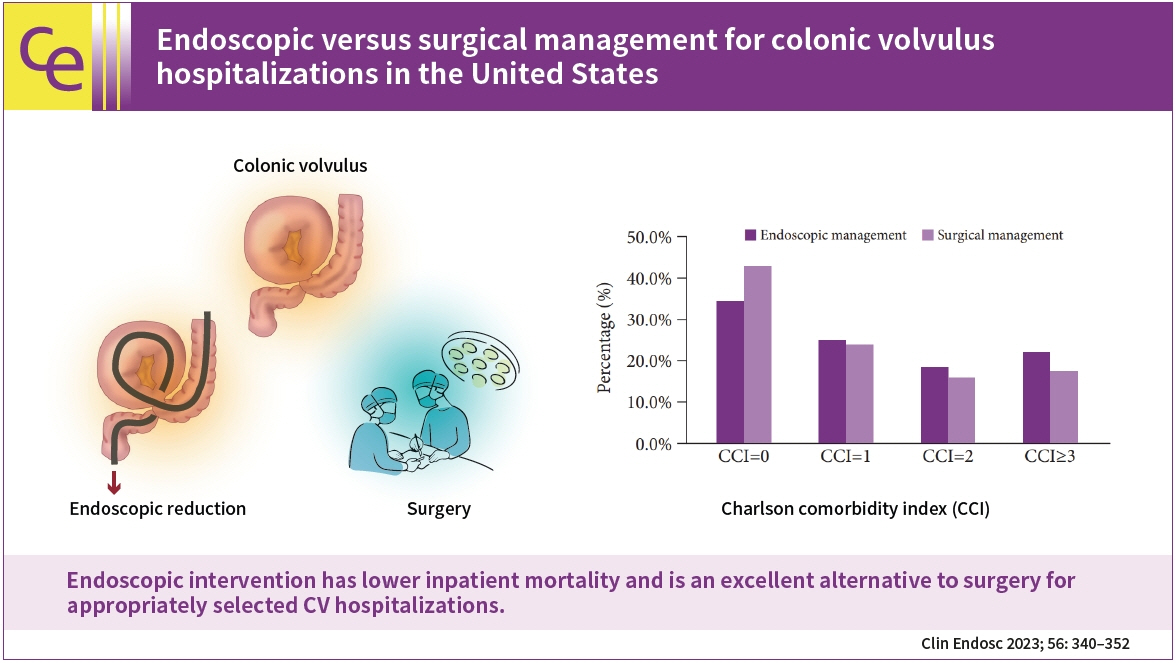
Endoscopic versus surgical management for colonic volvulus hospitalizations in the United States
- Affiliations
-
- 1Department of Internal Medicine, Central Michigan University College of Medicine, Saginaw, MI, USA
- 2Department of Gastroenterology, Parkview Cancer Institute, Fort Wayne, IN, USA
- 3The Wright Center for Graduate Medical Education, Scranton, PA, USA
- 4Department of Internal Medicine, Mercer University School of Medicine, Macon, GA, USA
- 5Department of Gastroenterology and Hepatology, University of Arkansas for Medical Sciences, Little Rock, AR, USA
- 6Department of Gastroenterology, Hepatology and Nutrition, Cleveland Clinic Foundation, Cleveland, OH, USA
- 7Department of Statistics, Actuarial and Data Science, Central Michigan University, Mt. Pleasant, MI, USA
- 8Division of Gastroenterology and Hepatology, Indiana University School of Medicine, Indianapolis, IN, USA
- 9Division of Interventional Oncology and Surgical Endoscopy (IOSE), Parkview Cancer Institute, Fort Wayne, IN, USA
- KMID: 2542462
- DOI: http://doi.org/10.5946/ce.2022.166
Abstract
- Background/Aims
Colonic volvulus (CV), a common cause of bowel obstruction, often requires intervention. We aimed to identify hospitalization trends and CV outcomes in the United States.
Methods
We used the National Inpatient Sample to identify all adult CV hospitalizations in the United States from 2007 to 2017. Patient demographics, comorbidities, and inpatient outcomes were highlighted. Outcomes of endoscopic and surgical management were compared.
Results
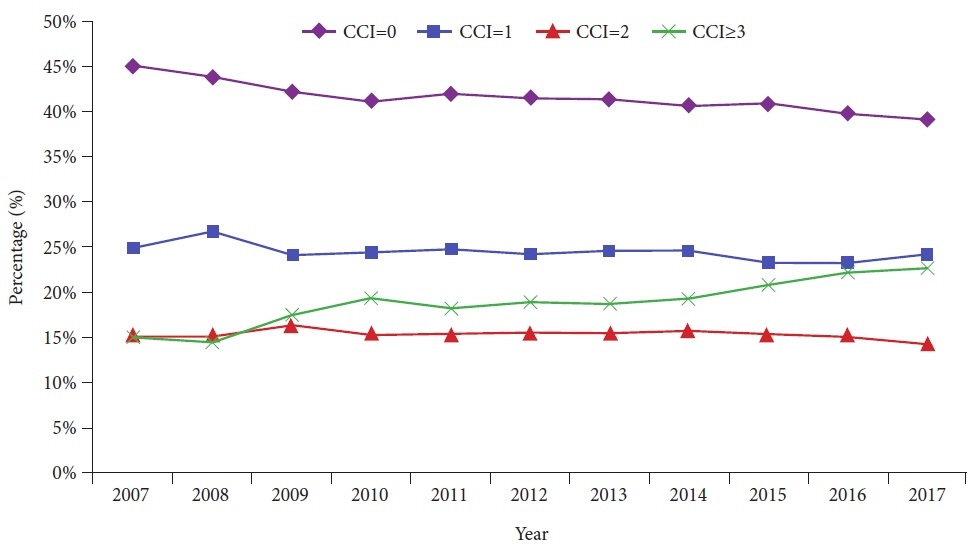
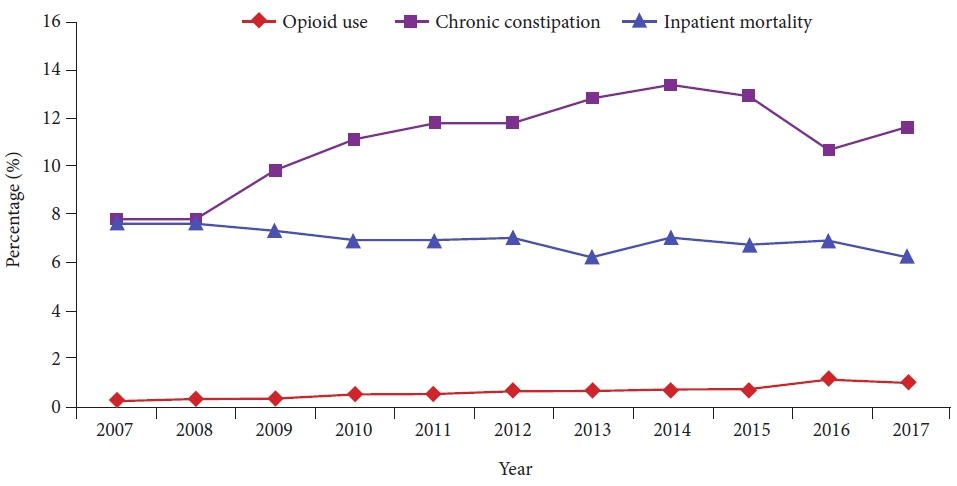
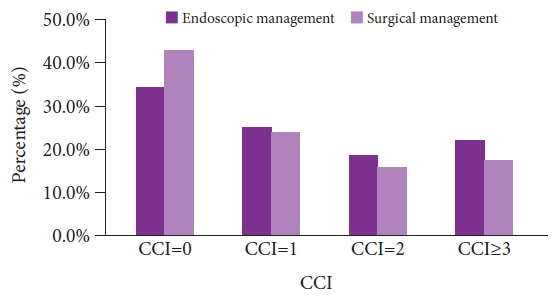
From 2007 to 2017, there were 220,666 CV hospitalizations. CV-related hospitalizations increased from 17,888 in 2007 to 21,715 in 2017 (p=0.001). However, inpatient mortality decreased from 7.6% in 2007 to 6.2% in 2017 (p<0.001). Of all CV-related hospitalizations, 13,745 underwent endoscopic intervention, and 77,157 underwent surgery. Although the endoscopic cohort had patients with a higher Charlson comorbidity index, we noted lower inpatient mortality (6.1% vs. 7.0%, p<0.001), mean length of stay (8.3 vs. 11.8 days, p<0.001), and mean total healthcare charge ($68,126 vs. $106,703, p<0.001) compared to the surgical cohort. Male sex, increased Charlson comorbidity index scores, acute kidney injury, and malnutrition were associated with higher odds of inpatient mortality in patients with CV who underwent endoscopic management.
Conclusions
Endoscopic intervention has lower inpatient mortality and is an excellent alternative to surgery for appropriately selected CV hospitalizations.
Keyword
Figure
Reference
-
1. Hiltunen KM, Syrjä H, Matikainen M. Colonic volvulus. Diagnosis and results of treatment in 82 patients. Eur J Surg. 1992; 158:607–611.2. Margolin DA, Whitlow CB. The pathogenesis and etiology of colonic volvulus. Semin Colon Rectal Surg. 2007; 18:79–86.3. Gingold D, Murrell Z. Management of colonic volvulus. Clin Colon Rectal Surg. 2012; 25:236–244.4. Oren D, Atamanalp SS, Aydinli B, et al. An algorithm for the management of sigmoid colon volvulus and the safety of primary resection: experience with 827 cases. Dis Colon Rectum. 2007; 50:489–497.5. Perrot L, Fohlen A, Alves A, et al. Management of the colonic volvulus in 2016. J Visc Surg. 2016; 153:183–192.6. Naveed M, Jamil LH, Fujii-Lau LL, et al. American Society for Gastrointestinal Endoscopy guideline on the role of endoscopy in the management of acute colonic pseudo-obstruction and colonic volvulus. Gastrointest Endosc. 2020; 91:228–235.7. Halabi WJ, Jafari MD, Kang CY, et al. Colonic volvulus in the United States: trends, outcomes, and predictors of mortality. Ann Surg. 2014; 259:293–301.8. Healthcare Cost and Utilization Project (HCUP). Introduction to the HCUP National Inpatient Sample (NIS) [Internet]. HCUP;2018. [cited 2022 Sep 10]. Available from: https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2018.jsp.9. Houchens R, Ross D, Elixhauser A, et al. Nationwide Inpatient Sample (NIS) redesign final report (2014). HCUP Methods Series [Internet]. US Agency for Healthcare Research and Quality;2014. [cited 2022 Sep 10]. Available from: http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp.10. Bauman ZM, Evans CH. Volvulus. Surg Clin North Am. 2018; 98:973–993.11. Gonzalez-Urquijo M, Rodarte-Shade M, Gil-Galindo G. Acute colonic volvulus in a Mexican population: a case series. Ann Coloproctol. 2020; 36:48–53.12. Chokhavatia S, John ES, Bridgeman MB, et al. Constipation in elderly patients with noncancer pain: focus on opioid-induced constipation. Drugs Aging. 2016; 33:557–574.13. Firat N, Mantoglu B, Ozdemir K, et al. Endoscopic detorsion results in sigmoid volvulus: single-center experience. Emerg Med Int. 2020; 2020:1473580.14. Lou Z, Yu ED, Zhang W, et al. Appropriate treatment of acute sigmoid volvulus in the emergency setting. World J Gastroenterol. 2013; 19:4979–4983.15. Helgeland J, Skyrud K, Lindahl AK, et al. Benchmarking of abdominal surgery: a study evaluating the HARM score in a European national cohort. BJS Open. 2020; 4:637–644.16. Lal SK, Morgenstern R, Vinjirayer EP, et al. Sigmoid volvulus an update. Gastrointest Endosc Clin N Am. 2006; 16:175–187.17. Ifversen AK, Kjaer DW. More patients should undergo surgery after sigmoid volvulus. World J Gastroenterol. 2014; 20:18384–18389.18. Atamanalp SS. Comments on "Endoscopic management of sigmoid volvulus in a debilitated population: what relevance?". GE Port J Gastroenterol. 2021; 28:374–375.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Sigmoid Volvulus Treated by Emergency Endoscopic Reduction and Surgical Colonic Resection
- A Case Report of a Rare Aetiology of a Sigmoid Volvulus Involving a Congenital Omental Defect
- Laparoscopic Management of Sigmoid Volvulus for Which Endoscopic Reduction had Failed
- Transverse Colon Volvulus around the Gastrostomy Tube in a Pediatric Situs Inversus Patient
- A Case of Gastric Volvulus Reduced by Endoscope