J Korean Assoc Oral Maxillofac Surg.
2023 Apr;49(2):100-104. 10.5125/jkaoms.2023.49.2.100.
A ramus cortical bone harvesting technique without bone marrow invasion
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Dentistry and Institute of Oral Bioscience, Research Institute of Clinical Medicine of Jeonbuk National University, Jeonju, Korea
- 2Biomedical Research Institute of Jeonbuk National University Hospital, Jeonbuk National University, Jeonju, Korea
- 3Department of Mechanical and Design Engineering, Wonkwang University, Iksan, Korea
- KMID: 2542217
- DOI: http://doi.org/10.5125/jkaoms.2023.49.2.100
Abstract
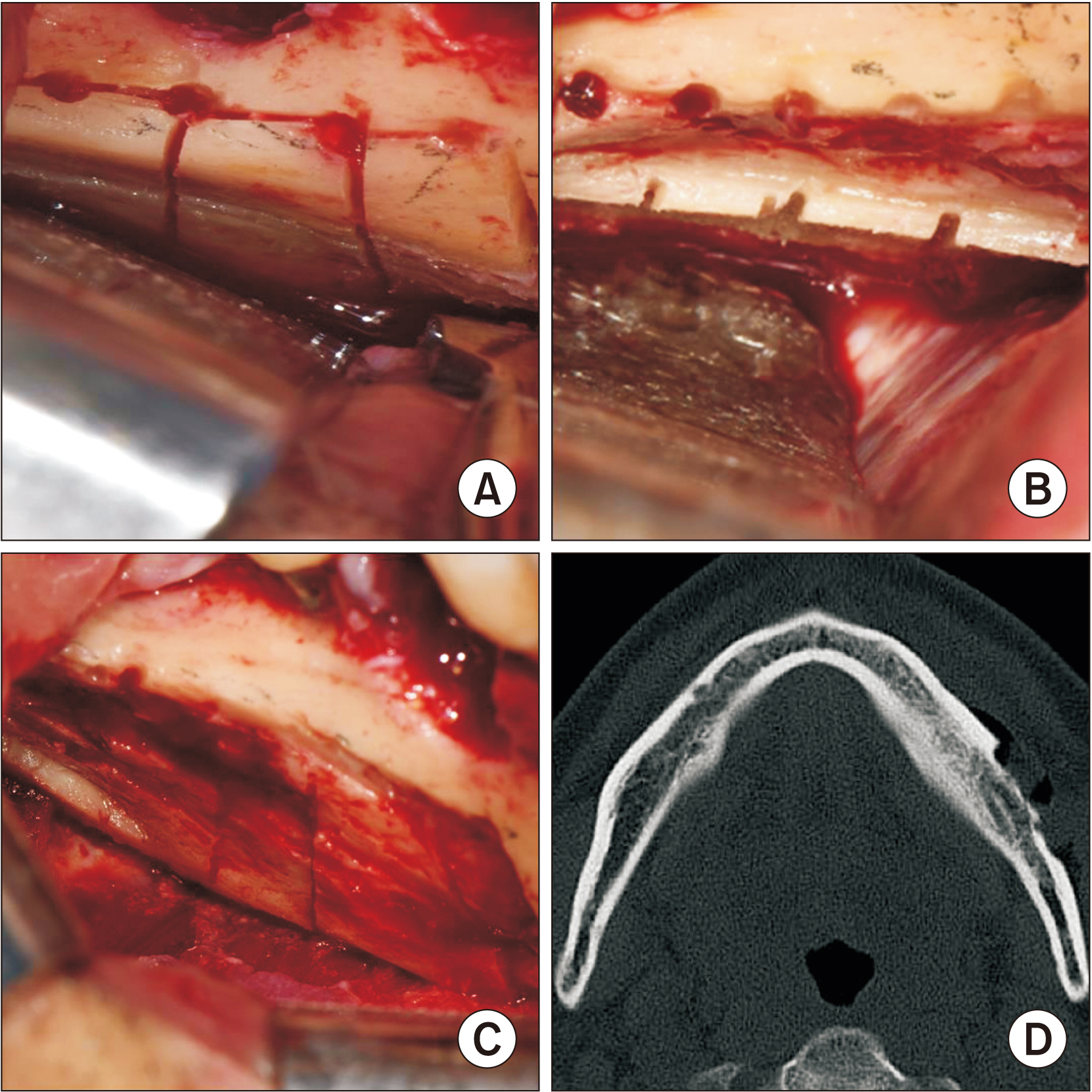
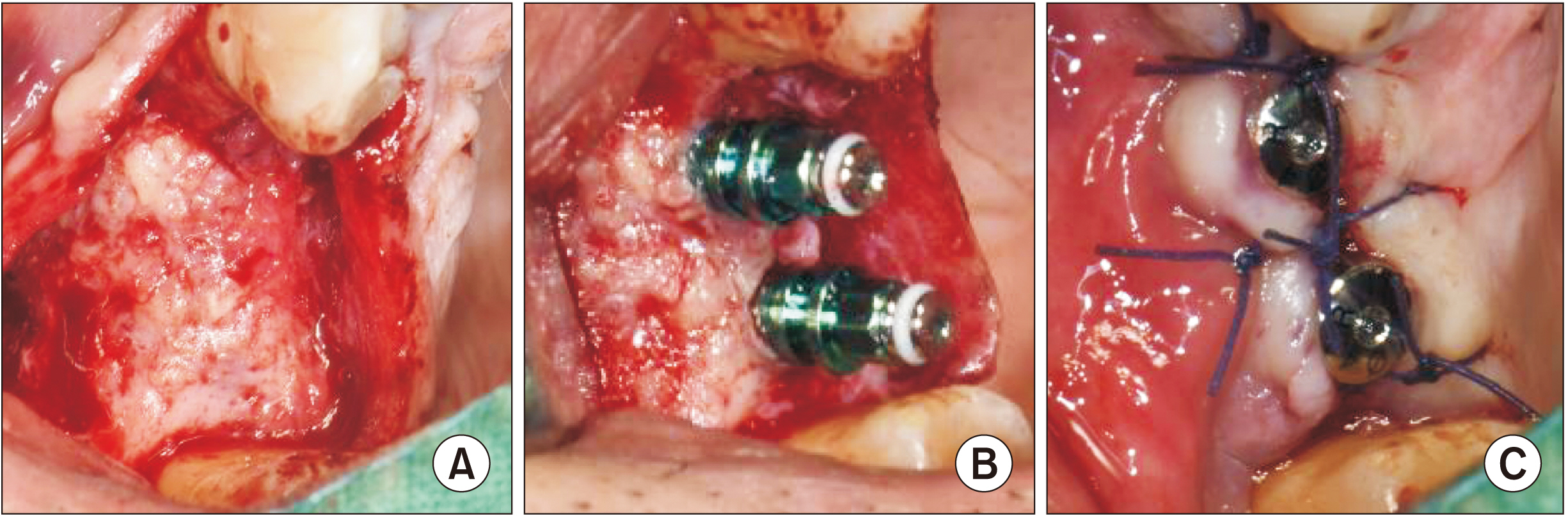
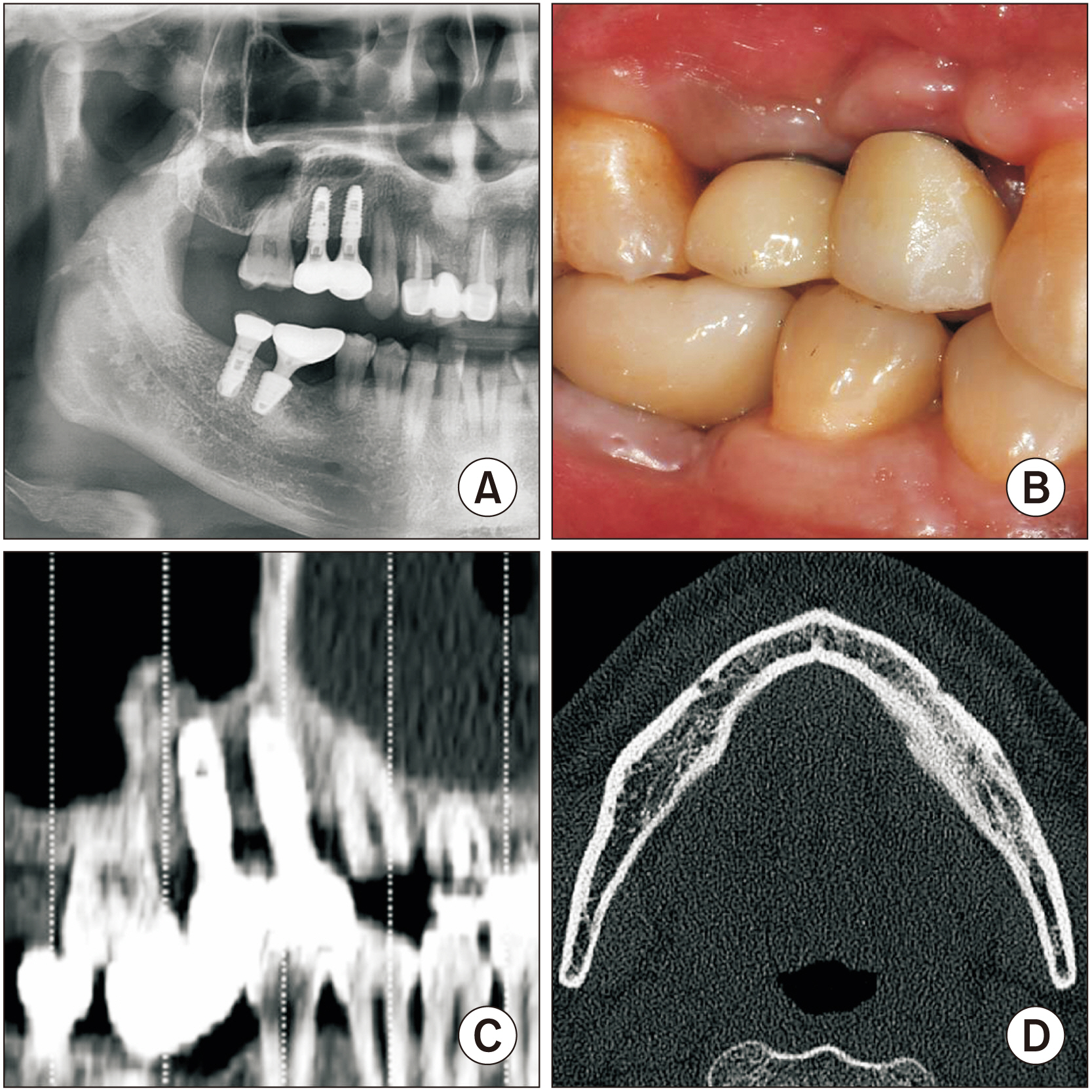
- Autogenous bone grafts from the mandibular ramus are a known source of inadequate bone volume scenarios of the residual alveolar ridge. However, the conventional block-type harvesting technique cannot prevent bone marrow invasion, which can cause postoperative complications such as pain, swelling, and inferior alveolar nerve injury. This study aims to suggest a complication-free harvesting technique and present the results of bone grafting and donor sites. One patient received two dental implants with a complication-free harvesting technique that involves creation of ditching holes with a 1 mm round bur. Sagittal, coronal, and axial osteotomies produced grid-type cortical squares using a micro-saw and a round bur to confirm the cortical thickness. The grid-type cortical bone was harvested from the occlusal aspect, and the harvesting was extended through an additional osteotomy on the exposed and remaining cortical bone to prevent bone marrow invasion. The patient did not suffer postoperative severe pain, swelling, or numbness. After 15 months, the harvested site exhibited new cortical bone lining, and the grafted area had healed to a cortico-cancellous complex with functional loading of the implants. Our technique, grid-type cortical bone harvesting without bone marrow invasion, allowed application of autogenous bone without bone marrow invasion to achieve acceptable bone healing of the dental implants and to regenerate the harvested cortical bone.
Keyword
Figure
Reference
-
References
1. Kim YK, Ku JK. 2020; Ridge augmentation in implant dentistry. J Korean Assoc Oral Maxillofac Surg. 46:211–7. https://doi.org/10.5125/jkaoms.2020.46.3.211. DOI: 10.5125/jkaoms.2020.46.3.211. PMID: 32606284. PMCID: PMC7338632.
Article2. Bell RB, Blakey GH, White RP, Hillebrand DG, Molina A. 2002; Staged reconstruction of the severely atrophic mandible with autogenous bone graft and endosteal implants. J Oral Maxillofac Surg. 60:1135–41. https://doi.org/10.1053/joms.2002.34986. DOI: 10.1053/joms.2002.34986. PMID: 12378486.
Article3. Jang K, Lee JH, Oh SH, Ham BD, Chung SM, Lee JK, et al. 2020; Bone graft materials for current implant dentistry. J Dent Implant Res. 39:1–10. https://doi.org/10.54527/jdir.2020.39.1.1. DOI: 10.54527/jdir.2020.39.1.1.
Article4. Rogers GF, Greene AK. 2012; Autogenous bone graft: basic science and clinical implications. J Craniofac Surg. 23:323–7. https://doi.org/10.1097/scs.0b013e318241dcba. DOI: 10.1097/SCS.0b013e318241dcba. PMID: 22337435.
Article5. Zins JE, Whitaker LA. 1983; Membranous versus endochondral bone: implications for craniofacial reconstruction. Plast Reconstr Surg. 72:778–85. https://doi.org/10.1097/00006534-198312000-00005. DOI: 10.1097/00006534-198312000-00005. PMID: 6196801.
Article6. Lee HG, Kim YD. 2015; Volumetric stability of autogenous bone graft with mandibular body bone: cone-beam computed tomography and three-dimensional reconstruction analysis. J Korean Assoc Oral Maxillofac Surg. 41:232–9. https://doi.org/10.5125/jkaoms.2015.41.5.232. DOI: 10.5125/jkaoms.2015.41.5.232. PMID: 26568924. PMCID: PMC4641213.
Article7. Cha HS, Kim JW, Hwang JH, Ahn KM. 2016; Frequency of bone graft in implant surgery. Maxillofac Plast Reconstr Surg. 38:19. https://doi.org/10.1186/s40902-016-0064-2. DOI: 10.1186/s40902-016-0064-2. PMID: 27077072. PMCID: PMC4819798.
Article8. Güngörmüş M, Yavuz MS. 2002; The ascending ramus of the mandible as a donor site in maxillofacial bone grafting. J Oral Maxillofac Surg. 60:1316–8. https://doi.org/10.1053/joms.2002.35731. DOI: 10.1053/joms.2002.35731. PMID: 12420267.
Article9. Reininger D, Cobo-Vázquez C, Monteserín-Matesanz M, López-Quiles J. 2016; Complications in the use of the mandibular body, ramus and symphysis as donor sites in bone graft surgery. A systematic review. Med Oral Patol Oral Cir Bucal. 21:e241–9. https://doi.org/10.4317/medoral.20938. DOI: 10.4317/medoral.20938. PMID: 26827063. PMCID: PMC4788806.
Article10. Hwang KG, Shim KS, Yang SM, Park CJ. 2008; Partial-thickness cortical bone graft from the mandibular ramus: a non-invasive harvesting technique. J Periodontol. 79:941–4. https://doi.org/10.1902/jop.2008.070408. DOI: 10.1902/jop.2008.070408. PMID: 18454675.
Article11. Bayome M, Park JH, Kook YA. 2013; New three-dimensional cephalometric analyses among adults with a skeletal class I pattern and normal occlusion. Korean J Orthod. 43:62–73. https://doi.org/10.4041/kjod.2013.43.2.62. DOI: 10.4041/kjod.2013.43.2.62. PMID: 23671831. PMCID: PMC3650215.
Article12. Clavero J, Lundgren S. 2003; Ramus or chin grafts for maxillary sinus inlay and local onlay augmentation: comparison of donor site morbidity and complications. Clin Implant Dent Relat Res. 5:154–60. https://doi.org/10.1111/j.1708-8208.2003.tb00197.x. DOI: 10.1111/j.1708-8208.2003.tb00197.x. PMID: 14575631.
Article13. Kim SG, Song JY, Lee YC. 2011; Modified veneer bone graft with the concomitant installation of a dental implant: technical note. Oral Maxillofac Surg. 15:189–92. https://doi.org/10.1007/s10006-011-0271-z. DOI: 10.1007/s10006-011-0271-z. PMID: 21503623.
Article14. Leong DJ, Li J, Moreno I, Wang HL. 2010; Distance between external cortical bone and mandibular canal for harvesting ramus graft: a human cadaver study. J Periodontol. 81:239–43. https://doi.org/10.1902/jop.2009.090417. DOI: 10.1902/jop.2009.090417. PMID: 20151802.
Article15. Doh RM, Shin S, You TM. 2018; Delayed paresthesia of inferior alveolar nerve after dental surgery: case report and related pathophysiology. J Dent Anesth Pain Med. 18:177–82. https://doi.org/10.17245/jdapm.2018.18.3.177. DOI: 10.17245/jdapm.2018.18.3.177. PMID: 29984322. PMCID: PMC6031975.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthetic Management of Healthy Donor for Bone Marrow Harvesting
- A Case of Paturient Bone Marrow Harvest Under General Anesthesia
- Effect of Bone Marrow Exposure in Rabbit Skull Osteogenesis
- An experimental study on the bone regeneration of tibial bone defect
- Bone Marrow Examination: Adventures in Diagnostic Hematology