J Korean Neurosurg Soc.
2023 May;66(3):298-307. 10.3340/jkns.2023.0020.
Perspectives : Understanding the Pathophysiology of Intraventricular Hemorrhage in Preterm Infants and Considering of the Future Direction for Treatment
- Affiliations
-
- 1Department of Neurosurgery and Children’s Medical Center, Nara Medical University, Kashihara, Japan
- KMID: 2542015
- DOI: http://doi.org/10.3340/jkns.2023.0020
Abstract
- Remarkable advances in neonatal care have significantly improved the survival of extremely low birth weight infants in recent years. However, intraventricular hemorrhage (IVH) continues to be a major complication in preterm infants, leading to a high incidence of cerebral palsy and cognitive impairment. IVH is primarily caused by disruption of the fragile vascular network of the subependymal germinal matrix, and subsequent ventricular dilatation adversely affects the developing infant brain. Based on recent research, periventricular white matter injury is caused not only by ischemia and morphological distortion due to ventricular dilatation but also by free iron and inflammatory cytokines derived from hematoma and its lysates. The current guidelines for the treatment of posthemorrhagic hydrocephalus (PHH) in preterm infants do not provide strong recommendations, but initiating treatment intervention based on ultrasound measurement values before the appearance of clinical symptoms of PHH has been proposed. Moreover, in the past decade, therapeutic interventions that actively remove hematomas and lysates have been introduced. The era is moving beyond cerebrospinal fluid shunt toward therapeutic goals aimed at improving neurodevelopmental outcomes.
Figure
Reference
-
References
1. Adams-Chapman I, Hansen NI, Stoll BJ, Higgins R; NICHD Research Network. Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics. 121:e1167–e1177. 2008.
Article2. Ahn SY, Chang YS, Park WS. Mesenchymal stem cells transplantation for neuroprotection in preterm infants with severe intraventricular hemorrhage. Korean J Pediatr. 57:251–256. 2014.
Article3. Ahn SY, Chang YS, Sung SI, Park WS. Mesenchymal stem cells for severe intraventricular hemorrhage in preterm infants: phase I doseescalation clinical trial. Stem Cells Transl Med. 7:847–856. 2018.
Article4. Ahn SY, Sung DK, Kim YE, Sung S, Chang YS, Park WS. Brain-derived neurotropic factor mediates neuroprotection of mesenchymal stem cellderived extracellular vesicles against severe intraventricular hemorrhage in newborn rats. Stem Cells Transl Med. 10:374–384. 2021.
Article5. Back SA, Gan X, Li Y, Rosenberg PA, Volpe JJ. Maturation-dependent vulnerability of oligodendrocytes to oxidative stress-induced death caused by glutathione depletion. J Neurosci. 18:6241–6253. 1998.
Article6. Back SA, Luo NL, Borenstein NS, Levine JM, Volpe JJ, Kinney HC. Late oligodendrocyte progenitors coincide with the developmental window of vulnerability for human perinatal white matter injury. J Neurosci. 21:1302–1312. 2001.
Article7. Badhiwala JH, Hong CJ, Nassiri F, Hong BY, Riva-Cambrin J, Kulkarni AV. Treatment of posthemorrhagic ventricular dilation in preterm infants: a systematic review and meta-analysis of outcomes and complications. J Neurosurg Pediatr. 16:545–555. 2015.
Article8. Ballabh P, de Vries LS. White matter injury in infants with intraventricular haemorrhage: mechanisms and therapies. Nat Rev Neurol. 17:199–214. 2021.
Article9. Behrens P, Tietze A, Walch E, Bittigau P, Bührer C, Schulz M, et al. Neurodevelopmental outcome at 2 years after neuroendoscopic lavage in neonates with posthemorrhagic hydrocephalus. J Neurosurg Pediatr. 26:495–503. 2020.
Article10. Bell EF, Hintz SR, Hansen NI, Bann CM, Wyckoff MH, DeMauro SB, et al. Mortality, in-hospital morbidity, care practices, and 2-year outcomes for extremely preterm infants in the US, 2013-2018. JAMA. 327:248–263. 2022.
Article11. Bolisetty S, Dhawan A, Abdel-Latif M, Bajuk B, Stack J, Lui K, et al. Intraventricular hemorrhage and neurodevelopmental outcomes in extreme preterm infants. Pediatrics. 133:55–62. 2014.
Article12. Brouwer AJ, Groenendaal F, Benders MJ, de Vries LS. Early and late complications of germinal matrix-intraventricular haemorrhage in the preterm infant: what is new? Neonatology. 106:296–303. 2014.
Article13. Brouwer AJ, van Stam C, Uniken Venema M, Koopman C, Groenendaal F, de Vries LS. Cognitive and neurological outcome at the age of 5-8 years of preterm infants with post-hemorrhagic ventricular dilatation requiring neurosurgical intervention. Neonatology. 101:210–216. 2012.
Article14. Chari A, Mallucci C, Whitelaw A, Aquilina K. Intraventricular haemorrhage and posthaemorrhagic ventricular dilatation: moving beyond CSF diversion. Childs Nerv Syst. 37:3375–3383. 2021.
Article15. Christian EA, Melamed EF, Peck E, Krieger MD, McComb JG. Surgical management of hydrocephalus secondary to intraventricular hemorrhage in the preterm infant. J Neurosurg Pediatr. 17:278–284. 2016.
Article16. d’Arcangues C, Schulz M, Bührer C, Thome U, Krause M, Thomale UW. Extended experience with neuroendoscopic lavage for posthemorrhagic hydrocephalus in neonates. World Neurosurg. 116:e217–e224. 2018.
Article17. Deger J, Goethe EA, LoPresti MA, Lam S. Intraventricular hemorrhage in premature infants: a historical review. World Neurosurg. 153:21–25. 2021.
Article18. de Vries LS, Groenendaal F, Liem KD, Heep A, Brouwer AJ, van ‘t Verlaat E, et al. Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 104:F70–F75. 2019.
Article19. de Vries LS, Liem KD, van Dijk K, Smit BJ, Sie L, Rademaker KJ, et al. Early versus late treatment of posthaemorrhagic ventricular dilatation: results of a retrospective study from five neonatal intensive care units in the Netherlands. Acta Paediatr. 91:212–217. 2002.
Article20. Dorner RA, Burton VJ, Allen MC, Robinson S, Soares BP. Preterm neuroimaging and neurodevelopmental outcome: a focus on intraventricular hemorrhage, post-hemorrhagic hydrocephalus, and associated brain injury. J Perinatol. 38:1431–1443. 2018.
Article21. El-Dib M, Limbrick DD Jr, Inder T, Whitelaw A, Kulkarni AV, Warf B, et al. Management of post-hemorrhagic ventricular dilatation in the infant born preterm. J Pediatr. 226:16–27.e3. 2020.22. Fountain DM, Chari A, Allen D, James G. Comparison of the use of ventricular access devices and ventriculosubgaleal shunts in posthaemorrhagic hydrocephalus: systematic review and meta-analysis. Childs Nerv Syst. 32:259–267. 2016.
Article23. Franz AP, Bolat GU, Bolat H, Matijasevich A, Santos IS, Silveira RC, et al. Attention-deficit/hyperactivity disorder and very preterm/very low birth weight: a meta-analysis. Pediatrics. 141:e20171645. 2018.
Article24. Hintz SR, Kendrick DE, Vohr BR, Poole WK, Higgins RD; National Institute of Child Health and Human Development Neonatal Research Network. Changes in neurodevelopmental outcomes at 18 to 22 months’ corrected age among infants of less than 25 weeks’ gestational age born in 1993-1999. Pediatrics. 115:1645–1651. 2005.
Article25. Hollebrandse NL, Spittle AJ, Burnett AC, Anderson PJ, Roberts G, Doyle LW, et al. School-age outcomes following intraventricular haemorrhage in infants born extremely preterm. Arch Dis Child Fetal Neonatal Ed. 106:4–8. 2021.
Article26. Inder TE, Perlman JM, Volpe JJ : Preterm Intraventricular Hemorrhage/Posthemorrhagic Hydrocephalus in Volpe JJ, Inder TE, Barra BT, de Vries LS, du Plessis AJ, Neil JJ, et al. (eds) : Volpe’s Neurology of the Newborn (Sixth Edition). Philadelphia : Elsevier, 2018, pp637-698.27. Indredavik MS, Skranes JS, Vik T, Heyerdahl S, Romundstad P, Myhr GE, et al. Low-birth-weight adolescents: psychiatric symptoms and cerebral MRI abnormalities. Pediatr Neurol. 33:259–266. 2005.
Article28. International PHVD Drug Trial Group. International randomised controlled trial of acetazolamide and furosemide in posthaemorrhagic ventricular dilatation in infancy. Lancet. 352:433–440. 1998.29. Kennedy CR, Ayers S, Campbell MJ, Elbourne D, Hope P, Johnson A. Randomized, controlled trial of acetazolamide and furosemide in posthemorrhagic ventricular dilation in infancy: follow-up at 1 year. Pediatrics. 108:597–607. 2001.
Article30. Kusuda S, Fujimura M, Sakuma I, Aotani H, Kabe K, Itani Y, et al. Morbidity and mortality of infants with very low birth weight in Japan: center variation. Pediatrics. 18:e1130–e1138. 2006.
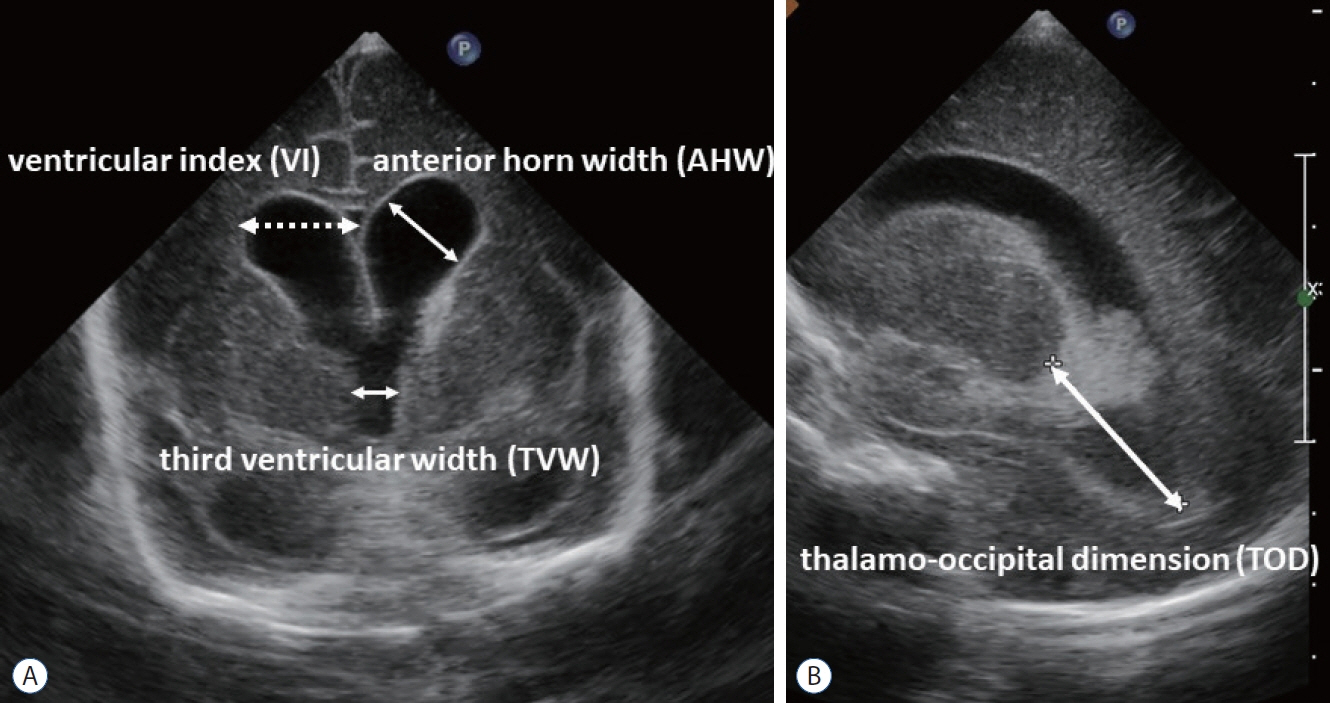
Article31. Langley EA, Blake SM, Coe KL. Recent review of germinal matrix hemorrhage-intraventricular hemorrhage in preterm infants. Neonatal Netw. 41:100–106. 2022.32. Levene MI. Measurement of the growth of the lateral ventricles in preterm infants with real-time ultrasound. Arch Dis Child. 56:900–904. 1981.
Article33. Limbrick DD Jr, de Vries LS. New insights into the management of posthemorrhagic hydrocephalus. Semin Perinatol. 46:151597. 2022.
Article34. Limbrick DD Jr, Mathur A, Johnston JM, Munro R, Sagar J, Inder T, et al. Neurosurgical treatment of progressive posthemorrhagic ventricular dilation in preterm infants: a 10-year single-institution study. J Neurosurg Pediatr. 6:224–230. 2010.
Article35. Luyt K, Jary SL, Lea CL, Young GJ, Odd DE, Miller HE, et al. Drainage, irrigation and fibrinolytic therapy (DRIFT) for posthaemorrhagic ventricular dilatation: 10-year follow-up of a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 105:466–473. 2020.
Article36. Mazzola CA, Choudhri AF, Auguste KI, Limbrick DD Jr, Rogido M, Mitchell L, et al. Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 2: management of posthemorrhagic hydrocephalus in premature infants. J Neurosurg Pediatr 14 Suppl. 1:8–23. 2014.
Article37. McClugage SG, Laskay NMB, Donahue BN, Arynchyna A, Zimmerman K, Aban IB, et al. Functional outcomes at 2 years of age following treatment for posthemorrhagic hydrocephalus of prematurity: what do we know at the time of consult? J Neurosurg Pediatr. 14:1–9. 2020.
Article38. Murphy BP, Inder TE, Rooks V, Taylor GA, Anderson NJ, Mogridge N, et al. Posthaemorrhagic ventricular dilatation in the premature infant: natural history and predictors of outcome. Arch Dis Child Fetal Neonatal Ed. 87:F37–F41. 2002.
Article39. Nosarti C, Giouroukou E, Micali N, Rifkin L, Morris RG, Murray RM. Impaired executive functioning in young adults born very preterm. J Int Neuropsychol Soc. 13:571–581. 2007.
Article40. O’Shea TM, Allred EN, Kuban KC, Hirtz D, Specter B, Durfee S, et al. Intraventricular hemorrhage and developmental outcomes at 24 months of age in extremely preterm infants. J Child Neurol. 27:22–29. 2012.
Article41. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 92:529–534. 1978.
Article42. Park YS. Treatment strategies and challenges to avoid cerebrospinal fluid shunting for pediatric hydrocephalus. Neurol Med Chir (Tokyo). 62:416–430. 2022.
Article43. Park YS, Kotani Y, Kim TK, Yokota H, Sugimoto T, Nakagawa I, et al. Efficacy and safety of intraventricular fibrinolytic therapy for postintraventricular hemorrhagic hydrocephalus in extreme low birth weight infants: a preliminary clinical study. Childs Nerv Syst. 37:69–79. 2021.
Article44. Rees P, Callan C, Chadda KR, Vaal M, Diviney J, Sabti S, et al. Preterm brain injury and neurodevelopmental outcomes: a meta-analysis. Pediatrics. 150:e2022057442. 2022.
Article45. Riva-Cambrin J, Shannon CN, Holubkov R, Whitehead WE, Kulkarni AV, Drake J, et al. Center effect and other factors influencing temporization and shunting of cerebrospinal fluid in preterm infants with intraventricular hemorrhage. J Neurosurg Pediatr. 9:473–481. 2012.
Article46. Robinson S. Neonatal posthemorrhagic hydrocephalus from prematurity: pathophysiology and current treatment concepts. J Neurosurg Pediatr. 9:242–258. 2012.
Article47. Savman K, Nilsson UA, Blennow M, Kjellmer I, Whitelaw A. Non-protein-bound iron is elevated in cerebrospinal fluid from preterm infants with posthemorrhagic ventricular dilatation. Pediatr Res. 49:208–212. 2001.
Article48. Sävman K, Blennow M, Hagberg H, Tarkowski E, Thoresen M, Whitelaw A. Cytokine response in cerebrospinal fluid from preterm infants with posthaemorrhagic ventricular dilatation. Acta Paediatr. 91:1357–1363. 2002.
Article49. Schulz M, Bührer C, Pohl-Schickinger A, Haberl H, Thomale UW. Neuroendoscopic lavage for the treatment of intraventricular hemorrhage and hydrocephalus in neonates. J Neurosurg Pediatr. 13:626–635. 2014.
Article50. Shooman D, Portess H, Sparrow O. A review of the current treatment methods for posthaemorrhagic hydrocephalus of infants. Cerebrospinal Fluid Res. 6:1. 2009.
Article51. Spader HS, Hertzler DA, Kestle JR, Riva-Cambrin J. Risk factors for infection and the effect of an institutional shunt protocol on the incidence of ventricular access device infections in preterm infants. J Neurosurg Pediatr. 15:156–160. 2015.
Article52. Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 314:1039–1051. 2015.
Article53. Szpecht D, Wiak K, Braszak A, Szymankiewicz M, Gadzinowski J. Role of selected cytokines in the etiopathogenesis of intraventricular hemorrhage in preterm newborns. Childs Nerv Syst. 32:2097–2103. 2016.
Article54. Taylor HG, Minich N, Bangert B, Filipek PA, Hack M. Long-term neuropsychological outcomes of very low birth weight: associations with early risks for periventricular brain insults. J Int Neuropsychol Soc. 10:987–1004. 2004.
Article55. Thomale UW, Auer C, Spennato P, Schaumann A, Behrens P, Gorelyshev S, et al. TROPHY registry - status report. Childs Nerv Syst. 37:3549–3554. 2021.
Article56. Thomale UW, Cinalli G, Kulkarni AV, Al-Hakim S, Roth J, Schaumann A, et al. TROPHY registry study design: a prospective, international multicenter study for the surgical treatment of posthemorrhagic hydrocephalus in neonates. Childs Nerv Syst. 35:613–619. 2019.
Article57. Tirado-Caballero J, Rivero-Garvia M, Arteaga-Romero F, Herreria-Franco J, Lozano-Gonzalez Á, Marquez-Rivas J. Neuroendoscopic lavage for the management of posthemorrhagic hydrocephalus in preterm infants: safety, effectivity, and lessons learned. J Neurosurg Pediatr. 26:237–246. 2020.
Article58. Valcamonico A, Accorsi P, Sanzeni C, Martelli P, La Boria P, Cavazza A, et al. Mid- and long-term outcome of extremely low birth weight (ELBW) infants: an analysis of prognostic factors. J Matern Fetal Neonatal Med. 20:465–471. 2007.
Article59. Ventriculomegaly Trial Group. Randomised trial of early tapping in neonatal posthaemorrhagic ventricular dilatation. Arch Dis Child. 65(1 Spec No):3–10. 1990.60. Volpe JJ. Intraventricular hemorrhage in the premature infant--current concepts. Part I. Ann Neurol. 25:3–11. 1989.
Article61. Volpe JJ. Intraventricular hemorrhage in the premature infant--current concepts. Part II. Ann Neurol. 25:109–116. 1989.
Article62. Wang JY, Amin AG, Jallo GI, Ahn ES. Ventricular reservoir versus ventriculosubgaleal shunt for posthemorrhagic hydrocephalus in preterm infants: infection risks and ventriculoperitoneal shunt rate. J Neurosurg Pediatr. 14:447–454. 2014.
Article63. Wellons JC, Shannon CN, Kulkarni AV, Simon TD, Riva-Cambrin J, Whitehead WE, et al. A multicenter retrospective comparison of conversion from temporary to permanent cerebrospinal fluid diversion in very low birth weight infants with posthemorrhagic hydrocephalus. J Neurosurg Pediatr. 4:50–55. 2009.
Article64. Wellons JC 3rd, Shannon CN, Holubkov R, Riva-Cambrin J, Kulkarni AV, Limbrick DD Jr, et al. Shunting outcomes in posthemorrhagic hydrocephalus: results of a Hydrocephalus Clinical Research Network prospective cohort study. J Neurosurg Pediatr. 20:19–29. 2017.
Article65. Whitaker AH, Feldman JF, Lorenz JM, McNicholas F, Fisher PW, Shen S, et al. Neonatal head ultrasound abnormalities in preterm infants and adolescent psychiatric disorders. Arch Gen Psychiatry. 68:742–752. 2011.
Article66. Whitelaw A, Aquilina K. Management of posthaemorrhagic ventricular dilatation. Arch Dis Child Fetal Neonatal Ed. 97:F229–3. 2012.
Article67. Whitelaw A, Evans D, Carter M, Thoresen M, Wroblewska J, Mandera M, et al. Randomized clinical trial of prevention of hydrocephalus after intraventricular hemorrhage in preterm infants: brain-washing versus tapping fluid. Pediatrics. 119:e1071–e1078. 2007.
Article68. Whitelaw A, Jary S, Kmita G, Wroblewska J, Musialik-Swietlinska E, Mandera M, et al. Randomized trial of drainage, irrigation and fibrinolytic therapy for premature infants with posthemorrhagic ventricular dilatation: developmental outcome at 2 years. Pediatrics. 125:e852–e858. 2010.
Article69. Whitelaw A, Lee-Kelland R. Repeated lumbar or ventricular punctures in newborns with intraventricular haemorrhage. Cochrane Database Syst Rev. 4:CD000216. 2017.
Article70. Whitelaw A, Pople I, Cherian S, Evans D, Thoresen M. Phase 1 trial of prevention of hydrocephalus after intraventricular hemorrhage in newborn infants by drainage, irrigation, and fibrinolytic therapy. Pediatrics. 111(4 Pt 1):759–765. 2003.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fibrinolytic (Thrombolytic) Therapy for Post Intraventricular Hemorrhagic Hydrocephalus in Preterm Infants
- Pharmacological Management of Germinal Matrix-Intraventricular Hemorrhage
- Pathogenesis and Prevention of Intraventricular Hemorrhage in Preterm Infants
- Neurodevelopmental Outcomes and Brain Volumetric Analysis of Low-Grade Intraventricular Hemorrhage
- Clinical Applications of Plasma B-type Natriuretic Peptide Assays in Preterm Infants with Patent Ductus Arteriosus