J Korean Neurosurg Soc.
2023 May;66(3):263-273. 10.3340/jkns.2022.0258.
Fibrinolytic (Thrombolytic) Therapy for Post Intraventricular Hemorrhagic Hydrocephalus in Preterm Infants
- Affiliations
-
- 1Department of Neurosurgery and Children’s Medical Center, Nara Medical University, Kashihara, Japan
- KMID: 2542011
- DOI: http://doi.org/10.3340/jkns.2022.0258
Abstract
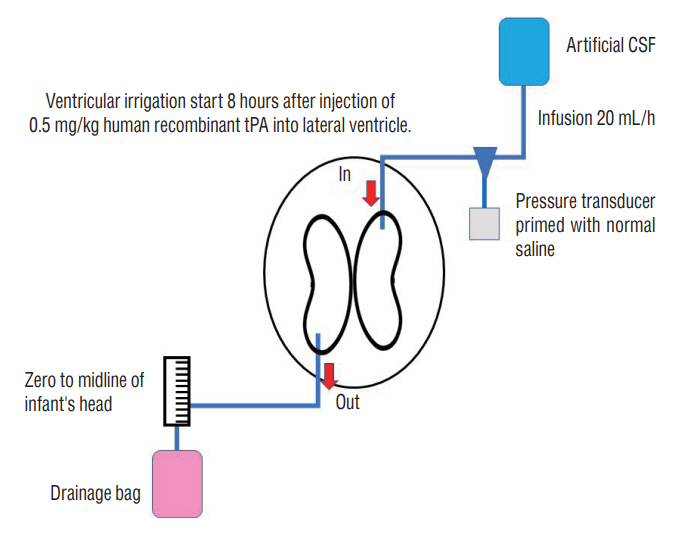
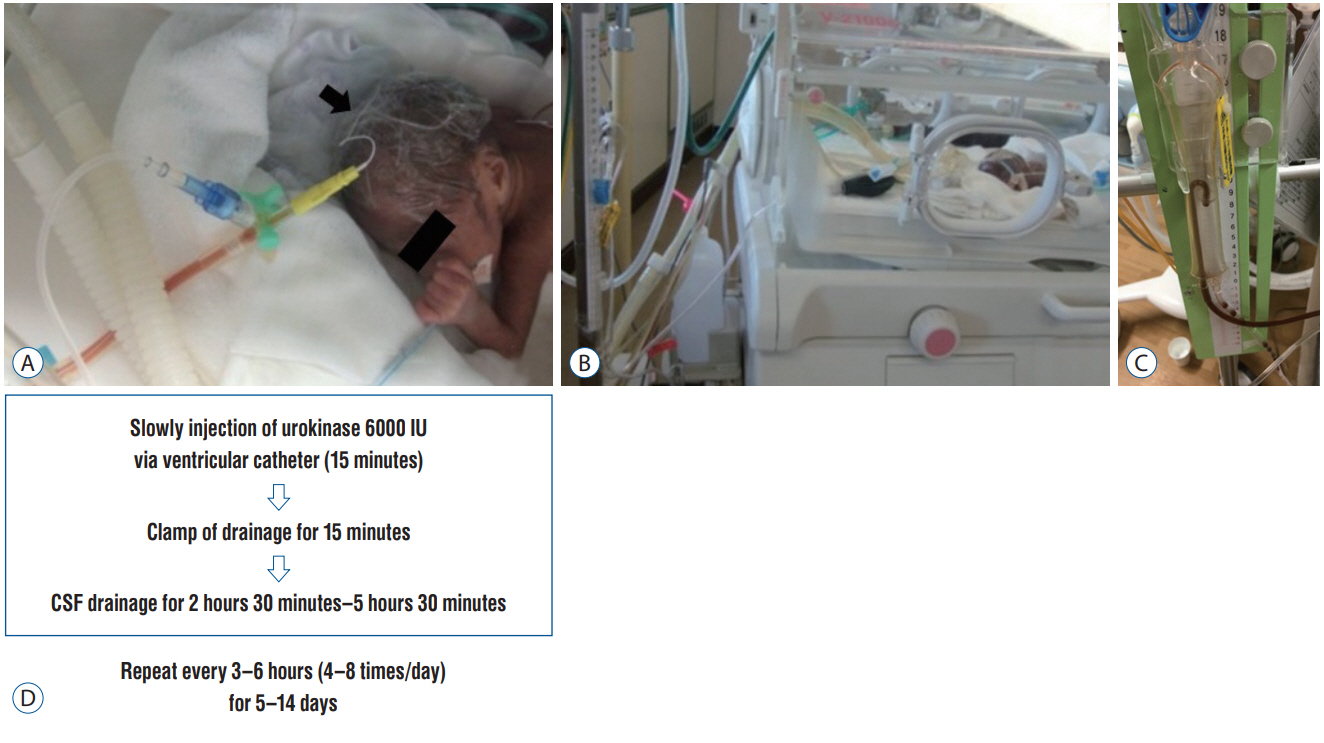
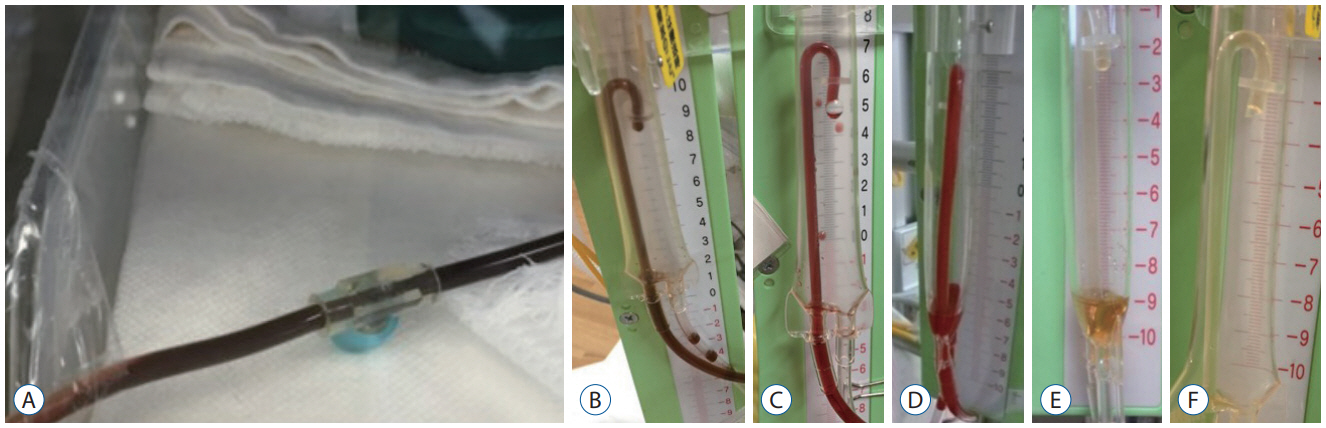
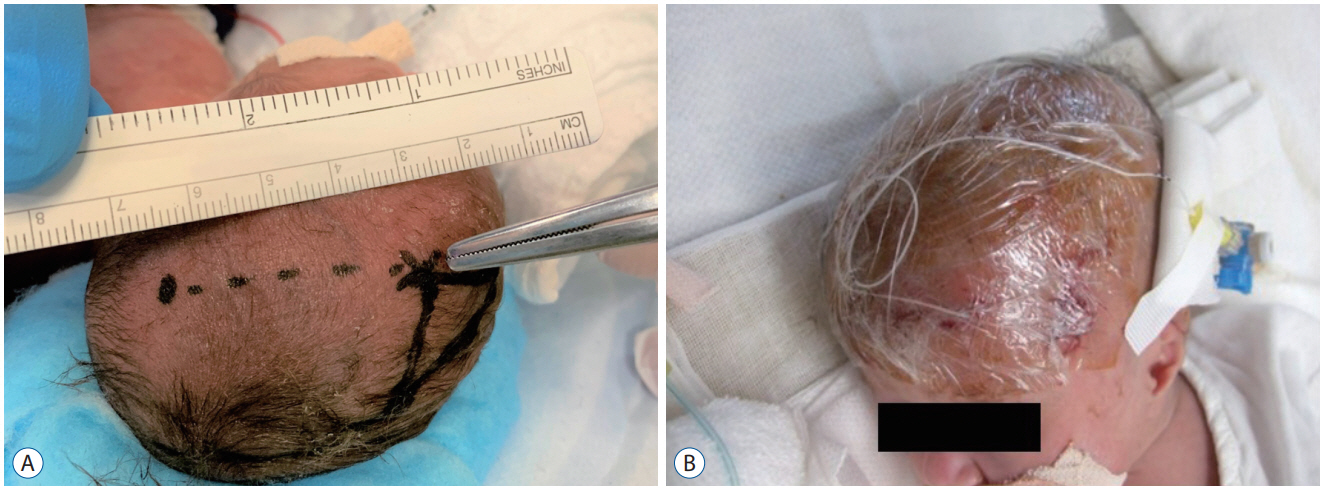
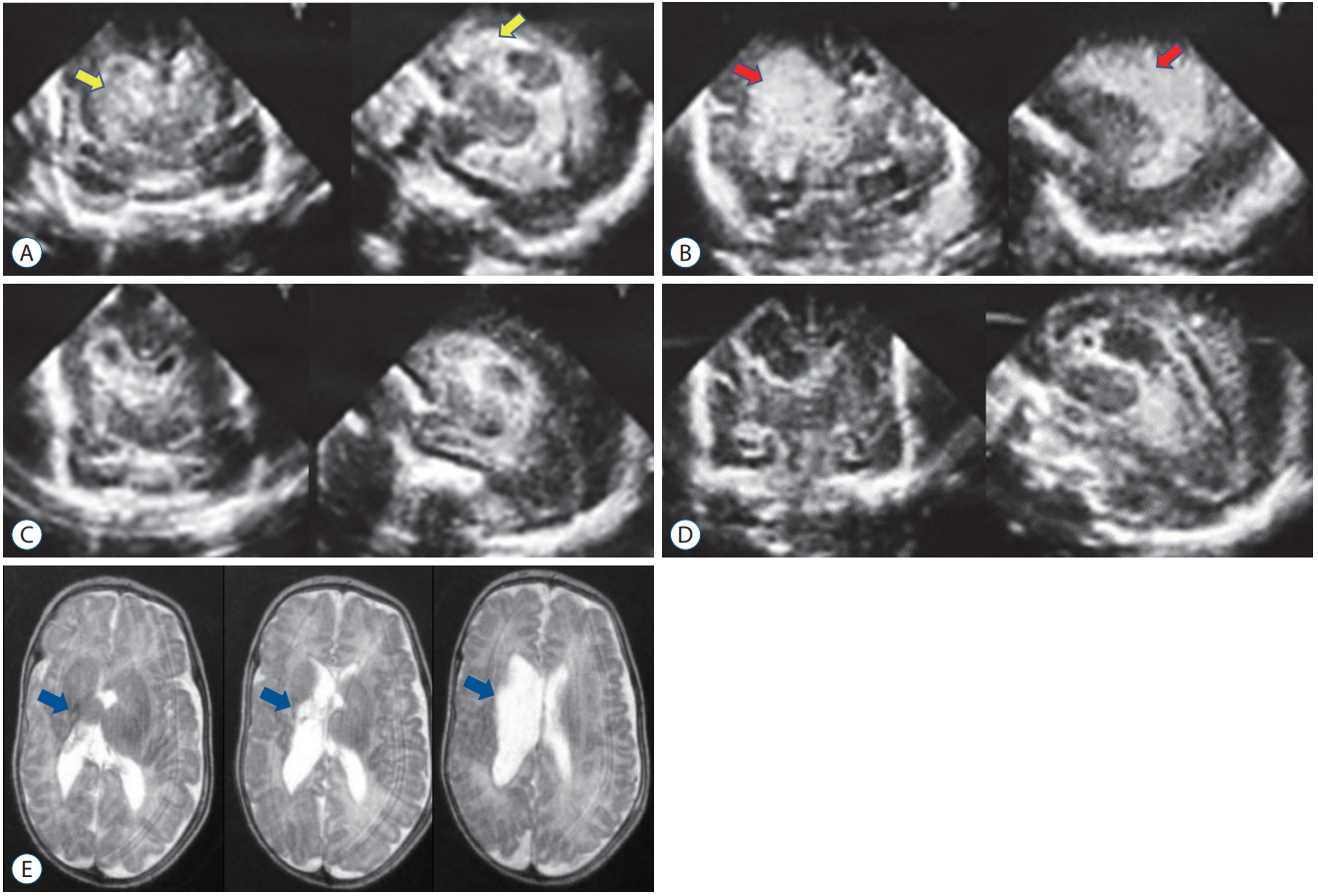
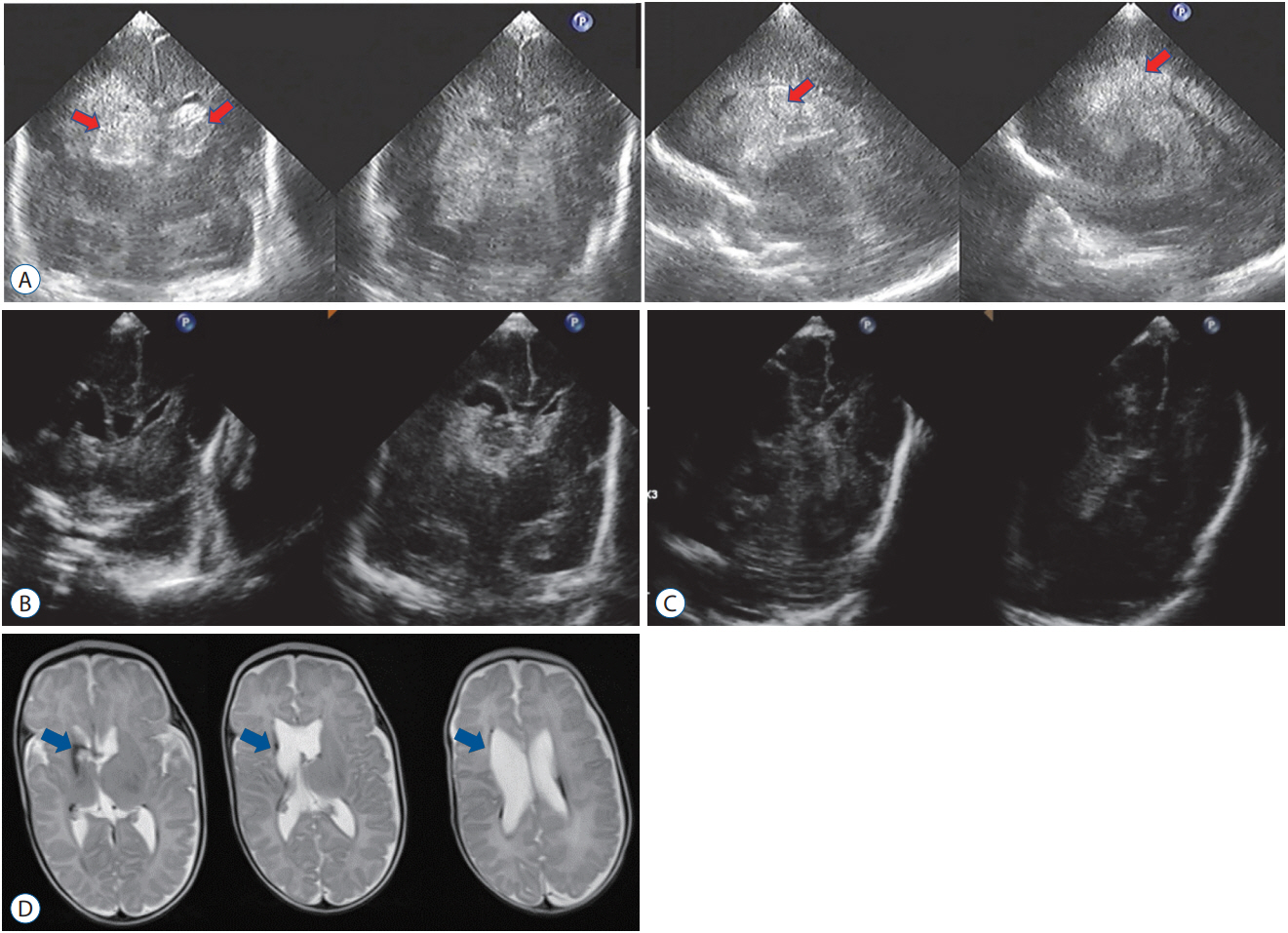
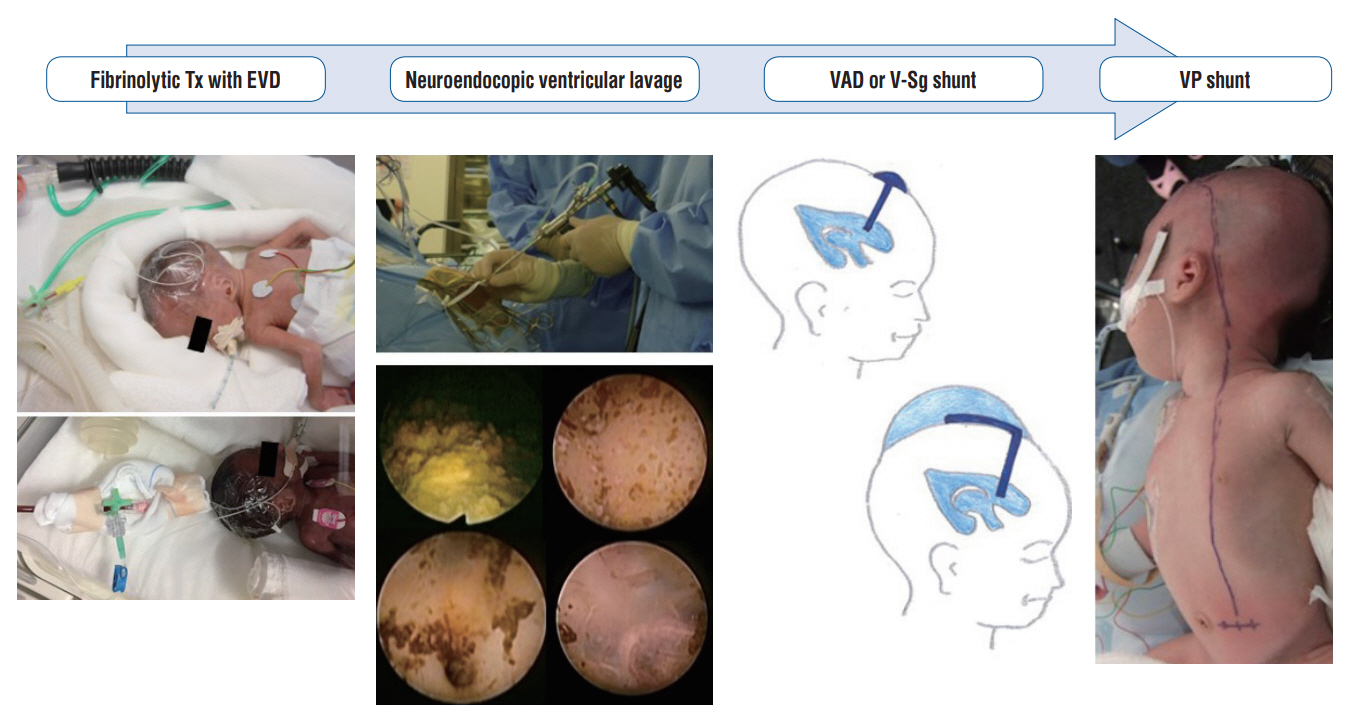
- While the survival rate of preterm infants has increased dramatically over the last few decades, intraventricular hemorrhage and subsequent hydrocephalus remain major unsolved problems in neonatal intensive care. Once intraventricular hemorrhage occurs, severe neurological sequelae are inevitable. Treatment of this complicated pathology and achievement of favorable neurofunctional outcomes in fragile infants are crucial challenges for pediatric neurosurgeons. Fibrinolytic therapy, which chemically dissolves hematoma, is a promising and useful treatment method. In this paper, the historical background of fibrinolytic therapy for postintraventricular hemorrhagic hydrocephalus in preterm infants is reviewed and a recent method of fibrinolytic therapy using urokinase is introduced.
Figure
Reference
-
References
1. Adams-Chapman I, Hansen NI, Stoll BJ, Higgins R; NICHD Research Network. Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics. 121:e1167–1177. 2008.
Article2. Akdemir H, Selçuklu A, Paşaoğlu A, Oktem IS, Kavuncu I. Treatment of severe intraventricular hemorrhage by intraventricular infusion of urokinase. Neurosurg Rev. 18:95–100. 1995.
Article3. Behrens P, Tietze A, Walch E, Bittigau P, Bührer C, Schulz M, et al. Neurodevelopmental outcome at 2 years after neuroendoscopic lavage in neonates with posthemorrhagic hydrocephalus. J Neurosurg Pediatr. 26:495–503. 2020.
Article4. Brouwer AJ, van Stam C, Uniken Venema M, Koopman C, Groenendaal F, de Vries LS. Cognitive and neurological outcome at the age of 5-8 years of preterm infants with post-hemorrhagic ventricular dilatation requiring neurosurgical intervention. Neonatology. 101:210–216. 2012.
Article5. Chari A, Mallucci C, Whitelaw A, Aquilina K. Intraventricular haemorrhage and posthaemorrhagic ventricular dilatation: moving beyond CSF diversion. Childs Nerv Syst. 37:3375–3383. 2021.
Article6. Christian EA, Jin DL, Attenello F, Wen T, Cen S, Mack WJ, et al. Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000-2010. J Neurosurg Pediatr. 17:260–269. 2016.
Article7. Cizmeci MN, Groenendaal F, Liem KD, van Haastert IC, Benavente-Fernández I, van Straaten HLM, et al. Randomized controlled early versus late ventricular intervention study in posthemorrhagic ventricular dilatation: outcome at 2 years. J Pediatr. 226:28–35.e3. 2020.8. d’Arcangues C, Schulz M, Bührer C, Thome U, Krause M, Thomale UW. Extended experience with neuroendoscopic lavage for posthemorrhagic hydrocephalus in neonates. World Neurosurg. 116:e217–e224. 2018.
Article9. Dvalishvili A, Khinikadze M, Gegia G, Khutsishvili L. Neuroendoscopic lavage versus traditional surgical methods for the early management of posthemorrhagic hydrocephalus in neonates. Childs Nerv Syst. 38:1897–1902. 2022.
Article10. El-Dib M, Limbrick DD Jr, Inder T, Whitelaw A, Kulkarni AV, Warf B, et al. Management of post-hemorrhagic ventricular dilatation in the infant born preterm. J Pediatr. 226:16–27.e3. 2020.11. Etus V, Kahilogullari G, Karabagli H, Unlu A. Early endoscopic ventricular irrigation for the treatment of neonatal posthemorrhagic hydrocephalus: a feasible treatment option or not? A multicenter study. Turk Neurosurg. 28:137–141. 2018.12. Gaberel T, Montagne A, Lesept F, Gauberti M, Lemarchand E, Orset C, et al. Urokinase versus alteplase for intraventricular hemorrhage fibrinolysis. Neuropharmacology. 85:158–165. 2014.
Article13. Hansen A, Whitelaw A, Lapp C, Brugnara C. Cerebrospinal fluid plasminogen activator inhibitor-1: a prognostic factor in posthaemorrhagic hydrocephalus. Acta Paediatr. 86:995–998. 1997.
Article14. Hansen AR, Volpe JJ, Goumnerova LC, Madsen JR. Intraventricular urokinase for the treatment of posthemorrhagic hydrocephalus. Pediatr Neurol. 17:213–217. 1997.
Article15. Hirata K, Kimura T, Hirano S, Wada K, Kusuda S, Fujimura M, et al. Outcomes of outborn very-low-birth-weight infants in Japan. Arch Dis Child Fetal Neonatal Ed. 106:131–136. 2021.
Article16. Honeyman SI, Boukas A, Jayamohan J, Magdum S. Neuroendoscopic lavage for the management of neonatal post-haemorrhagic hydrocephalus: a retrospective series. Childs Nerv Syst. 38:115–121. 2022.
Article17. Hudgins RJ, Boydston WR, Hudgins PA, Morris R, Adler SM, Gilreath CL. Intrathecal urokinase as a treatment for intraventricular hemorrhage in the preterm infant. Pediatr Neurosurg. 26:281–187. 1997.
Article18. Jeon GW, Lee JH, Oh M, Chang YS. Serial long-term growth and neurodevelopment of very-low-birth-weight infants: 2022 update on the Korean neonatal network. J Korean Med Sci. 37:e263. 2022.
Article19. Kandula V, Mohammad LM, Thirunavu V, LoPresti M, Beestrum M, Lai GY, et al. The role of blood product removal in intraventricular hemorrhage of prematurity: a meta-analysis of the clinical evidence. Childs Nerv Syst. 38:239–252. 2022.
Article20. Kusuda S, Fujimura M, Sakuma I, Aotani H, Kabe K, Itani Y, et al. Morbidity and mortality of infants with very low birth weight in Japan: center variation. Pediatrics. 118:e1130–1138. 2006.
Article21. Luyt K, Jary SL, Lea CL, Young GJ, Odd DE, Miller HE, et al. Drainage, irrigation and fibrinolytic therapy (DRIFT) for posthaemorrhagic ventricular dilatation: 10-year follow-up of a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 105:466–473. 2020.
Article22. Mazzola CA, Choudhri AF, Auguste KI, Limbrick DD Jr, Rogido M, Mitchell L, et al. Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 2: management of posthemorrhagic hydrocephalus in premature infants. J Neurosurg Pediatr 14 Suppl. 1:8–23. 2014.
Article23. McClugage SG, Laskay NMB, Donahue BN, Arynchyna A, Zimmerman K, Aban IB, et al. Functional outcomes at 2 years of age following treatment for posthemorrhagic hydrocephalus of prematurity: what do we know at the time of consult? J Neurosurg Pediatr. 14:1–9. 2020.
Article24. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 92:529–534. 1978.
Article25. Park YS. Intraventricular hemorrhage in the newborn, congenital and developmental cranial anomalies. In : Alexiou G, Prodromou N, editors. Pediatric Neurosurgery for Clinicians. Cham: Springer;2022. p. 51–65.26. Park YS. Treatment strategies and challenges to avoid cerebrospinal fluid shunting for pediatric hydrocephalus. Neurol Med Chir (Tokyo). 62:416–430. 2022.
Article27. Park YS, Kotani Y, Kim TK, Yokota H, Sugimoto T, Nakagawa I, et al. Efficacy and safety of intraventricular fibrinolytic therapy for postintraventricular hemorrhagic hydrocephalus in extreme low birth weight infants: a preliminary clinical study. Childs Nerv Syst. 37:69–79. 2021.
Article28. Rainov NG, Burkert WL. Urokinase infusion for severe intraventricular haemorrhage. Acta Neurochir (Wien). 134:55–59. 1995.29. Richard E, Cinalli G, Assis D, Pierre-Kahn A, Lacaze-Masmonteil T. Treatment of post-haemorrhage ventricular dilatation with an Ommaya’s reservoir: management and outcome of 64 preterm infants. Childs Nerv Syst. 17:334–340. 2001.
Article30. Sävman K, Blennow M, Hagberg H, Tarkowski E, Thoresen M, Whitelaw A. Cytokine response in cerebrospinal fluid from preterm infants with posthaemorrhagic ventricular dilatation. Acta Paediatr. 91:1357–1363. 2002.
Article31. Savman K, Nilsson UA, Blennow M, Kjellmer I, Whitelaw A. Non-protein-bound iron is elevated in cerebrospinal fluid from preterm infants with posthemorrhagic ventricular dilatation. Pediatr Res. 49:208–212. 2001.
Article32. Schulz M, Bührer C, Pohl-Schickinger A, Haberl H, Thomale UW. Neuroendoscopic lavage for the treatment of intraventricular hemorrhage and hydrocephalus in neonates. J Neurosurg Pediatr. 13:626–635. 2014.
Article33. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 126:443–456. 2010.
Article34. Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 314:1039–1051. 2015.
Article35. Szpecht D, Wiak K, Braszak A, Szymankiewicz M, Gadzinowski J. Role of selected cytokines in the etiopathogenesis of intraventricular hemorrhage in preterm newborns. Childs Nerv Syst. 32:2097–2103. 2016.
Article36. Tirado-Caballero J, Rivero-Garvia M, Arteaga-Romero F, Herreria-Franco J, Lozano-Gonzalez Á, Marquez-Rivas J. Neuroendoscopic lavage for the management of posthemorrhagic hydrocephalus in preterm infants: safety, effectivity, and lessons learned. J Neurosurg Pediatr. 26:237–246. 2020.
Article37. Todo T, Usui M, Takakura K. Treatment of severe intraventricular hemorrhage by intraventricular infusion of urokinase. J Neurosurg. 74:81–86. 1991.
Article38. Volpe JJ. Intraventricular hemorrhage in the premature infant--current concepts. Part I. Ann Neurol. 25:3–11. 1989.
Article39. Volpe JJ. Intraventricular hemorrhage in the premature infant--current concepts. Part II. Ann Neurol. 25:109–116. 1989.
Article40. Whitelaw A, Aquilina K. Management of posthaemorrhagic ventricular dilatation. Arch Dis Child Fetal Neonatal Ed. 97:F229–F233. 2012.
Article41. Whitelaw A, Evans D, Carter M, Thoresen M, Wroblewska J, Mandera M, et al. Randomized clinical trial of prevention of hydrocephalus after intraventricular hemorrhage in preterm infants: brain-washing versus tapping fluid. Pediatrics. 119:e1071–e1078. 2007.
Article42. Whitelaw A, Jary S, Kmita G, Wroblewska J, Musialik-Swietlinska E, Mandera M, et al. Randomized trial of drainage, irrigation and fibrinolytic therapy for premature infants with posthemorrhagic ventricular dilatation: developmental outcome at 2 years. Pediatrics. 125:e852–e858. 2010.
Article43. Whitelaw A, Mowinckel MC, Abildgaard U. Low levels of plasminogen in cerebrospinal fluid after intraventricular haemorrhage: a limiting factor for clot lysis? Acta Paediatr. 84:933–936. 1995.
Article44. Whitelaw A, Mowinckel MC, Fellman V, Abildgaard U. Endogenous tissue plasminogen activator in neonatal cerebrospinal fluid. Eur J Pediatr. 155:117–119. 1996.
Article45. Whitelaw A, Pople I, Cherian S, Evans D, Thoresen M. Phase 1 trial of prevention of hydrocephalus after intraventricular hemorrhage in newborn infants by drainage, irrigation, and fibrinolytic therapy. Pediatrics. 111(4 Pt 1):759–765. 2003.
Article46. Whitelaw A, Rivers RP, Creighton L, Gaffney P. Low dose intraventricular fibrinolytic treatment to prevent posthaemorrhagic hydrocephalus. Arch Dis Child. 67(1 Spec No):12–14. 1992.
Article47. Whitelaw A, Saliba E, Fellman V, Mowinckel MC, Acolet D, Marlow N. Phase I study of intraventricular recombinant tissue plasminogen activator for treatment of posthaemorrhagic hydrocephalus. Arch Dis Child Fetal Neonatal Ed. 75:F20–F26. 1996.
Article48. Wilson-Costello D, Friedman H, Minich N, Siner B, Taylor G, Schluchter M, et al. Improved neurodevelopmental outcomes for extremely low birth weight infants in 2000-2002. Pediatrics. 119:37–45. 2007.
Article49. Yapicioğlu H, Narli N, Satar M, Soyupak S, Altunbaşak S. Intraventricular streptokinase for the treatment of posthaemorrhagic hydrocephalus of preterm. J Clin Neurosci. 10:297–299. 2003.
Article50. Youn Y, Lee SM, Hwang JH, Cho SJ, Kim EK, Kim EA, et al. Two-year outcomes of Korean very low birth weight infants born in 2013-2014. J Korean Med Sci. 33:e309. 2018.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of congenital hydrocephalus associated with fetal intraventricular hemorrhage
- Clinical Feature and General Management of Post-Hemorrhagic Hydrocephalus in Premature Infants
- Enoxaparin Therapy for Arterial Thrombosis After Umbilical Cord Catheterization in Preterm Infants
- Temporary Surgical Management of Intraventricular Hemorrhage in Premature Infants
- Current Status and Associated Factors of Post-Hemorrhagic Hydrocephalus in Infants of 22 to 28 Weeks Gestation With Severe Intraventricular Hemorrhage in Korea: A Nationwide Cohort Study