Cancer Res Treat.
2023 Apr;55(2):652-658. 10.4143/crt.2022.893.
A Nationwide Study of Differences in Surgical Treatment Rates and Oncological Outcomes for Prostate Cancer according to Economic Status and Region
- Affiliations
-
- 1Department of Urology, SMG-SNU Boramae Medical Center, Seoul, Korea
- 2Department of Biostatistics, SMG-SNU Boramae Medical Center, Seoul, Korea
- KMID: 2541252
- DOI: http://doi.org/10.4143/crt.2022.893
Abstract
- Purpose
We investigated the effects of economic status (classified based on insurance type and residential area) on oncological outcomes of prostate cancer using a nationwide database. We additionally investigated oncological outcomes based on economic status and residential area in patients who underwent surgical treatment.
Materials and Methods
The study included 75,518 men with newly diagnosed prostate cancer between 2009 and 2018 in whom oncological outcomes were investigated based on economic status and residential area. Among the 75,518 men with prostate cancer, the data of 29,973 men who underwent radical prostatectomy were further analyzed. Multivariate analysis was performed to determine the effects of economic status and residential area on postoperative oncological outcomes.
Results
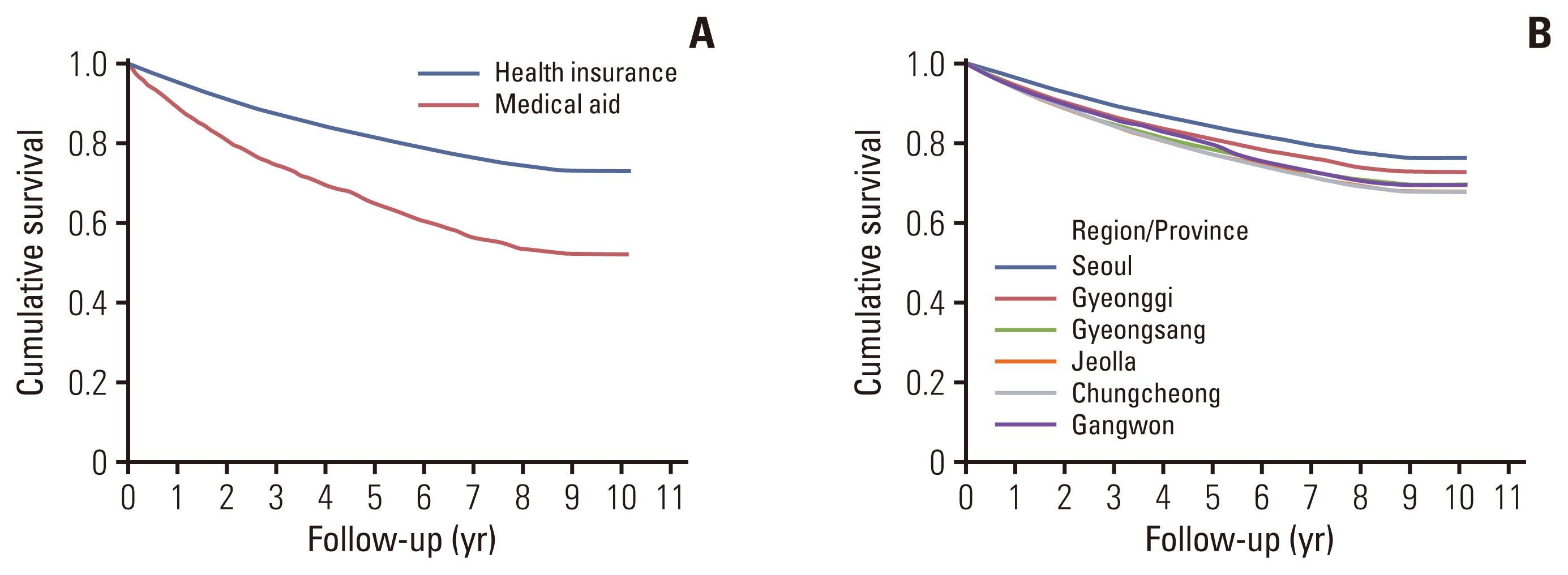
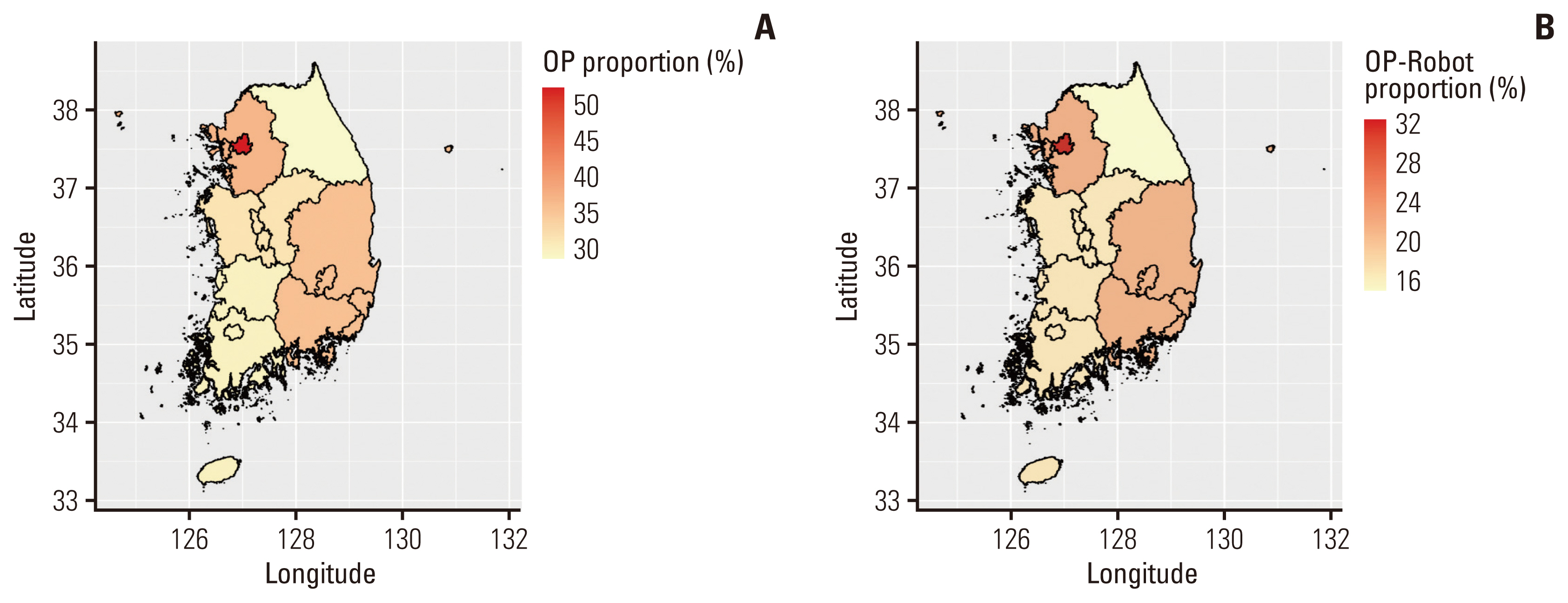
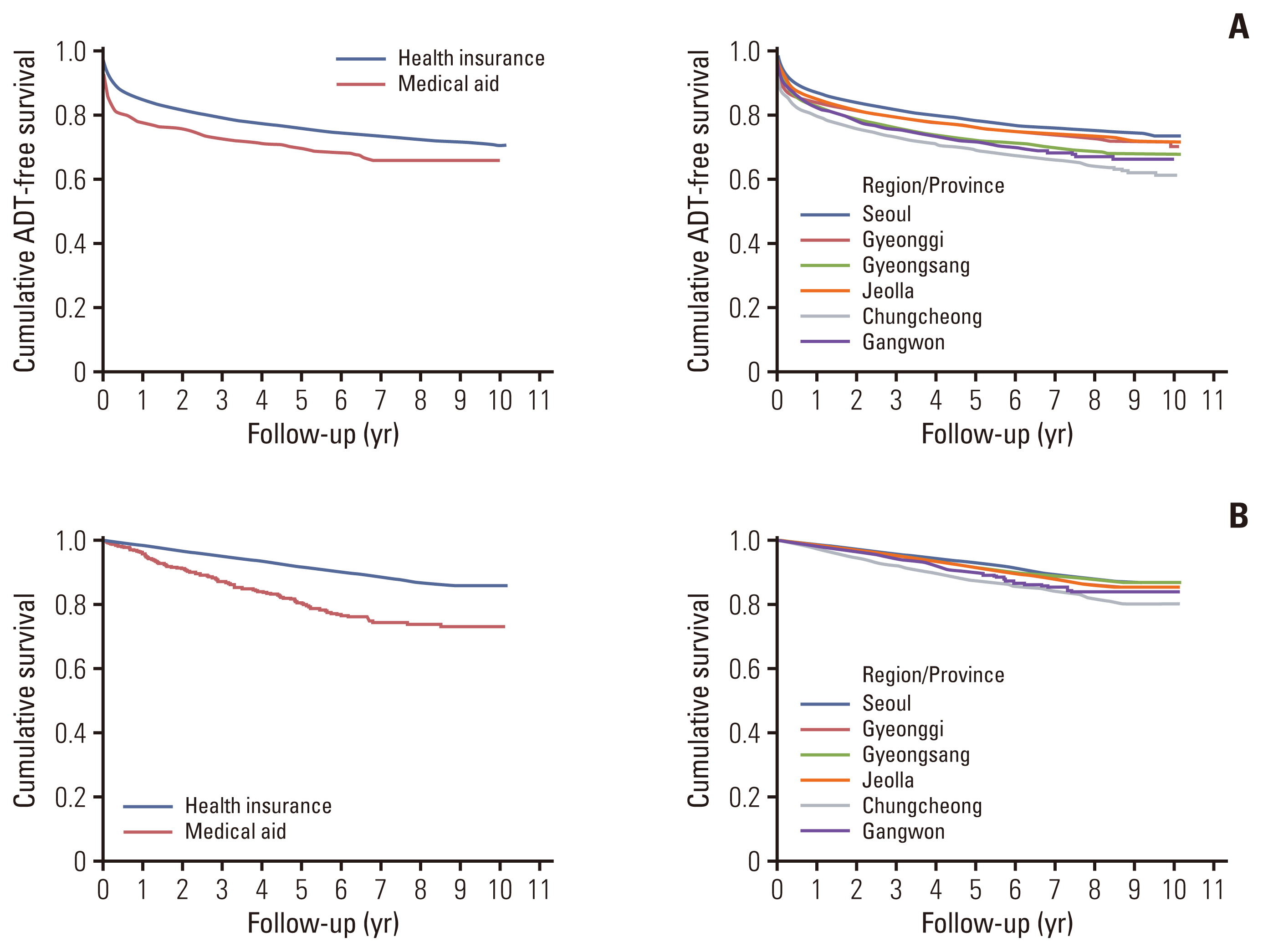
Among the 75,518 patients with prostate cancer, 3,254 (4.31%) were medical aid beneficiaries. The 5-year overall survival rates were 81.2% and 64.8% in the health insurance and medical aid groups, respectively. Radical prostatectomy was more common in the health insurance group, and surgical intervention was significantly affected by the residential area. Among patients who underwent surgery, 5-year androgen deprivation therapy–free and overall survival were better in the health insurance group. Multivariate analysis showed that insurance type and residential area were significantly associated with the androgen deprivation therapy–free and overall survival after adjustment for other variables.
Conclusion
Economic status and residential area were shown to affect not only treatment patterns but also post-diagnosis and postoperative oncological outcomes. Political support for early diagnosis and appropriate treatment of prostate cancer is warranted for medically vulnerable populations.
Keyword
Figure
Reference
-
References
1. Rawla P. Epidemiology of prostate cancer. World J Oncol. 2019; 10:63–89.
Article2. Brawley OW. Trends in prostate cancer in the United States. J Natl Cancer Inst Monogr. 2012; 2012:152–6.
Article3. Jung KW, Won YJ, Hong S, Kong HJ, Im JS, Seo HG. Prediction of cancer incidence and mortality in Korea, 2021. Cancer Res Treat. 2021; 53:316–22.
Article4. Moyer VA; US. Preventive Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012; 157:120–34.
Article5. Fleshner K, Carlsson SV, Roobol MJ. The effect of the USPSTF PSA screening recommendation on prostate cancer incidence patterns in the USA. Nat Rev Urol. 2017; 14:26–37.
Article6. Bibbins-Domingo K, Grossman DC, Curry SJ. The US Preventive Services Task Force 2017 draft recommendation statement on screening for prostate cancer: an invitation to review and comment. JAMA. 2017; 317:1949–50.
Article7. Hong S, Won YJ, Park YR, Jung KW, Kong HJ, Lee ES, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2017. Cancer Res Treat. 2020; 52:335–50.
Article8. Baldwin LM, Andrilla CH, Porter MP, Rosenblatt RA, Patel S, Doescher MP. Treatment of early-stage prostate cancer among rural and urban patients. Cancer. 2013; 119:3067–75.
Article9. Gray PJ, Lin CC, Cooperberg MR, Jemal A, Efstathiou JA. Temporal trends and the impact of race, insurance, and socioeconomic status in the management of localized prostate cancer. Eur Urol. 2017; 71:729–37.
Article10. Xia L, Talwar R, Chelluri RR, Guzzo TJ, Lee DJ. Surgical delay and pathological outcomes for clinically localized high-risk prostate cancer. JAMA Netw Open. 2020; 3:e2028320.
Article11. Yoo S, Oh S, Park J, Cho SY, Cho MC, Jeong H, et al. The impacts of metabolic syndrome and lifestyle on the prevalence of benign prostatic hyperplasia requiring treatment: historical cohort study of 130 454 men. BJU Int. 2019; 123:140–8.
Article12. Park J, Suh B, Shin DW, Hong JH, Ahn H. Changing patterns of primary treatment in Korean men with prostate cancer over 10 years: a nationwide population based study. Cancer Res Treat. 2016; 48:899–906.
Article13. Lee SY, Jung KY, Lee IK, Yi SD, Cho YW, Kim DW, et al. Prevalence of treated epilepsy in Korea based on national health insurance data. J Korean Med Sci. 2012; 27:285–90.
Article14. Johansson JE, Holmberg L, Johansson S, Bergstrom R, Adami HO. Fifteen-year survival in prostate cancer. A prospective, population-based study in Sweden. JAMA. 1997; 277:467–71.
Article15. Cuzick J, Thorat MA, Andriole G, Brawley OW, Brown PH, Culig Z, et al. Prevention and early detection of prostate cancer. Lancet Oncol. 2014; 15:e484–92.
Article16. Van Poppel H, Roobol MJ, Chapple CR, Catto JW, N’Dow J, Sonksen J, et al. Prostate-specific antigen testing as part of a risk-adapted early detection strategy for prostate cancer: European Association of Urology position and recommendations for 2021. Eur Urol. 2021; 80:703–11.
Article17. Rapiti E, Fioretta G, Schaffar R, Neyroud-Caspar I, Verkooijen HM, Schmidlin F, et al. Impact of socioeconomic status on prostate cancer diagnosis, treatment, and prognosis. Cancer. 2009; 115:5556–65.
Article18. Aarts MJ, Koldewijn EL, Poortmans PM, Coebergh JW, Louwman M. The impact of socioeconomic status on prostate cancer treatment and survival in the southern Netherlands. Urology. 2013; 81:593–9.
Article19. Lee DH, Jung HB, Chung MS, Lee SH, Chung BH. The change of prostate cancer treatment in Korea: 5 year analysis of a single institution. Yonsei Med J. 2013; 54:87–91.
Article20. Mottet N, van den Bergh RC, Briers E, Van den Broeck T, Cumberbatch MG, De Santis M, et al. EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer-2020 update. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2021; 79:243–62.21. Roehrborn CG, Albertsen P, Stokes ME, Black L, Benedict A. First-year costs of treating prostate cancer: estimates from SEER-Medicare data. Prostate Cancer Prostatic Dis. 2009; 12:355–60.
Article22. Jemal A, Ward E, Wu X, Martin HJ, McLaughlin CC, Thun MJ. Geographic patterns of prostate cancer mortality and variations in access to medical care in the United States. Cancer Epidemiol Biomarkers Prev. 2005; 14:590–5.
Article23. Afshar N, English DR, Milne RL. Rural-urban residence and cancer survival in high-income countries: a systematic review. Cancer. 2019; 125:2172–84.
Article24. Arcury TA, Gesler WM, Preisser JS, Sherman J, Spencer J, Perin J. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res. 2005; 40:135–55.
Article25. Cary C, Odisho AY, Cooperberg MR. Variation in prostate cancer treatment associated with population density of the county of residence. Prostate Cancer Prostatic Dis. 2016; 19:174–9.
Article26. Lee J. Health inequality in health checkups. Korean J Fam Med. 2018; 39:65–6.
Article27. Unger JM, Moseley A, Symington B, Chavez-MacGregor M, Ramsey SD, Hershman DL. Geographic distribution and survival outcomes for rural ppatients with cancer treated in clinical trials. JAMA Netw Open. 2018; 1:e181235.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radical Prostatectomy: Respective Roles and Comparisons of Robotic and Open Surgeries
- Racial Differences in Prostate Cancer Characteristics and Cancer-Specific Mortality: An Overview
- Intersphincteric Resection for Patients With Low-Lying Rectal Cancer: Oncological and Functional Outcomes
- Comparison of the oncological outcomes of stenting as a bridge to surgery and surgery alone in stages II to III obstructive colorectal cancer: a retrospective study
- Robotic Intersphincteric Resection for Low Rectal Cancer: Technical Controversies and a Systematic Review on the Perioperative, Oncological, and Functional Outcomes