Kosin Med J.
2023 Mar;38(1):21-27. 10.7180/kmj.22.131.
Remote health monitoring services in nursing homes
- Affiliations
-
- 1Department of Internal Medicine, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- 2Department of Chest Surgery, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- 3Geriatric and Extended Care Service, Department of Veterans Affairs Greater Los Angeles Healthcare System, and Department of Medicine, David Geffen School of Medicine at University of California at Los Angeles, Los Angeles, CA, USA
- KMID: 2540758
- DOI: http://doi.org/10.7180/kmj.22.131
Abstract
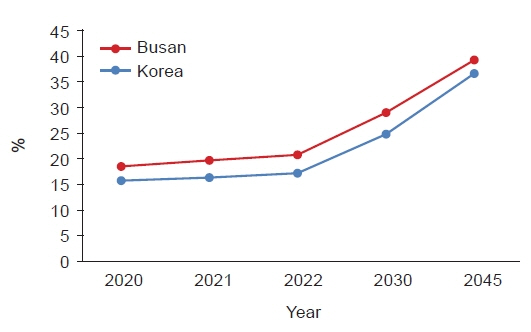
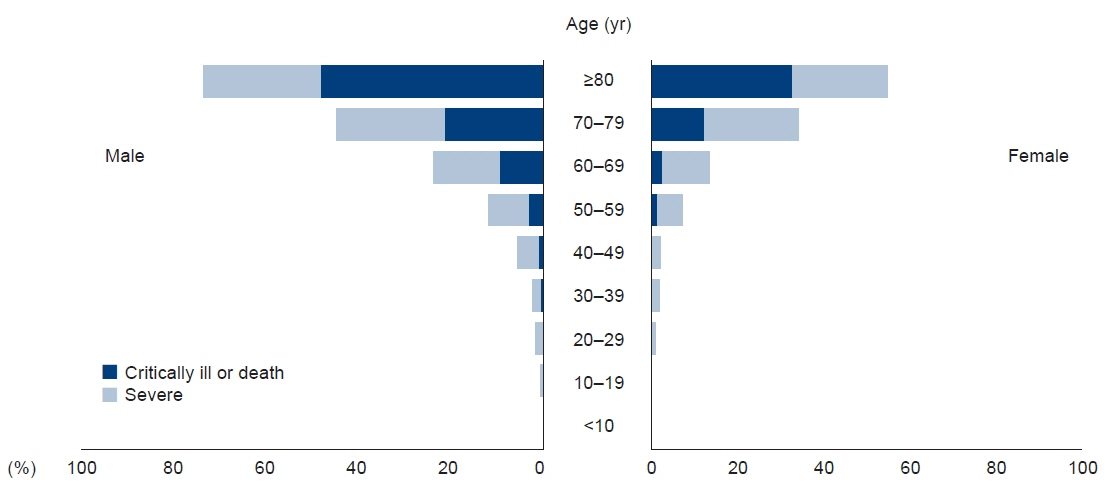
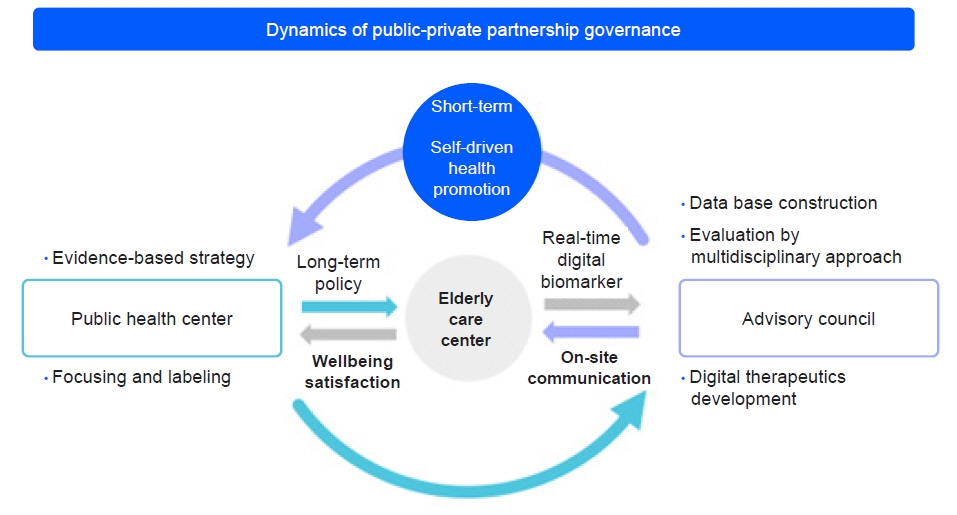
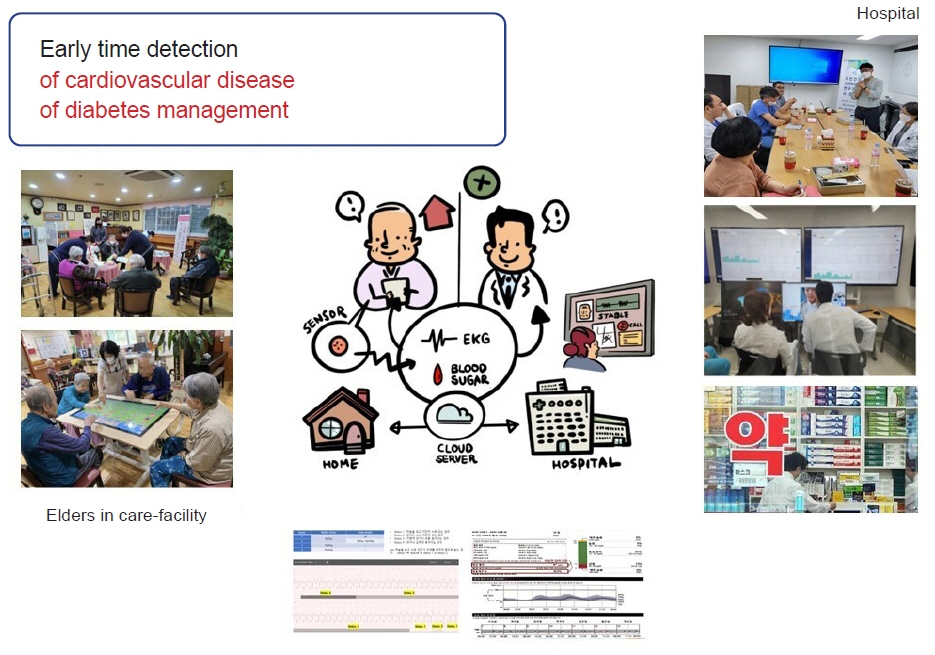
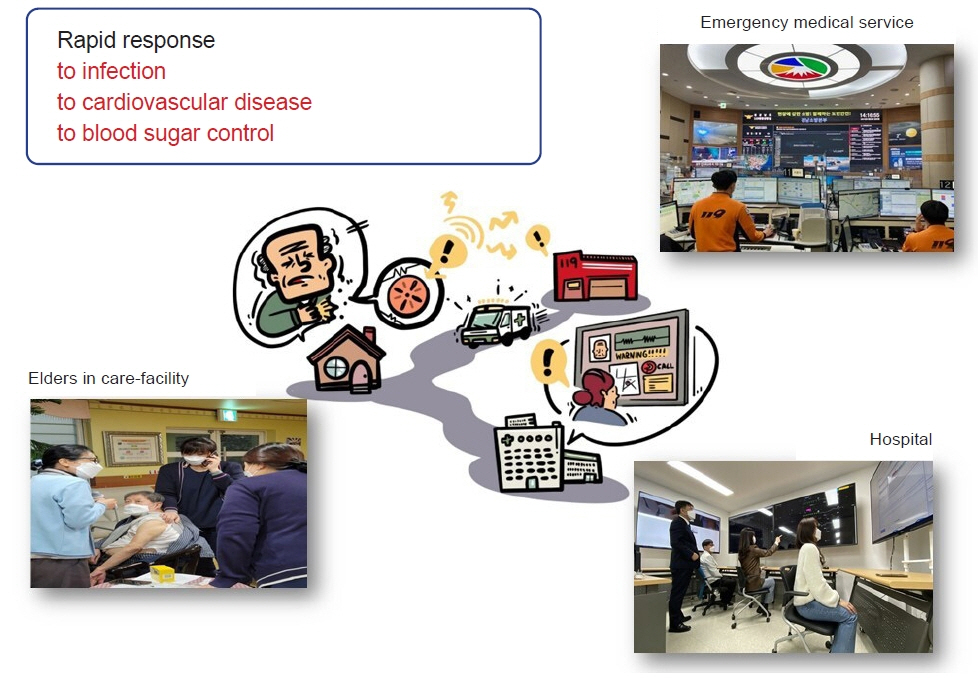
- Aged people are challenged by serious complications from chronic diseases, such as mood disorder, diabetes, heart disease, and infectious diseases, which are also the most common causes of death in older people. Therefore, elderly care facilities are more important than ever. The most common causes of death in elderly care facilities were reported to be diabetes, cardiovascular disease, and pneumonia. Recently, the coronavirus disease 2019 (COVID-19) pandemic have a great impact on blind spots of safety where aged people were isolated from society. Elderly care facilities were one of the blind spots in the midst of the pandemic, where major casualties were reported from COVID-19 complications because most people had one or two mortality risk factors, such as diabetes or cardiovascular disease. Therefore, medical governance of public health center and hospital, and elderly care facility is becoming important issue of priority. Thus, remote health monitoring service by the Internet of Medical Things (IoMT) sensors is more important than ever. Recently, technological breakthroughs have enabled healthcare professionals to have easy access to patients in medical blind spots through the use of IoT sensors. These sensors can detect medically urgent situations in a timely fashion and make medical decisions for aged people in elderly care facilities. Real-time electrocardiograms and blood sugar monitoring sensors are approved by the medical insurance service. Real-time monitoring services in medical blind spots, such as elderly care facilities, has been suggested. Heart rhythm monitoring could play a role in detecting early cardiovascular disease events and monitoring blood glucose levels in the management of chronic diseases, such as diabetes, in aged people in elderly care facilities. This review presents the potential usefulness of remote monitoring with IoMT sensors in medical blind spots and clinical suggestions for applications.
Figure
Reference
-
References
1. Ministry of Health and Welfare. 2020 National Survey of the Living Conditions and Welfare Needs of Older Koreans. Ministry of Health and Welfare; 2021.2. Park HY, Lee JH, Lim NK, Lim DS, Hong SO, Park MJ, et al. Presenting characteristics and clinical outcome of patients with COVID-19 in South Korea: a nationwide retrospective observational study. Lancet Reg Health West Pac. 2020; 5:100061.3. Koff WC, Williams MA. COVID-19 and immunity in aging populations: a new research agenda. N Engl J Med. 2020; 383:804–5.4. Tsang JS, Dobano C, VanDamme P, Moncunill G, Marchant A, Othman RB, et al. Improving vaccine-induced immunity: can baseline predict outcome? Trends Immunol. 2020; 41:457–65.5. Barbera JA, Macintyre AG. Medical surge capacity and capability: a management system for integrating medical and health resources during large-scale emergencies. US Department of Health and Human Services; 2007.6. Klimova B. Mobile health devices for aging population groups: a review study. In : Younas M, Awan I, Kryvinska N, Strauss C, Thanh D, editors. Mobile Web and Intelligent Information Systems. Lecture Notes in Computer Science;2016. p. 295–301.7. Chung YF, Liu CH. Design of a wireless sensor network platform for tele-homecare. Sensors (Basel). 2013; 13:17156–75.8. Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020; 382:1679–81.9. Salman OH, Rasid MF, Saripan MI, Subramaniam SK. Multi-sources data fusion framework for remote triage prioritization in telehealth. J Med Syst. 2014; 38:103.10. Mat Kiah ML, Al-Bakri SH, Zaidan AA, Zaidan BB, Hussain M. Design and develop a video conferencing framework for real-time telemedicine applications using secure group-based communication architecture. J Med Syst. 2014; 38:133.11. Damiano ER, McKeon K, El-Khatib FH, Zheng H, Nathan DM, Russell SJ. A comparative effectiveness analysis of three continuous glucose monitors: the Navigator, G4 Platinum, and Enlite. J Diabetes Sci Technol. 2014; 8:699–708.12. Pleus S, Schoemaker M, Morgenstern K, Schmelzeisen-Redeker G, Haug C, Link M, et al. Rate-of-change dependence of the performance of two CGM systems during induced glucose swings. J Diabetes Sci Technol. 2015; 9:801–7.13. Gliner V, Keidar N, Makarov V, Avetisyan AI, Schuster A, Yaniv Y. Automatic classification of healthy and disease conditions from images or digital standard 12-lead electrocardiograms. Sci Rep. 2020; 10:16331.14. De Ridder B, Van Rompaey B, Kampen JK, Haine S, Dilles T. Smartphone apps using photoplethysmography for heart rate monitoring: meta-analysis. JMIR Cardio. 2018; 2:e4.15. Garcia JS, Alonso SG, de la Torre Diez I, Garcia-Zapirain B, Castillo C, Coronado ML, et al. Reviewing mobile apps to control heart rate in literature and virtual stores. J Med Syst. 2019; 43:80.16. Ilbeigipour S, Albadvi A, Akhondzadeh Noughabi E. Real-time heart arrhythmia detection using Apache Spark Structured Streaming. J Healthc Eng. 2021; 2021:6624829.17. Eisenhuber E, Schaefer-Prokop CM, Prosch H, Schima W. Bedside chest radiography. Respir Care. 2012; 57:427–43.18. Mentrup D, Jockel S, Menser B, Neitzel U. Iterative scatter correction for grid-less bedside chest radiography: performance for a chest phantom. Radiat Prot Dosimetry. 2016; 169:308–12.19. Mjolstad OC, Dalen H, Graven T, Kleinau JO, Salvesen O, Haugen BO. Routinely adding ultrasound examinations by pocket-sized ultrasound devices improves inpatient diagnostics in a medical department. Eur J Intern Med. 2012; 23:185–91.20. Mulvagh SL, Bhagra A, Nelson BP, Narula J. Handheld ultrasound devices and the training conundrum: how to get to “seeing is believing”. J Am Soc Echocardiogr. 2014; 27:310–3.21. Polonsky WH, Fisher L, Schikman CH, Hinnen DA, Parkin CG, Jelsovsky Z, et al. Structured self-monitoring of blood glucose significantly reduces A1C levels in poorly controlled, noninsulin-treated type 2 diabetes: results from the Structured Testing Program study. Diabetes Care. 2011; 34:262–7.22. Duran A, Martin P, Runkle I, Perez N, Abad R, Fernandez M, et al. Benefits of self-monitoring blood glucose in the management of new-onset type 2 diabetes mellitus: the St Carlos Study, a prospective randomized clinic-based interventional study with parallel groups. J Diabetes. 2010; 2:203–11.23. Pimazoni-Netto A, Rodbard D, Zanella MT; Diabetes Education and Control Group. Rapid improvement of glycemic control in type 2 diabetes using weekly intensive multifactorial interventions: structured glucose monitoring, patient education, and adjustment of therapy-a randomized controlled trial. Diabetes Technol Ther. 2011; 13:997–1004.24. Lee JW, Kim NK, Park HJ, Lee JY, Choi SY, Lee EM, et al. Obesity and insulin resistance according to age in newly diagnosed type 2 diabetes patients in Korea. Kosin Med J. 2016; 31:157–66.25. Kim KH, Kim YH, Seo KW, Yoon KY, Shin YM, Choi YS, et al. Immediate changes of glucose metabolism after gastretomy for early gastric cancer in patients with type 2 diabetes. Kosin Med J. 2021; 36:25–33.26. Lion KC, Brown JC, Ebel BE, Klein EJ, Strelitz B, Gutman CK, et al. Effect of telephone vs video interpretation on parent comprehension, communication, and utilization in the pediatric emergency department: a randomized clinical trial. JAMA Pediatr. 2015; 169:1117–25.27. Voils CI, Venne VL, Weidenbacher H, Sperber N, Datta S. Comparison of telephone and televideo modes for delivery of genetic counseling: a randomized trial. J Genet Couns. 2018; 27:339–48.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development and Application of Nursing Service Quality Indicators in Nursing Homes
- Assessment of Long-Term Care Service Needs in the Baby Boom Generation
- Current Status and Barriers to Health Care Services for Nursing Home Residents: Perspectives of Staffs in Korean Nursing Homes
- Structural Factors Influencing the Quality Management Activities in Nursing Homes
- Preliminary Development of Humanistic Care Indicators for Residents in Nursing Homes: A Delphi Technique